16 June 2020: Original Paper
Minimally Invasive Surgery Is Feasible in Patients with Liver and Kidney Transplantation
Da Wen Hsu12BCDF, Chun Ming Chang23BCDF, Chun Shuo Hsu24BCD, Wen Yao Yin12ABCDEFG*DOI: 10.12659/AOT.922602
Ann Transplant 2020; 25:e922602
Abstract
BACKGROUND: Minimally invasive surgery (MIS) has rapidly advanced, but its use in transplant patients has lagged. We share our experience of MIS for patients after kidney and liver transplantation and compare our results with similar studies in the literature.
MATERIAL AND METHODS: This study included 14 MIS (12 laparoscopic, 2 transvaginal) procedures for 13 transplant cases (6 liver and 7 kidney) done from May 2006 to May 2018. Gastrointestinal surgery was performed in 6 cases: appendectomy performed 8 months after liver transplant and 16 months after kidney transplant in 2 cases, radical right hemi-colectomy performed 6 weeks after liver transplant in 1 case; exploration for chylous ascites 6 months after liver transplant in 1 case, sleeve gastrectomy performed 3 years after kidney transplant in 1 case, and partial hepatectomy performed 12 years after kidney transplant in 1 case. For urological problems, 2 patients received ipsilateral right-side nephroureterectomy performed 10 and 12 years after kidney transplant, and 1 patient received contralateral left-side nephroureterectomy performed 12 years after kidney transplant. The 2 liver transplant patients with huge incisional hernias received repair approximately 3 and 2 years after liver transplant. Three patients underwent gynecological surgery: 2 transvaginal for pelvic floor reconstruction in 1 patient with liver transplant and 1 hysterectomy in a kidney transplant patient, and 1 laparoscopic-assisted hysterectomy in a kidney transplant patient. We retrospectively analyzed the clinical presentation, operative findings, operation time, postoperative complications, and length of stay.
RESULTS: The postoperative course was uneventful, with early resumption of oral intake, including immunosuppressants administered the same as in the non-transplant patients. All surgical procedures in these transplant patients were achieved without conversion, showed stable kidney and liver function, had better surgical outcomes in comparison with traditional surgery, and most of them were discharged within 1 week.
CONCLUSIONS: Laparoscopic and non-laparoscopic MIS surgery are feasible and safe for abdominal organ transplant patients and are helpful for timely intervention in cases with acute abdomen. No adjustment of immunosuppressant is usually needed, as oral intake can be resumed very soon after surgery.
Keywords: Kidney Transplantation, Liver Transplantation, Surgical Procedures, Minimally Invasive, Length of Stay, Postoperative Complications, transplant recipients
Background
The rate of not only liver and kidney transplantation, but also of transplantation of other abdominal organs, like the small bowel and pancreas, is increasing worldwide. In 2008, more than 27 000 patients received solid-organ transplants in the United States alone. The survival rates for organ transplantation are also markedly improving; the 5-year survival of liver transplant patients is 79% [1], and the 10-year overall renal graft survival rate for both living and deceased-donor transplantation is approximately 55–60% compared with the 35–40% noted a decade ago [2]. The 5-year survival rate for living-donor renal transplantation patients is 91%.
Accordingly, general surgeons must pay more attention to the increasing number of patients with acute- and chronic-stage diseases requiring surgical intervention [3]. The laparoscopic approach is a new and rarely used concept in solid-organ transplantation surgery, particularly for the treatment of certain complications.
More than 2 decades ago, the laparoscopic approach was initially used for the treatment of lymphocele after kidney transplant, and it has since become a routine approach for this complication [4]. Eight of 186 kidney transplant patients developed symptomatic lymphocele at an average of 26 months (range 4–59 months) after transplantation. All successfully underwent laparoscopic drainage [5].
Abdominal surgery is frequently performed in transplant patients, and up to 10% of renal transplant patients experience a severe gastrointestinal (GI) complication within 10 years, and 24% of liver transplant patients undergo another surgical procedure within 10 years [2,6,7]. Extensive abdominal surgery, like surgery for liver transplantation, is generally considered high-risk surgery when performed using the laparoscopic approach. However, some previous studies reported the advantages of laparoscopic surgery specific to immune-suppressed patients, with fewer wound-related problems, shorter hospitalization, and earlier resumption of oral intake and oral immunosuppressants [8]. In this study, we evaluate our experience with minimally invasive surgery (MIS) for transplantation patients and compare it with reports of open surgery and MIS in the literature.
Material and Methods
PATIENTS:
We enrolled liver and kidney transplant patients who received abdominal MIS at our hospital from May 2006 to May 2018. The 14 procedures performed in 13 patients were grouped into gastrointestinal (GI), urological (URO), gynecological (GYN), and abdominal wall (AW) surgeries. All patients gave informed consent, and the study was approved by Dalin Tzu Chi General Hospital Institutional Review Board (approval numbers B10801013 and B10503008).
INCLUSION CRITERIA:
Patients who underwent liver or kidney transplantation performed by our surgical team at our hospital or other hospitals were included in this study. Most of the cases received laparoscopic technique and only 2 cases (both in the GYN group) received transvaginal uterine fixation for uterine prolapse and hysterectomy for prolapse with bleeding.
HUMAN LEUCOCYTE ANTIGEN (HLA) TYPING AND IMMUNE SUPPRESSION:
We routinely test for human leucocyte antigens (HLA): HLA-A, HLA-B, HLA-C, HLA-DR, HLA-DR, HLA-DQ, and HLA-DP. No zero mismatch or all mismatches were noted in this study, and their HLA mismatches ranged from 2 to 5. Eight out of 13 cases had at least 1 allele match in the HLA-DR locus.
All transplant patients received the same protocol perioperatively and also received maintenance immunosuppression. Basiliximab (trade name Simulect), a monoclonal antibody to the α chain (CD25) of the IL-2 receptor of T cells, was used for induction therapy, except for cases numbered as Her-2 with deceased-donor liver transplant and URO-3 with deceased-donor kidney transplant (Table 1), and a triple drug combination (tacrolimus, mycophenolate mofetil, and prednisolone) was used for short- and long-term anti-rejection regimen. Tacrolimus 0.l5 mg/kg via oral route (PO) was given l–2 h preoperatively, and methylprednisolone iv 500–1000 mg (7–10 mg/kg dry weight) was given immediately before reperfusion of the transplant organ. Postoperatively, recycling of methylprednisolone started from 200 mg a day, gradually tapering down to 20 mg a day within 1 week, then tapered slowly to 5 mg/day PO at the end of the first month. Tacrolimus (FK506) was given at the dose of 0.15–0.3 mg/kg/day PO bid with a target level of 8–12 ng/ml in the first 6 weeks, 6–10 ng/ml until 3 months, 5–8 ng/ml for 1 year, followed by 4–6 ng/ml thereafter. Mycophenolate mofetil was given 1–2 gram daily.
