07 April 2021: Clinical Research
Beyond Sociodemographic and COVID-19-Related Factors: The Association Between the Need for Psychological and Information Support from School and Anxiety and Depression
Na Meng1ABCEF, Zheng Liu2ABE, Ya Wang2BD, Yan Feng3B, Qin Liu4B, Junqiang Huang5F, Xiaolin Li6ACG*DOI: 10.12659/MSM.929280
Med Sci Monit 2021; 27:e929280
Abstract
BACKGROUND: In addition to sociodemographic and COVID-19- related factors, the needs of school support, including material, psychological and information support, have seldom been discussed as factors influencing anxiety and depression among college students during the COVID-19 pandemic.
MATERIAL AND METHODS: In this cross-sectional study, 3351 college students from China were surveyed through questionnaires about their sociodemographic and COVID-19 characteristics, the needs of school support, and their experiences with anxiety and depression.
RESULTS: Anxiety and depression were reported by 6.88% and 10.50% of students, respectively. Married, higher education, non-medical, and urban students had significantly higher risks of anxiety or depression. Additionally, symptoms such as cough and fever, especially when following a possible contact with suspected individuals, quarantine history of a personal contact, going out 1-3 times a week, not wearing a mask, and spending 2-3 hours browsing COVID-19-related information were significantly associated with the occurrence of anxiety or depression. Those who used methods to regulate their emotional state, used a psychological hotline, and who had visited a psychiatrist showed higher anxiety or depression. Those who used online curricula and books, used preventive methods for COVID-19, and who had real-time information about the epidemic situation of the school showed lower anxiety and depression.
CONCLUSIONS: In addition to sociodemographic and COVID-19-related aspects, students’ needs for psychological assistance and information from schools were also associated with anxiety and depression among college students.
Keywords: Anxiety, COVID-19, Depression, Needs Assessment, Students, Adolescent, COVID-19, Communicable Disease Control, Cross-Sectional Studies, Financial Support, Health Education, Hotlines, Information Dissemination, Mental Health, Pandemics, Prevalence, Psychosocial Support Systems, Schools, Socioeconomic Factors, Surveys and Questionnaires, young adult
Background
The new coronavirus, referred to as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was reported for the first time in Wuhan, China in December 2019 [1]. SARS-CoV-2 expanded rapidly worldwide through contact or aerosol transmission [2]. On March 11th, the World Health Organization (WHO) declared the coronavirus disease 2019 (COVID-19) a global pandemic [3]. To control the COVID-19 outbreak, WHO advocates that the public should avoid going to crowded places, should wear surgical masks, and keep at least 1-meter distance from others [3].
In China, all colleges and universities were closed to control the epidemic after the pandemic of COVID-19. College students underwent home quarantine and had no idea about when they could go back to school [4]. Firstly, with the increasing number of confirmed cases and deaths, as well as the lack of protective resources, many college students experienced serious anxiety, depression, and fear levels [5]. Secondly, people in quarantined areas were likely to feel bored, lonely, angry, and became distressed [6]. Thirdly, college students experienced additional pressure caused by the closure of education institutions [7]. College students were also faced with course interruptions, which further increased the degree of stress and uncertainty [8]. Furthermore, graduate students were confronted with delayed final examinations and uncertainty of employment [9], which may lead to anxiety. Therefore, college students may face mental health problems caused by COVID-19.
More than 160 countries have implemented school closures nationwide, which affected over 87% of students worldwide [10]. The previous study showed that 16.5% and 28.8% of the general population had moderate-to-severe depression and anxiety, respectively, during the initial phase of the COVID-19 outbreak (31 January-2 February 2020) in China [11]. The indefinite city closure, the uncertainty of academic progress, and potential negative emotions may adversely affect the mental health of college students [11]. Several studies explored the possible factors influencing mental health problems. These possible factors include gender, grade [12], major [13], epidemic, prevention knowledge [14], contact history with COVID-19 patients [15], the influence of COVID-19 on daily life, and academic delays due to COVID-19 [16]. When considering the possible factors influencing mental health problems, previous studies mainly focused on the sociodemographic characteristics and COVID-19-related factors such as mask usage and knowledge. Few studies focused on the possible factors from the perspective of what colleges and universities could provide. Meanwhile, several researchers have previously pointed out the lack of “beyond the population” investigations on mental health problems of college students [17].
The present cross-sectional study was conducted to assess the prevalence of anxiety and depression among college students, and to explore factors associated with the sociodemographic characteristics, COVID-19-related factors, and the school support that students need.
Material and Methods
PARTICIPANTS:
A total of 3351 college students from all over China were recruited in this cross-sectional study by snowball sampling from 14 February 2020 to 21 February 2020. The inclusion criteria included: (a) full-time college students; (b) voluntary participation.
SOCIODEMOGRAPHIC AND COVID-19-RELATED DATA:
Sociodemographic characteristics were assessed by a self-administrated questionnaire, including gender, age, education level, medical major or not, marital status, living situation, and place of residence. COVID-19-related data were designed to reflect the quarantine conditions, symptoms, COVID-19-related behaviors, and mask use of students and their close contacts.
STUDENTS’ NEEDS FOR SCHOOL SUPPORT:
A total of 14 dichotomous questions were used to ask students if they needed material, psychological, and information support provided by schools. Material support included setting a special COVID-19-related fund, providing books or laptops for students, supplying protective equipment, arranging and mailing clothes for students, and taking care of pets and plants. Psychological support included emotional regulation, professional psychological counseling, and a hotline. Information support included course-related online curricula and books, authoritative information and skills to deal with rumors, courses on preventive measures, real-time tracking of the epidemic situation of the school, course arrangements, employment or part-time jobs, and online social groups.
ASSESSMENT OF STUDENTS’ ANXIETY AND DEPRESSION: The Generalized Anxiety Disorder 7-item (GAD-7) Scale and the Patient Health Questionnaire-9 (PHQ-9) were used to assess anxiety and depression. The GAD-7, developed by Spitzer [18], contains 7 items and is widely used to evaluate anxiety. Each item is scored on a scale of 0 to 3 with a maximum total score of 21. The anxiety severity was determined based on the total GAD-7 score, with scores of 0–4 indicating minimal anxiety, 5–9 indicating mild anxiety, 10–14 suggesting moderate anxiety, and 15 or greater indicating severe anxiety (Cronbach’s α was 0.92 [18]). In our study, the Cronbach’s alpha coefficient of the GAD-7 was 0.93. GAD-7 scores ≥10 points were defined as anxiety. The PHQ-9 was developed by Kroenke [19] and is widely used to assess depression. It contains 9 items, with each item scored on a scale of 0 to 3. The depression severity was determined based on the total score: scores of 0–4 indicate minimal depression, 5–9 indicate mild depression, 10–14 indicate moderate depression, 15–19 indicate moderately severe depression, and scores ≥20 indicate severe depression (Cronbach’s α was 0.89 [19]). In our study, the Cronbach’s alpha coefficient of the PHQ-9 was 0.92. PHQ-9 scores ≥10 points were defined as depression.
PROCEDURES:
All assessments were performed by 6 experienced researchers. The questionnaires were stored in WJX, an online survey platform. The online questionnaires were completed by 20 students during the pre-survey phase, requiring an average time of 3–8 min. The WJX link to the questionnaires was then sent to students individually via their WeChat accounts (a social software similar to WhatsApp) or WeChat groups that consists of college students. College students could voluntarily participate in the survey and were encouraged to share the link with their schoolmates. The link was clicked by 8333 participants. Finally, 3351 participants completed the questionnaires, with a 40.21% participation rate.
All items in the questionnaire were mandatory. Each WeChat ID could only fill in the questionnaire once to avoid an invalid repeat. Additionally, students had the possibility of filling out the online questionnaire even if they exited the link before submission. Moreover, key features such as the requirement for “full-time college students only” were highlighted in bold red to avoid misfilings. Students were encouraged to participate and carefully fill out the questionnaire through incentives such as the final assessment outcome, interpretations, and suggestions.