PATIENTS WITH GASTROINTESTINAL (GI) DISEASE:
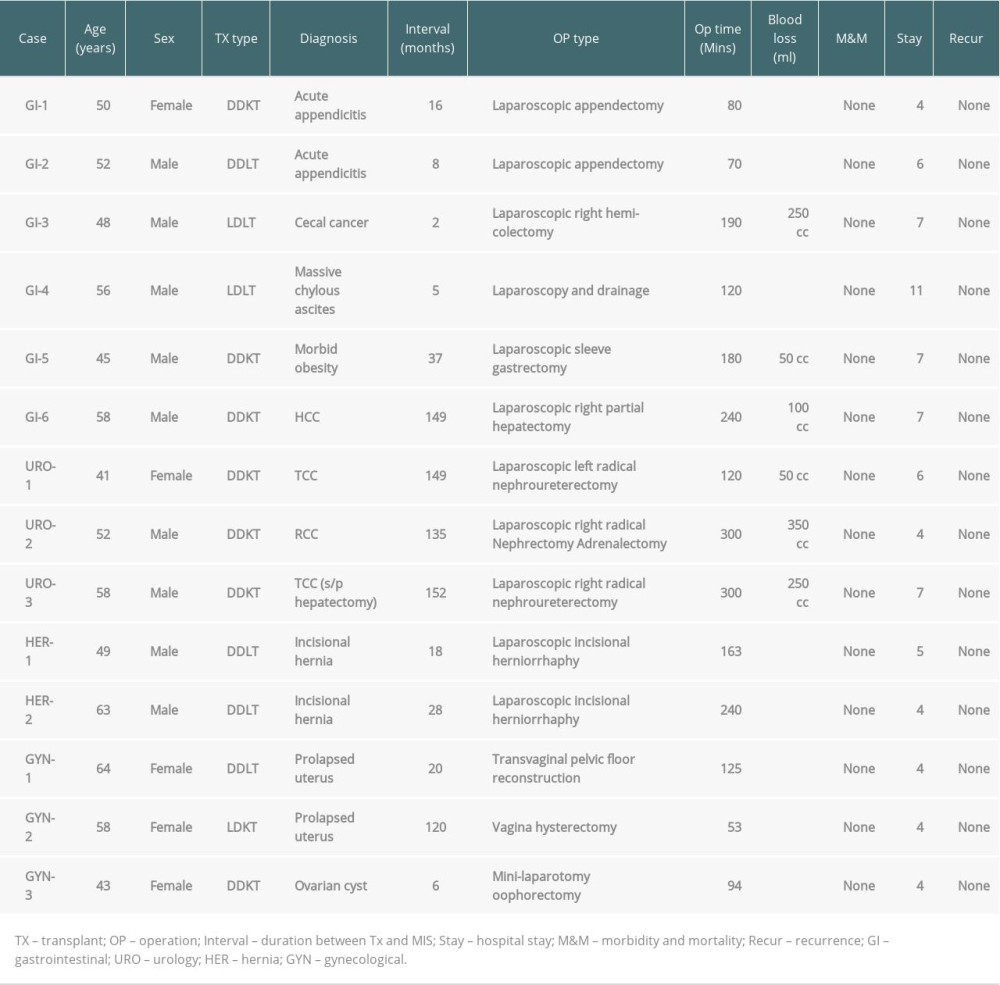
Six patients underwent laparoscopic GI surgery. Two patients, a 52-year-old man and a 50-year-old woman, underwent laparoscopic appendectomy 8 months after liver transplant for hepatitis C virus-related liver cirrhosis with end-stage liver disease (ESLD), and a 50-year-old woman (16 months after chronic renal failure with unknown cause) underwent laparoscopic appendectomy. All of them had right lower-quadrant (RLQ) pain with nausea and vomiting for 1 day. No definite history of fever was noted, but there was RLQ tenderness. A normal leukocyte count of 5456/ul (normal 3600–9600/ul) was detected in the liver transplant patient and leucocytosis 15 580/ul was detected in the kidney transplant patient. An urgent computed tomography (CT) scan showed a dilated appendix and some infiltrations around the cecum. The inflamed appendix in the kidney transplant patient was pushed anteromedially by the transplanted kidney (Figure 1) and tumor formation of acute appendicitis was noted during the operation (Figure 2). One patient underwent laparoscopic radical right hemi-colectomy 6weeks after living-donor liver transplant due to hepatitis B and C virus-related liver cirrhosis. This 48-year-old man had vague intermittent right lower-quadrant (RLQ) pain 6 weeks after transplant, and a CT scan (Figure 3) followed by colonoscopy showed cecal cancer, which was not detected before transplant. The fourth patient, a 56-year-old male with pre-transplant massive chylous ascites, received laparoscopic exploration for late-onset chylous ascites 6 months after liver transplant for end-stage liver disease (ESLD) due to HCV-related liver cirrhosis. Laparoscopic examination showed about 1000 cc of milk-like fluid (Figure 4) but no peritoneal carcinomatosis or enlarged lymph nodes. Analysis of ascites revealed a high level of triglyceride (TG: 449 mg%, normal <110 mg%) but negative for bacterial culture. A laparoscopic sleeve gastrectomy was done in a 45-year-old male with morbid obesity (body mass index >35 kg/m2 and associated metabolic diseases) (Figure 5), 3 years after kidney transplant, which occurred after right-sided radical nephrectomy for early renal cell carcinoma. A 58-year-old man underwent laparoscopic right lobectomy for hepatocellular carcinoma detected in regular follow-up 12 years after kidney transplant following renal failure of unknown cause (Figure 6).
PATIENTS WITH UROLOGICAL (URO) PROBLEMS:
Ipsilateral right-side nephroureterectomies were performed for TCC in a 58-year-old man for RCC (Figure 7) and in a 52-year-old man at 12 years and 11 years, respectively, after liver transplant. Both received renal transplant due to chronic renal failure (CRF) without specific etiology. The 58-year-old had received laparoscopic right partial hepatectomy 3 months before this operation. A laparoscopic contralateral left radical nephroureterectomy was carried out for recurrent TCC in a 41-year-old kidney transplant female patient about 13 years after transplant due to CRF with unknown cause.
PATIENTS WITH ABDOMINAL WALL (AW) HERNIA:
Two liver transplant patients with huge incisional hernias received laparoscopic hernia repair approximately 3 and 2 years after liver transplant. During laparoscopic surgery, an oval-shaped hernia defect measuring 15–20 cm in length and 10–15 cm in width (Figure 8) was detected. Dual mesh was used for hernia repair in both patients.
PATIENTS WITH GYNECOLOGICAL PROBLEMS (GYN):
Three patients underwent gynecological surgeries, with transvaginal pelvic floor reconstruction in 1 liver transplant patient, vaginal total hysterectomy in 1 kidney transplant patient, and left salpingo-oophorectomy in 1 kidney transplant patient.
A 64-year-old liver transplant patient experienced severe uterine prolapse, with her uterus hanging between her thighs. Consequently, she faced marked difficulty in sitting and walking (Figure 9). MIS with the transvaginal pelvic floor reconstruction technique was performed to lift the uterus upwards. A 58-year-old patient underwent vaginal total hysterectomy for uterine prolapse with bleeding approximately 10 years after a kidney transplant. The third case was a 43-year-old woman who underwent left adnexa resection for an ovarian cyst via mini-laparotomy 6 months after kidney transplantation.
Results
GI SURGERIES:
Both of the patients with acute appendicitis were diagnosed early, and early intervention by laparoscopic technique was done smoothly. The postoperative course was uneventful. The liver enzymes profiles 1 week after surgery were normal, with aspartate aminotransferase (AST)/alanine aminotransferase (ALT)/total bilirubin (TB) 18–22 IU/L 33–46 IU/L, and 0.8–1.0 mg%, respectively. In laparoscopic right hemi-colectomy, a moderate adhesion was noted in the whole abdomen, as usual, but there was severe tight adhesion of the raw surface of the transplanted liver and porta hepatis to the surrounding structures, including the duodenum, omentum, and hepatic flexure of the colon. A difficult dissection at the hepatic flexure was accomplished by medial-to-lateral approach, entering the retroperitoneal space, and a small part of the colon serosa strongly adhering to the liver hilum was spared to avoid injury to the liver and colon. The subserosal tumor was 3.5 cm in size, with histology of adenocarcinoma with positive lymphatic (11/15 LNs), and staging as T3N2M0 Stage IIIB.
Laparoscopy for persistent chylous ascites failed to show the leakage site, but helped to rule out other etiologies like carcinomatosis and lymphoma, as well as infections such as tuberculosis, or bowel adhesion, for which the management strategy would be different. The patient recovered following sustained and effective treatment after appropriate diagnosis. The amount of ascites drained gradually decreased and the TG level was normal in ascites. He could also tolerate an increasingly fatty diet after discharge.
For sleeve gastrectomy, there were no definite abnormal findings except for moderate-to-severe fatty liver. The excess body weight loss was more than 50%, from 138 kg before surgery to 86 kg within 6 months after the surgery. After the operation, the patient’s blood sugar was maintained in the normal range without the need for oral antihyperglycemic agents. One month after surgery, the patient had lost 13 kg and his HbA1C had decreased to 7%. One year after sleeve gastrectomy, the patient had lost 33 kg, which represented a 76% excessive body weight loss. No complications (including renal dysfunction) were noted during the 3-year follow-up.
During liver surgery for HCC, a 5-cm tumor involving segments 5, 6, and 7 on the right side of the liver was noted, and the patient received laparoscopic right lobectomy and was closely followed up.
There was no definite abnormal reaction change of liver tissue or abnormal bleeding during parenchymal transection. When the same patient underwent laparoscopic nephroureterectomy for TCC 3 months after the liver surgery, severe adhesion was noted in the subhepatic place between the right native diseased kidney and the hepatectomy area. After meticulous dissection of the diseased kidney, together with Gerota fascia, resection was completed by leaving a small part of the fascia tightly adhered to the liver surface to avoid unnecessary complications.
Regular follow-up showed no tumor recurrence for HCC and TCC by imaging study 2 years after the operation, and alfa fetoprotein (AFP) had declined from a high level of 25.63 ng/ml (normal: 10 ng/ml) to 4.38 after 1 month and 3.22 after 2 years.
URO SURGERIES:
No definite adhesion was noted between the native ureter and transplanted kidney and ureter in patients who underwent ipsilateral nephroureterectomy. All 3 patients had normal renal function, with creatinine levels of 0.8–1.2 mg% 1 month after the operation and 0.9–1.1 mg% 1 year after the operation
AW SURGERIES:
In both cases, the ventral hernias were huge with moderate adhesion to the small bowel and omentum. The hernia size noted under laparoscopy was 2–3 times the size estimated preoperatively by palpation. There was no definite liver dysfunction, with normal liver enzymes level GOT/GPT/TB: 29 IU/L/60 IU/L/1.0 mg% 1 month after surgery. A follow-up examination, even with CT, after 2 years showed no recurrence
GYN SURGERIES:
A deceased-donor LT patient with massive uterine procidentia recovered smoothly after the lifting procedure and could enjoy her normal life. Two other patients undergoing hysterectomy also recovered from the frequency of urination and uterine bleeding. None of the patients had any complications, with normal liver and kidney function GOT/GPT/TB: 33 IU/L/56 IU/L/1.0 mg% for liver and Cr 1.2 mg% for kidney transplant patients.