DATA ANALYSIS:
Sociodemographic and COVID-19-related data, as well as anxiety, depression, emotional self-regulation, and needs-related scores, were expressed as frequencies, percentages (n%), means±standard deviations (M±SD), medians, and 25th–75th percentiles. The sociodemographic and COVID-19-related characters were compared between the anxiety and the non-anxiety group, as comparing the depression and non-depression group, using ANOVA and chi-square test. Two multiple logistic regression models were built to explore the factors associated with anxiety and depression among college students. Considering the collinearity with the highest education level, 2 regression models did not include age as an independent variable. The other independent variables are listed in Tables 1 and 2. Multiple categorical variables were set as dummy variables. All models used a forward stepwise likelihood ratio. The statistical significance level was set at P<0.05. All statistical analyses were performed in SPSS version 22.
ETHICS APPROVAL:
This study was approved by the Ethics Committee of The One Tertiary Hospital (No. 323, 2020). Each participant signed an online informed consent and was thoroughly briefed on the background, content, benefits, and risks of this study, as well as the rights of volunteers and anonymity upon visiting the WJX link. The information of all participants was anonymous and each individual had the choice of exiting the study at any time. Study-related questions were addressed through phone calls by professor Li.
Results
A total of 3351 questionnaires were collected. Forty-seven college students expressed privacy-related concerns and declined to be incorporated into the final results of the study. Data from the remaining 3304 questionnaires were analyzed. The sociodemographic characteristics are shown and compared in Table 1. The COVID-19 related characteristics are shown and compared in Table 2. The school support that college students needed is shown in Table 3. Anxiety and depression were reported by 6.88% and 10.50%, respectively, of the surveyed college students (Table 4).
The factors independently associated with anxiety are shown in Table 5. Junior students and rural students showed a significantly lower risk of anxiety. The results also demonstrated that anxiety was significantly associated with the COVID-19-related factors, such as a history of close contact with people under quarantine, fever or cough, and mask usage. Compared with students without need for psychological support, students who need ways to regulate their emotions (OR=3.26, 95% CI=2.29–4.64), professional and psychological hotline (OR=1.87, 95% CI=1.23–2.82), and psychiatric visits (OR=2.68, 95% CI=1.75–4.10) provided by schools showed more severe anxiety. Compared with students without need for information support, students who need online curricula or books (OR=0.69, 95% CI=0.50–0.95), information on prevention and self-protection (OR=0.50, 95% CI=0.34–0.73), and real-time epidemic data of the school (OR=0.62, 95% CI=0.44–0.87) reported milder anxiety.
The factors independently associated with depression are shown in Table 6. Married, undergraduate and postgraduate, non-medical, and urban students showed significantly higher levels of depression. Depression was also significantly associated with COVID-19-related factors, such as a fever or cough, and hours spent browsing COVID-19-related information. Compared with students without need for psychological support, students who needed ways to regulate their emotions (OR=2.66, 95% CI=2.03–3.49), those who used professional and psychological hotlines (OR=1.55, 95% CI=1.10–2.18), and those who had psychiatric visits (OR=1.87, 95% CI=1.30–2.69) provided by schools showed more severe depression. Compared with students without need for information support, students who needed prevention and self-protection information provided by schools reported milder depression (OR=0.46, 95% CI=0.35–0.61).
Discussion
THE PREVALENCE OF ANXIETY AND DEPRESSION:
In this study, we found that the prevalence of anxiety was higher than in a previous study in China [20], in which 3.6% of college students reported moderate anxiety. The discrepancy may be due to differences in population distribution. Unlike a previous study published by Cao [20] et al, our study recruited junior college students and postgraduates, in addition to undergraduates. The prevalence of depression was lower than in a previous study in China, in which 19.9% of college students had depressive symptoms [21]. A possible explanation for the difference between rates might be that Pan et al [22] used Beck’s Depression Inventory to measure the depression symptoms. Another possible reason is that participants with a high level of anxiety and depression may not choose to volunteer in this survey. Another study found that the prevalence of anxiety and depression symptoms during the COVID-19 epidemic was 7.7% and 12.2%, respectively, a little higher than our findings [23], which might be due to the time frame. Wang et al performed their survey from 31 January to 2 February 2020. The survey results reflected the immediate psychological response to the crisis [23]. Our current study was conducted from 14 February 2020 to 21 February 2020, a period when the COVID-19 pandemic had already been controlled in China. Thus, our results are more reflective of the sustaining psychological responses to the disease.
COVID-19-RELATED FACTORS AND MENTAL HEALTH PROBLEMS:
Although the rate of depression might be lower than in other previous studies, our study pointed out that COVID-19-related characteristics were significantly associated with anxiety and depression among college students. Symptoms like fever and cough are associated with mental health problems among college students, and those who experienced or are experiencing a fever or cough in the past week had higher levels of anxiety. Additionally, students with a history of close contact with people under quarantine, experiencing COVID-19-associated symptoms, or people with an undetermined status generally had a higher degree of anxiety. A higher risk of depression was associated with students’ cough or fever as well as uncertainty about cough or fever among people they had had contact with. Our results suggested that both the uncertainty and risk of contracting COVID-19 were factors associated with anxiety and depression. Compared with students who did not wear a mask, students wearing masks showed lower levels of anxiety. As we all know, COVID-19 is highly contagious [3]. Students who manifested related symptoms, had a history of close contact with suspected subjects, or who did not wear a mask are at a higher risk of contracting the virus. These stressors alone hugely contribute to the occurrence of anxiety or depression. Moreover, we found that students with a history of quarantine experienced a higher degree of psychological distress [24] and were at a significant risk of anxiety and depression than their counterparts [25]. Students with infected relatives or acquaintances also exhibited anxiety-like symptoms [20]. In general, the results suggested that uncertainty is tightly related to anxiety or depression among college students. A previous study has also reported a positive association between uncertainty and anxiety and depression in patients [26]. Therefore, following the guidelines of the WHO [3], staying at home, limiting contact with people, and keeping a good daily routine, coupled with guidance from their institutions, might be very helpful in alleviating the mounting degree of uncertainty that students are facing. A significant number of students also adopted the home self-isolation method during the pandemic [27]. Although staying at home for a very long time is a challenge by itself [28], the results showed that those going out 1–3 times a week exhibited more anxiety symptoms than those who did not go out, which further advocates for the reduction of unnecessary trips.
Interestingly, compared with students who spent less time browsing for COVID-19-related information, those with 2–3 hours of browsing time showed higher degrees of anxiety and depression. However, no significant difference was seen between the group that browsed for over 3 hours the group that browsed for less than an hour. This result is not consistent with the findings of a previous study, which reported a higher risk of anxiety among people with COVID-19-related browsing time ≥3 hours [29]. This discrepancy can be explained by differences in detection power and inclusion criteria, such as healthcare workers [29]. Students usually seek information online. With the increasing number of rumors and the lack of official communications, it is easy to see how people were misled [30,31]. Our results suggest that spending less than 2 hours to browse COVID-19-related information might be a better choice for college students. Ultimately, schools should provide official and corrected COVID-19-related information for students to reduce the spread of rumors.
SOCIODEMOGRAPHIC CHARACTERISTICS AND MENTAL HEALTH PROBLEMS:
Similar to previous findings, this study also indicated a relationship between students’ sociodemographic characteristics and their psychological issues. We found that compared with unmarried or divorced students, married students showed a higher rate of depressive-like symptoms. Financial concerns played a much larger role in this trend [32]. Moreover, the findings showed that undergraduate and postgraduate students were at greater risk of developing depression and anxiety compared to their junior counterparts. This finding is similar to the results of a prior study in adolescents showing a positive correlation between students’ grades and the prevalence of anxiety and depression [12]. Compared to medical students, those non-medical students had a higher prevalence of depression. The possible reason might be that medical students had a better understanding of the virus and were more versed in preventive and protective behaviors [33]. Further analyses [34] indicated that students from rural areas were less prone to develop anxiety and depressive-like symptoms than their urban counterparts. In summary, the results suggested that being married, higher education, non-medical major, and urban college students are at a higher risk of developing psychological problems.