The postoperative course of all patients in this series was uneventful, with early bowel movement noted, usually on postoperative day (POD) 1 or 2. All patients continued oral intake, including IMS on the day after bowel movement was resumed, even in patients with upper and lower GI surgery. No significant modulation of IMS was needed in the perioperative period. All patients showed stable kidney and liver function, without any rejection episodes, and were discharged within 3 days to 1 week after any variant operation. All patients were followed up for a minimum of 2 years, except for the patient with uterine prolapse with bleeding for 7 months. Recurrence of HCC, RCC, TCC, or any other disease was not reported in any of the patients. The demographics, clinical course, and outcomes are summarized in Table 1.
Discussion
Many previous reports emphasized the tendency of delayed diagnoses, misdiagnoses, and operation for complicated acute appendicitis, instead of early simple appendicitis, with poor outcomes [8]. It was probably due to the unusual clinical features, additional differential diagnosis related to the newly implanted renal graft especially on the right side, and delayed surgical intervention. Laparoscopic technique, if available, can allow us to perform therapeutic interventions early during the disease course to prevent such unfavorable outcomes. This was corroborated by the findings in our patients with acute appendicitis, who recovered uneventfully after early intervention. Without intention to use laparoscopic technique, even using reliable diagnosis by Alvarado score in transplant patients, the surgeon may encounter complicated appendicitis (perforated appendicitis, 2 out of 11 cases) at the time of surgical intervention [9].
Laparoscopic cholecystectomy is also performed with no special difficulty for patients with simple cholecystitis [10,11]; however, the procedure is extremely difficult to perform for transplant patients with complicated cholecystitis [1]. The conversion rate to open surgery was quite high, with 32.3% (10 patients), and the average serum creatinine level 1 year after cholecystectomy was not different. One patient required temporary dialysis and 1 graft was lost [12].
Generally, when laparoscopic procedures are performed in the early post-transplant period, even for diagnostic purposes, the incidence of conversion to open surgery due to complications like bowel injury may be higher [13]. We performed laparoscopic radical right hemi-colectomy for a patient with occult cecal cancer presenting as acute appendicitis just 6 weeks after living-donor liver transplant. Surprisingly, we encountered only mild-to-moderate congestion, with minimal bleeding tendency, probably due to good recovery after liver transplantation. We, however, encountered severe tight adhesion of the hepatic flexure of the colon to the cut surface of the transplanted liver. We avoided unnecessary injury to the porta hepatis and colon perforation by leaving a small part of the colon serosa tightly adhering to the liver. The operative time, blood loss, and duration of hospitalization for this laparoscopic colectomy were comparable with those for a liver transplant patient reported in the literature [14]. In addition, no definite local recurrence was observed at the 2-year follow-up. This operative experience denoted that upper-abdominal surgery may be more difficult to perform than lower-abdominal surgery in liver transplant patients due to the adhesion of viscera onto the cut liver surface of the transplanted liver.
A similar condition was encountered during laparoscopic nephroureterectomy for distal ureter cancer in a deceased-donor KT patient who had received laparoscopic right lobectomy 3 months prior to the nephrectomy. We used the same method by leaving a small part of Gerota’s fascia adhering to the cut surface of the liver to prevent liver injury.
Unlike hepatic cirrhosis, noncirrhotic livers do not show the complications of jaundice, ascites, thrombocytopenia, or malnutrition. The higher HCC resection rate among the post-kidney transplantation group with better prognosis was related to their noncirrhotic livers [15].
Among the upper-GI surgery group, the patient who underwent laparoscopic sleeve gastrectomy 3 years after kidney transplant did not show more severe adhesion, edema, or bleeding tendency than those in non-transplant patients. The patient had significant weight loss with consequent improvement of blood pressure, sugar level control, lipid levels, and creatinine levels. Several studies have reported good outcomes of laparoscopic bariatric surgery in transplant patients [16–18]. Weight loss surgery was feasible not only for kidney transplant patients but also in liver and pancreas transplant cases (about 20%, 7 out of 34 abdominal organ transplant patients) in a series published by Renana Yemini, in which the tacrolimus blood trough levels declined slightly, but remained within therapeutic range [19].
We also attempted to use the laparoscopic approach for a patient with delayed-onset chylous ascites after living-donor LT. Laparoscopy in this case not only helped establishing a definitive diagnosis, but also helped exclude other possible etiologies like peritoneal carcinomatosis or lymphoma, which may not be detected on CT or MRI. The patient was successfully managed by complete parenteral nutrition and administration of octreotide, followed by low-fat diet with medium-chain triglycerides.
Extensive adhesion to the huge AW hernia was observed during the repair of incisional hernia in the liver transplant patients, quite similar to that observed in patients without liver transplant done by us. The postoperative course was quite smooth. Andreoni et al. also reported 9 cases of successful incisional hernia repair using Gore-Tex mesh by the laparoscopic technique in liver transplant patients, with a low incidence of infections (1–3%) and low recurrence rate (0–10%) [7,20,21]. A meta-analysis of 8 studies comparing open
The first laparoscopic nephrectomy was performed by Clayman et al. in 1990 [24]. Fornara et al. reported the use of laparoscopic bilateral nephrectomy for 11 renal transplant patients for poorly controlled hypertension [25]. Their rates of conversion of 9% and 27% for complications were comparable to the conversion rates of 7% and 16.4% noted a large series reported by Eraky et al. in immunocompetent patients undergoing unilateral laparoscopic nephrectomy [26]. Renal allograft function remained stable in all patients, without rejection or infection. Oral intake and mobilization were initiated on postoperative day 1, with a mean hospital stay of 4.2 days [26,27].
Compared with the open surgical group, patients in the laparoscopy group had significantly better postoperative parameters, such as earlier oral intake, less morphine equivalent consumption, and shorter hospital stay and convalescence [28]. These favorable outcomes were also noted in our cases.
Several studies have reported good outcome by using laparoscopic surgery for gynecological problems, including laparoscopically-assisted vaginal hysterectomy, even for a patient with a second liver transplant [29]. We performed MIS using the transvaginal and trans-abdominal approach for uterine prolapse with or without uterine bleeding for 2 kidney patients and 1 liver transplant patient, without any adverse effects. Several studies have reported that immunosuppression therapy does not contradict the effects of surgery, and good outcomes can be expected in most patients [3,30,31]. We also noted the same condition, and no adjustment of IMS was needed, as continuous daily intake of IMS after MIS could be achieved in most of the patients.
Conclusions
Our experience and literature review indicated that laparoscopic surgery including other MIS was beneficial for patients with transplanted abdominal organs. The surgeon who practices basic surgical principles and early surgical intervention with a rational threshold for conversion to open procedure can offer good surgical outcomes in these patients. Of course, further extensive studies in a larger number of cases by more experts in this field will be needed to verify the utility of our suggestions.
Figures
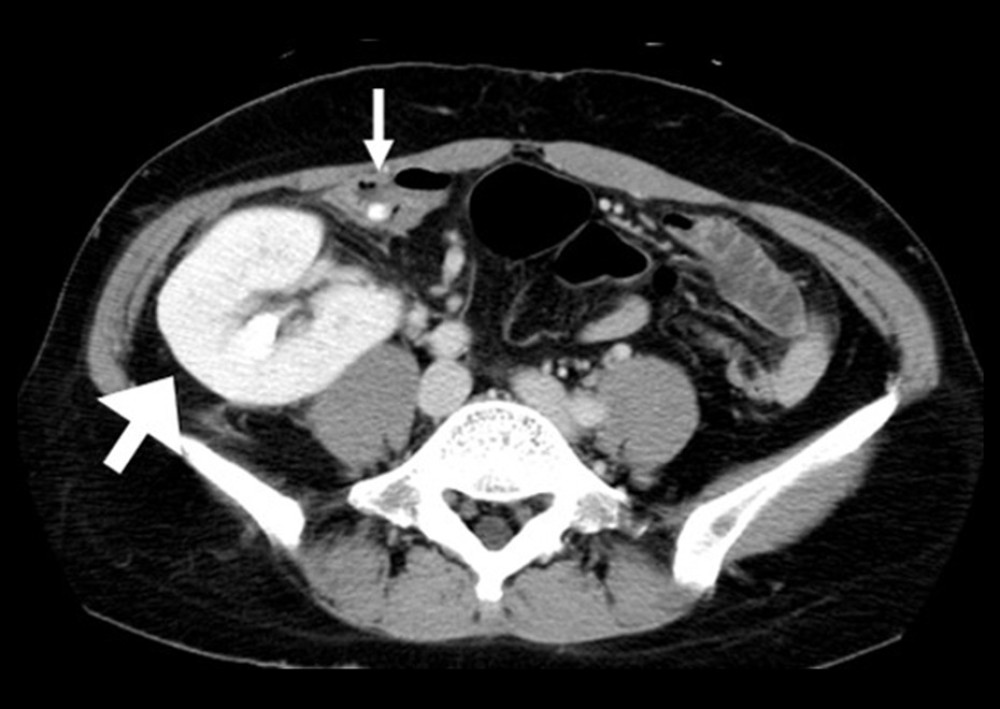 Figure 1. The appendix with fecalith (small arrow) was pushed to medial aspect by the transplanted kidney (large arrow).
Figure 1. The appendix with fecalith (small arrow) was pushed to medial aspect by the transplanted kidney (large arrow). 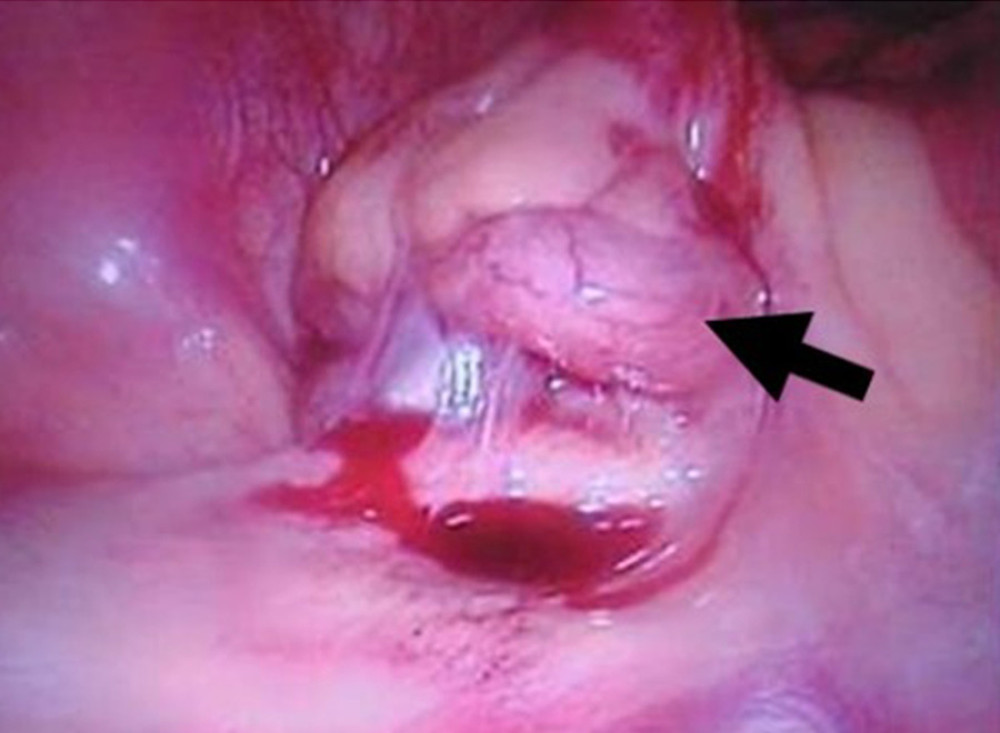 Figure 2. Tumor formation of appendicitis under laparoscopic view in a patient with kidney transplant.
Figure 2. Tumor formation of appendicitis under laparoscopic view in a patient with kidney transplant. 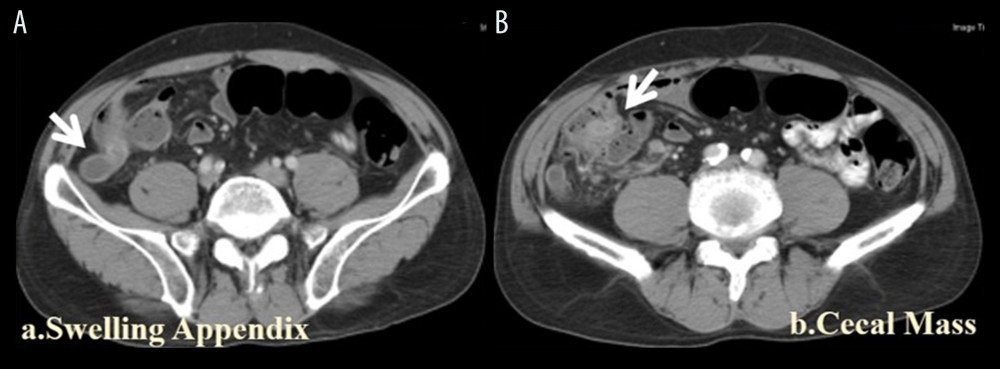 Figure 3. Cecal cancer. (A) Swollen and dilated appendix in a case with cecal tumor. (B) A polypoid tumor was noted in the cecum at the root of the appendix.
Figure 3. Cecal cancer. (A) Swollen and dilated appendix in a case with cecal tumor. (B) A polypoid tumor was noted in the cecum at the root of the appendix. 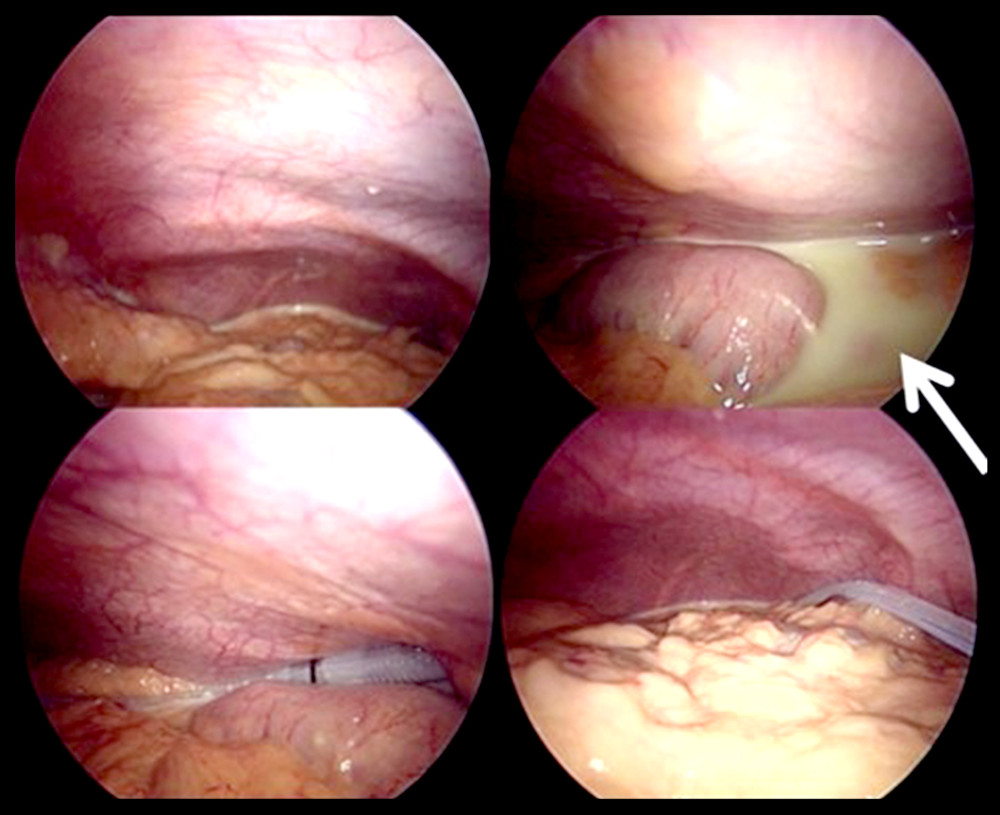 Figure 4. Yellowish turbid milky (chylous) ascites seen under laparoscopy.
Figure 4. Yellowish turbid milky (chylous) ascites seen under laparoscopy. 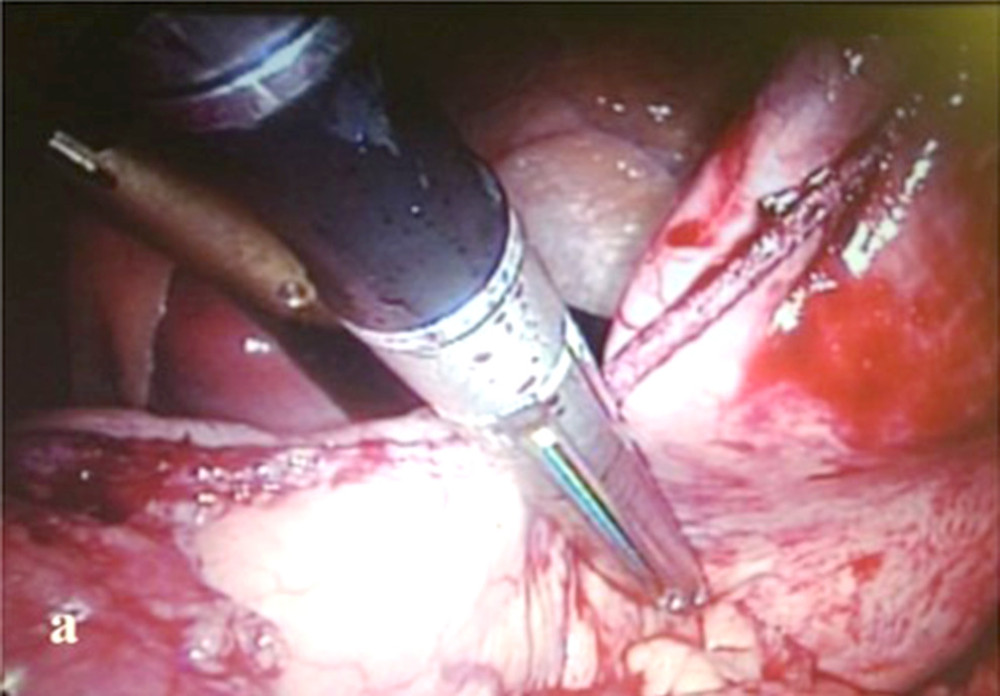 Figure 5. Laparoscopic sleeve gastrectomy in a patient with kidney transplant. Resection lateral to the oral gastric tube placed along the lesser curvature.
Figure 5. Laparoscopic sleeve gastrectomy in a patient with kidney transplant. Resection lateral to the oral gastric tube placed along the lesser curvature. 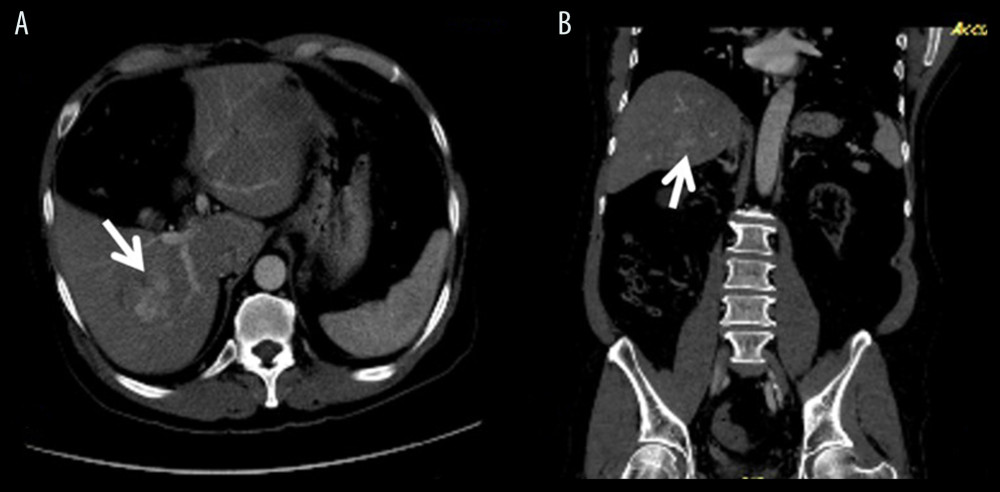 Figure 6. HCC. (A) A heterogenous early wash-out HCC in right lobe, segment 6, 7. (B) The same lesion on coronal section in CT abdomen.
Figure 6. HCC. (A) A heterogenous early wash-out HCC in right lobe, segment 6, 7. (B) The same lesion on coronal section in CT abdomen. 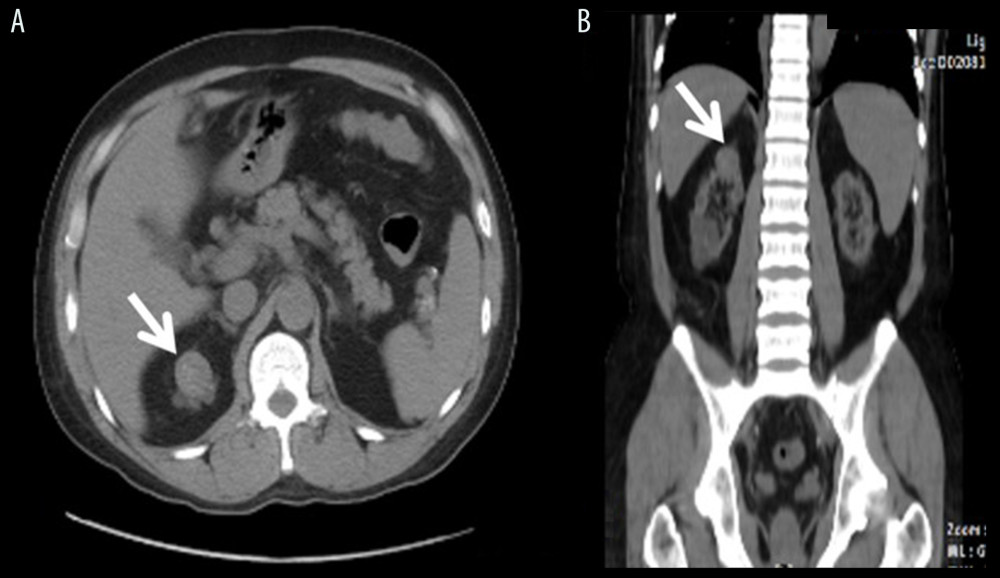 Figure 7. RCC. (A) A polypoid hyperdense tumor at the upper pole of right native kidney. (B) The same lesion seen in coronal section of CT abdomen.
Figure 7. RCC. (A) A polypoid hyperdense tumor at the upper pole of right native kidney. (B) The same lesion seen in coronal section of CT abdomen. 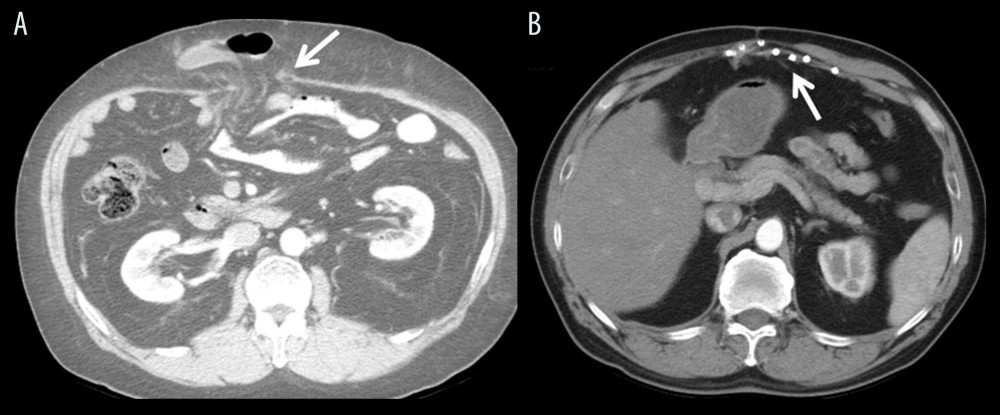 Figure 8. Incisional hernia. (A) Incisional hernia with evisceration. (B) Follow-up CT showed repair with mesh and no recurrence.
Figure 8. Incisional hernia. (A) Incisional hernia with evisceration. (B) Follow-up CT showed repair with mesh and no recurrence. 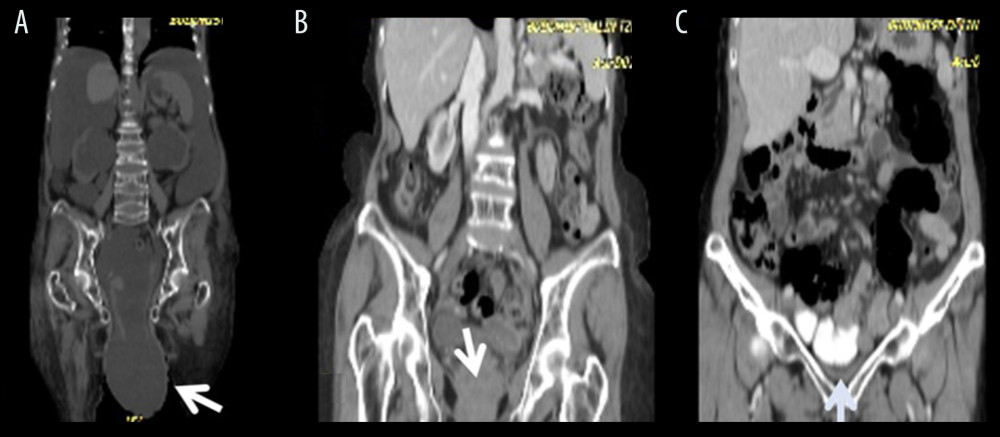 Figure 9. Prolapse uterus. (A) Severe uterine prolapse in liver cirrhosis due to massive ascites before liver transplant. (B) Persistent marked prolapse uterus after transplant. (C) No prolapse after reconstruction.
Figure 9. Prolapse uterus. (A) Severe uterine prolapse in liver cirrhosis due to massive ascites before liver transplant. (B) Persistent marked prolapse uterus after transplant. (C) No prolapse after reconstruction. References
1. Sutariya VK, Tank AH, An audit of laparoscopic cholecystectomy in renal transplant patients: Ann Med Health Sci Res, 2014; 4; 48-50
2. Matas AJ, OPTN/SRTR 2013 Annual Date Report: Kidney: Am J Transplant, 2015; 15( Suppl 2); 1-34
3. U.S. Department of Health and Human Services, Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation: Annual report of the U.S. Organ Procurement and Transplantation Network and the Scientific Registry of Transplant Recipients: Transplant data (1999–2008), 2009, Washington, DC, U.S. Department of Health and Human Services 2009
4. Voeller G, Butts A, Vera S, Kidney transplant lymphocele: Treatment with laparoscopic drainage and omental packing: J Laparoendosc Surg, 1992; 2; 53-55
5. Melvin WS, Bumgardner GL, Davies EA, The laparoscopic management of post-transplant lymphocele. A critical review: Surg Endosc, 1997; 11; 245-48
6. Testa G, Goldstein RM, Toughanipour A, Guidelines for surgical procedures after liver transplantation: Ann Surg, 1998; 227; 590-99
7. Andreoni KA, Lightfoot H, Gerber DA, Laparoscopic incisional hernia repair in liver transplant and other immunosuppressed patients: Am J Transplant, 2002; 2; 349-54
8. Wu L, Zhang J, Guo Z, Diagnosis and treatment of acute appendicitis after orthotopic liver transplant in adults: Exp Clin Transplant, 2011; 9; 113-17
9. Ince V, Barut B, Ozdemir F, The management of acute appendicitis in liver transplant patients: How effective is the Alvarado score?: North Clin Istanb, 2017; 4; 262-66
10. Hudson HM, Hakaim AG, Birkett DH, Laparoscopic cholecystectomy in a renal transplant recipient: Surg Endosc, 1992; 6; 193-94
11. DeIorio T, Thompson A, Larson GM, Laparoscopic cholecystectomy in transplant patients: Surg Endosc, 1993; 7; 404-7
12. Varga M, Kudla M, Vargova L, Fronek J, Laparoscopic cholecystectomy for acute cholecystitis after renal transplantations: Transplant Proc, 2016; 48; 2072-75
13. Merenda R, Gerunda GE, Neri D, Laparoscopic surgery after orthotopic liver transplantation: Liver Transpl, 2000; 6; 104-7
14. Rossi G, Mentz R, Vaccaro CA, Laparoscopic colectomy for colon cancer after liver transplantation: CRSLS, 2014 e2014.00224
15. Hsu NW, Chuang FR, Chen YT, Hepatocellular carcinoma in kidney transplant recipients: Transplant Proc, 2010; 42; 811-13
16. Taneja S, Gupta S, Wadhawan M, Goyal N, Single-lobe living donor liver transplant in a morbidly obese cirrhotic patient preceded by laparoscopic sleeve gastrectomy: Case Rep Transplant, 2013; 3; 279651
17. Marks WH, Florence LS, Chapman PH, Morbid obesity is not a contraindication to kidney transplantation: Am J Surg, 2004; 187; 635-38
18. Arias RH, Mesa L, Posada JG, Vélez JP, Kidney transplantation and gastric bypass: A better control of comorbidities: Obes Surg, 2010; 20; 851-54
19. Yemini R, Nesher E, Winkler J, Bariatric surgery in solid organ transplant patients: Long-term follow-up results of outcome, safety, and effect on immunosuppression: Am J Transplant, 2018; 18; 2772-80
20. Mekeel K, Mulligan D, Reddy KS, Laparoscopic incisional hernia repair after liver transplantation: Liver Transpl, 2007; 13; 1576-81
21. Hegab B, Abdelfattah MR, Azzam A, Al Sebayel M, The usefulness of laparoscopic hernia repair in the management of incisional hernia following liver transplantation: J Minim Access Surg, 2016; 12; 58-62
22. Goodney PP, Birkmeyer CM, Birkmeyer JD, Short-term outcomes of laparoscopic and open ventral hernia repair: A meta-analysis: Arch Surg, 2002; 137; 1161-65
23. Sommacale D, Nagarajan G, Lhuaire M, Surgical procedures in liver transplant patients: A monocentric retrospective cohort study: Int J Surg, 2017; 41; 58-64
24. Clayman RV, Kavoussi LR, Soper NJ, Laparoscopic nephrectomy: N Engl J Med, 1991; 324; 1370-71
25. Fornara P, Doehn C, Fricke L, Laparoscopic bilateral nephrectomy: Results in 11 renal transplant patients: J Urol, 1997; 157; 445-49
26. Doehn C, Fornara P, Fricke L, Jocham D, Comparison of laparoscopic and open nephroureterectomy for benign disease: J Urol, 1998; 159(3); 732-34
27. Eraky I, EI-Kappany HA, Ghoneim MA, Laparoscopic nephrectomy: Mansoura experience with 106 cases: Br J Urol, 1995; 75(3); 271-75
28. Hinton S, Aronoff R, Bilateral native nephrectomy for refractory hypertension in kidney transplant and kidney pancreas transplant patients: Int J Surg Case Rep, 2015; 15; 127-29
29. Rad MT, Wallwiener M, Schemmer P, Laparoscopically assisted vaginal hysterectomy in a patient with micro-invasive cervical cancer after two liver transplantations: J Obstet Gyn Canada, 2012; 34(4); 363-66
30. Deziel DJ, Hyser MJ, Doolas A, Major abdominal operations in acquired immunodeficiency syndrome: Am Surg, 1990; 56(7); 445-50
31. Meyer AA, The surgical management of AIDS and HIV-infected patients: Adv Surg, 1989; 22; 57-73
Figures
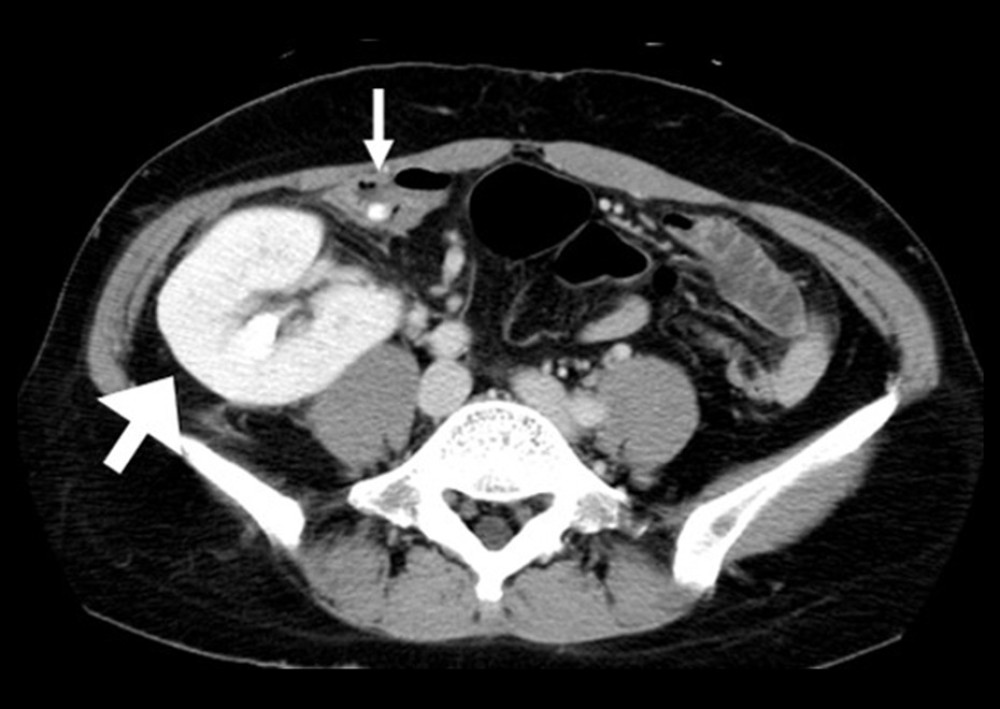 Figure 1. The appendix with fecalith (small arrow) was pushed to medial aspect by the transplanted kidney (large arrow).
Figure 1. The appendix with fecalith (small arrow) was pushed to medial aspect by the transplanted kidney (large arrow).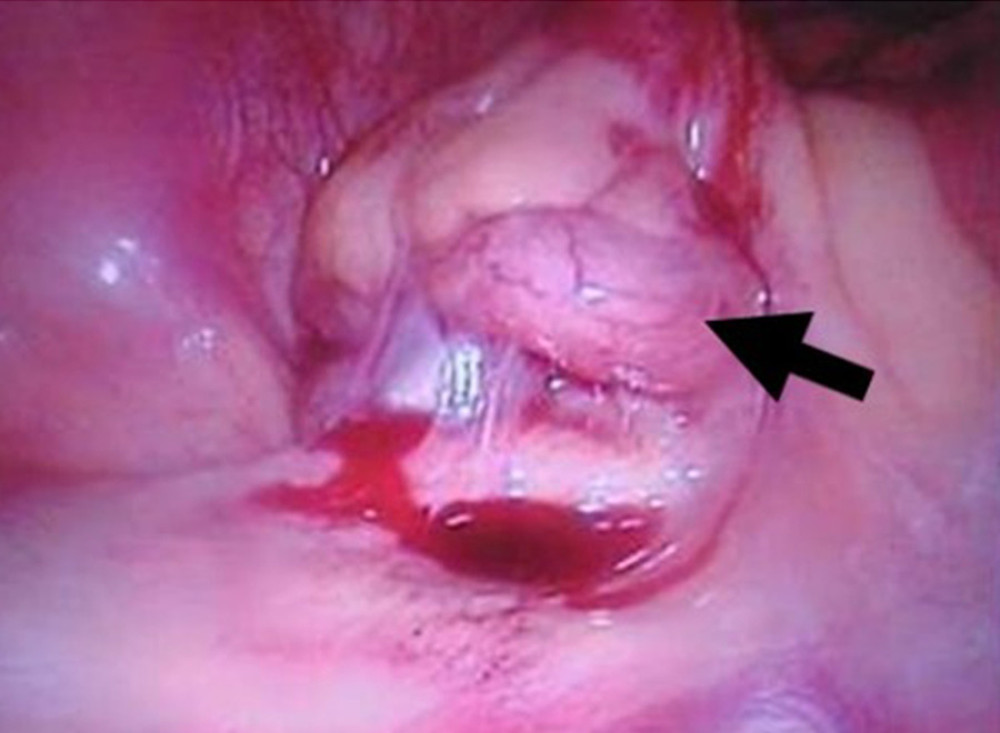 Figure 2. Tumor formation of appendicitis under laparoscopic view in a patient with kidney transplant.
Figure 2. Tumor formation of appendicitis under laparoscopic view in a patient with kidney transplant.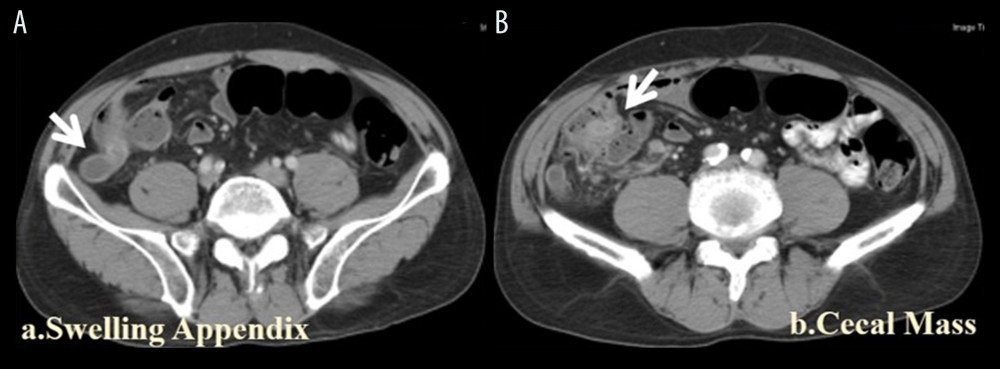 Figure 3. Cecal cancer. (A) Swollen and dilated appendix in a case with cecal tumor. (B) A polypoid tumor was noted in the cecum at the root of the appendix.
Figure 3. Cecal cancer. (A) Swollen and dilated appendix in a case with cecal tumor. (B) A polypoid tumor was noted in the cecum at the root of the appendix.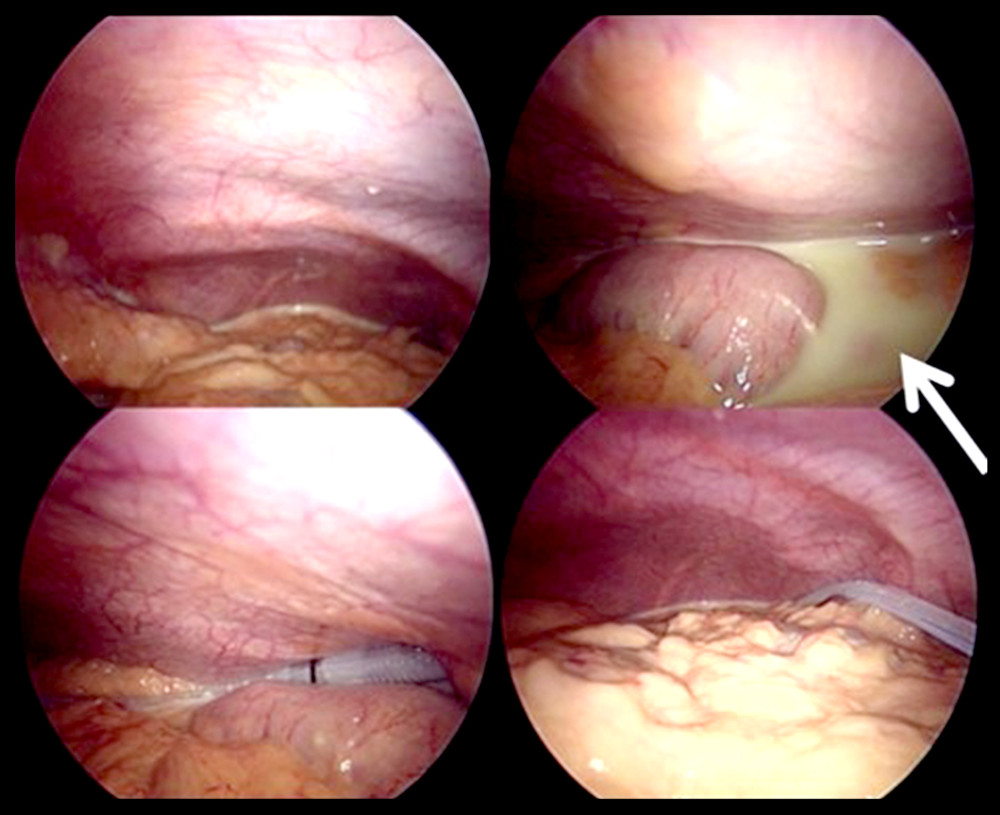 Figure 4. Yellowish turbid milky (chylous) ascites seen under laparoscopy.
Figure 4. Yellowish turbid milky (chylous) ascites seen under laparoscopy.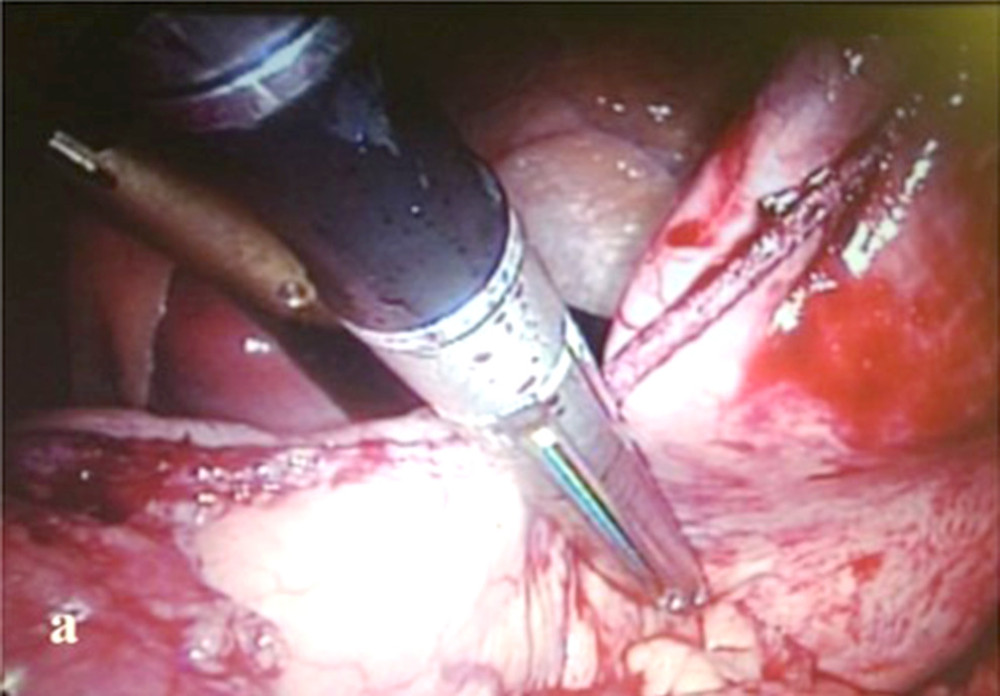 Figure 5. Laparoscopic sleeve gastrectomy in a patient with kidney transplant. Resection lateral to the oral gastric tube placed along the lesser curvature.
Figure 5. Laparoscopic sleeve gastrectomy in a patient with kidney transplant. Resection lateral to the oral gastric tube placed along the lesser curvature.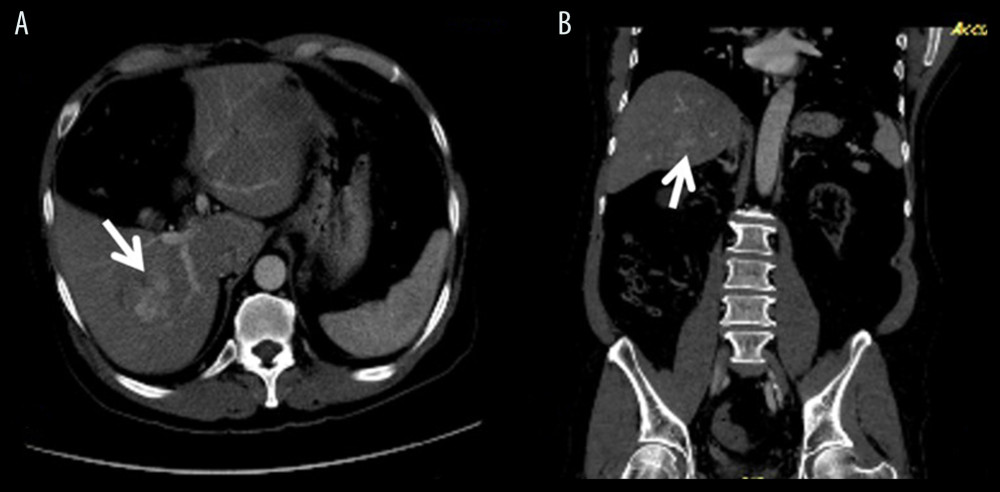 Figure 6. HCC. (A) A heterogenous early wash-out HCC in right lobe, segment 6, 7. (B) The same lesion on coronal section in CT abdomen.
Figure 6. HCC. (A) A heterogenous early wash-out HCC in right lobe, segment 6, 7. (B) The same lesion on coronal section in CT abdomen.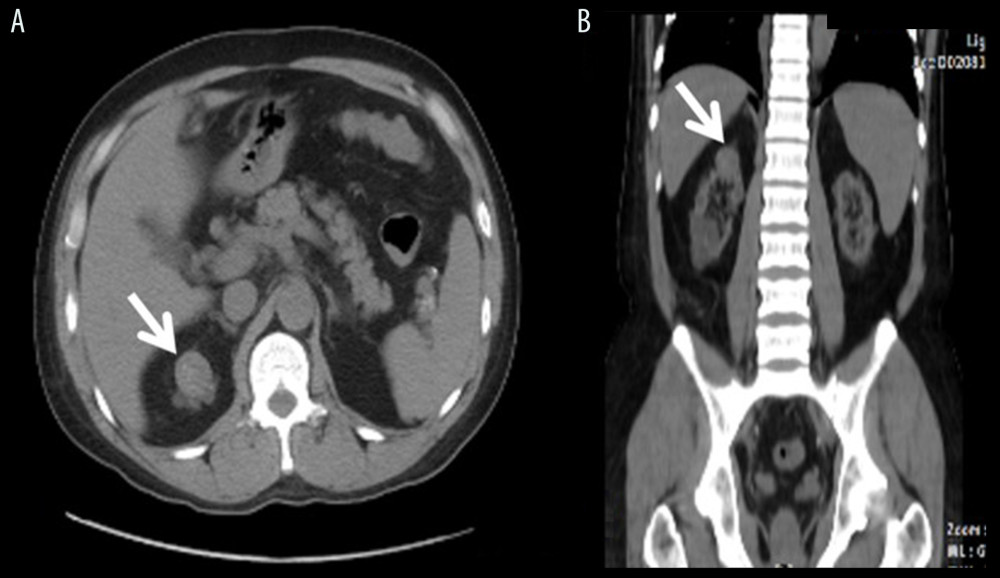 Figure 7. RCC. (A) A polypoid hyperdense tumor at the upper pole of right native kidney. (B) The same lesion seen in coronal section of CT abdomen.
Figure 7. RCC. (A) A polypoid hyperdense tumor at the upper pole of right native kidney. (B) The same lesion seen in coronal section of CT abdomen.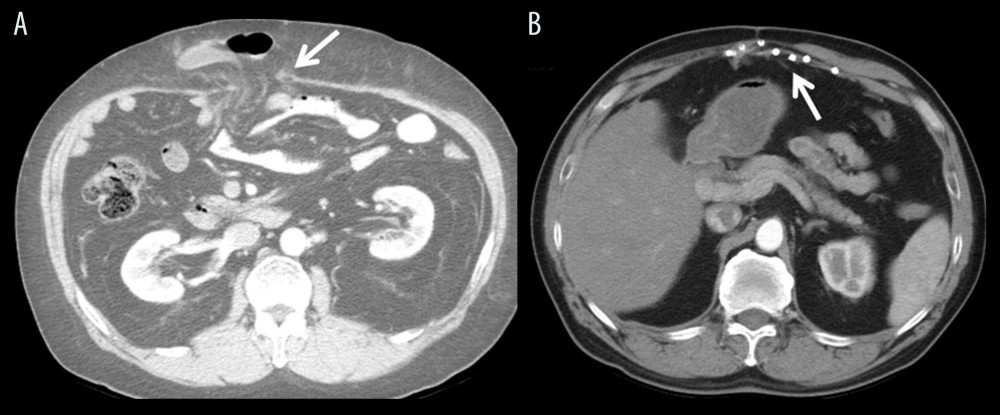 Figure 8. Incisional hernia. (A) Incisional hernia with evisceration. (B) Follow-up CT showed repair with mesh and no recurrence.
Figure 8. Incisional hernia. (A) Incisional hernia with evisceration. (B) Follow-up CT showed repair with mesh and no recurrence.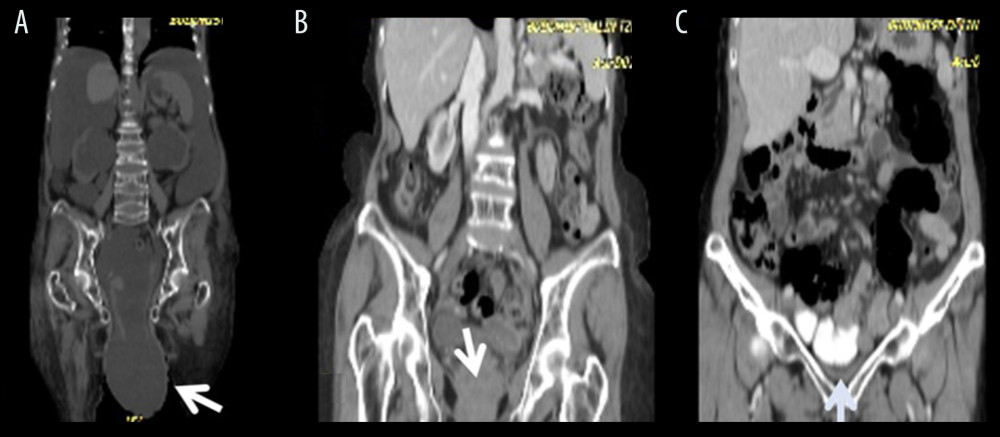 Figure 9. Prolapse uterus. (A) Severe uterine prolapse in liver cirrhosis due to massive ascites before liver transplant. (B) Persistent marked prolapse uterus after transplant. (C) No prolapse after reconstruction.
Figure 9. Prolapse uterus. (A) Severe uterine prolapse in liver cirrhosis due to massive ascites before liver transplant. (B) Persistent marked prolapse uterus after transplant. (C) No prolapse after reconstruction. In Press
18 Mar 2024 : Original article
Does Antibiotic Use Increase the Risk of Post-Transplantation Diabetes Mellitus? A Retrospective Study of R...Ann Transplant In Press; DOI: 10.12659/AOT.943282
20 Mar 2024 : Original article
Transplant Nephrectomy: A Comparative Study of Timing and Techniques in a Single InstitutionAnn Transplant In Press; DOI: 10.12659/AOT.942252
28 Mar 2024 : Original article
Association Between FEV₁ Decline Rate and Mortality in Long-Term Follow-Up of a 21-Patient Pilot Clinical T...Ann Transplant In Press; DOI: 10.12659/AOT.942823
02 Apr 2024 : Original article
Liver Transplantation from Brain-Dead Donors with Hepatitis B or C in South Korea: A 2014-2020 Korean Organ...Ann Transplant In Press; DOI: 10.12659/AOT.943588
Most Viewed Current Articles
05 Apr 2022 : Original article
Impact of Statins on Hepatocellular Carcinoma Recurrence After Living-Donor Liver TransplantationDOI :10.12659/AOT.935604
Ann Transplant 2022; 27:e935604
12 Jan 2022 : Original article
Risk Factors for Developing BK Virus-Associated Nephropathy: A Single-Center Retrospective Cohort Study of ...DOI :10.12659/AOT.934738
Ann Transplant 2022; 27:e934738
22 Nov 2022 : Original article
Long-Term Effects of Everolimus-Facilitated Tacrolimus Reduction in Living-Donor Liver Transplant Recipient...DOI :10.12659/AOT.937988
Ann Transplant 2022; 27:e937988
15 Mar 2022 : Case report
Combined Liver, Pancreas-Duodenum, and Kidney Transplantation for Patients with Hepatitis B Cirrhosis, Urem...DOI :10.12659/AOT.935860
Ann Transplant 2022; 27:e935860