STUDENTS’ NEEDS FOR SCHOOL SUPPORT AND PSYCHOLOGICAL PROBLEMS:
A notable finding was that college students’ needs for school support were related to their psychological status and were significantly associated with their anxiety levels and depression symptoms. Few studies have been conducted in this area. Students who need more self-protection-related information on COVID-19 provided by schools showed less anxiety and depression than their counterparts. In our opinion, schools could provide authentic and accurate information. Accurate health and precautionary-related knowledge were associated with lower levels of stress, anxiety, and depression [11]. Moreover, one of the hot topics related to COVID-19 on social media is how to decrease risks and self-exposure to the virus [35]. Even though 1 month had already passed since the beginning of the outbreak, 40.54% of students still needed information on self-protection against COVID-19 in our study. Therefore, schools should enhance and promote well recognized preventive measures through counseling and official sites on social media.
Another finding in this study was that anxiety levels were lower among students who need real and up-to-date pandemic-related information about their school. The reason might be that those students are more sensitive and easily affected by the daily increase in confirmed cases, deaths, and rumors. University students usually anticipated transparency on the pandemic situation no matter the outcome [36]. Additionally, a study also suggested that a more empathic presentation of the pandemic evolution by the government can reduce public anxiety [37]. Therefore, schools should provide real and timely updates for students instead of delay or non-disclosure.
The results suggested that students in need of online curricula and books were at lower risk of developing anxiety. The possible reason is that those students may focus on their academic tasks instead of on COVID-19, which decreased the level of anxiety. The global education system is confronted with a significant disruption due to COVID-19 [38,39]. Facing the challenge of how to resume classes without serious exposure to the virus [8], schools could translate a face-to-face educational mode to an online delivery mode [40].
Another issue in this study was the correlation between students’ psychological needs and mental health problems. Indeed, the results showed that students in need of mood regulation mechanisms, professional counseling, and psychiatric visits, were prone to develop anxiety and depressive-like symptoms. Unquestionably, schools should build and provide a psychological support system for their students [41]. Another study showed that self-stigma also plays an important role in failing to seek help among college students [42]. Previous findings revealed that self-stigma is highly prevalent among college students and is negatively correlated with willingness to seek psychological help [43]. Thus, schools should provide counseling and online lectures on anxiety and depression, as well as providing an enlightened environment for students to alleviate the stigma surrounding mental disorders. Schools could also assess each student’s status through simple questions such as ‘do you need psychological support’. For those with a yes answer, a psychological support team could provide online one-to-one counseling or visits for severe cases.
LIMITATIONS:
One of the limitations was that the data were collected online using snowball sampling instead of random sampling. There may be a selection bias resulting from the non-response of college students with severe anxiety and depression. Additionally, the number of female participants was slightly larger than that of male students. Therefore, the sample may not reflect the entire reality of the mental status of college students. Furthermore, very few participants had a quarantine or close contact history, making the results less reflective of confirmed or suspected individuals. Random sampling and including more participants with a quarantine history would be considered to assess the relationship between quarantine and mental health in future studies. Moreover, it would be better to investigate the psychological status of college students after a period and explored the risk factors or protective factors against anxiety or depression. Lastly, this study assessed anxiety and depression using 2 self-administered scales, which may cause bias and inconsistencies in the professional assessment of anxiety and depression.
Conclusions
Moderate anxiety and depressive symptoms were reported by 6.88% and 10.50% of college students, respectively. Anxiety or depression were associated with being married, higher education level, non-medical area of study, urban residence, not wearing a mask, going out 1–3 times per week, history of 2–3 hours of browsing COVID-19-related information, symptoms of cough and fever, and a history of close contact with quarantined subjects. Furthermore, anxiety or depression is positively associated with students’ needs for psychological and information support from schools. As an emergency, COVID-19 has an impact on students’ mental health. Students need support from schools. Besides home quarantine, schools could implement mental health-related measures to decrease the incidence of anxiety and depression among college students, such as by providing emotional regulation knowledge and counseling to students during the COVID-19 pandemic.
Tables
Table 1. Sociodemographic characteristics.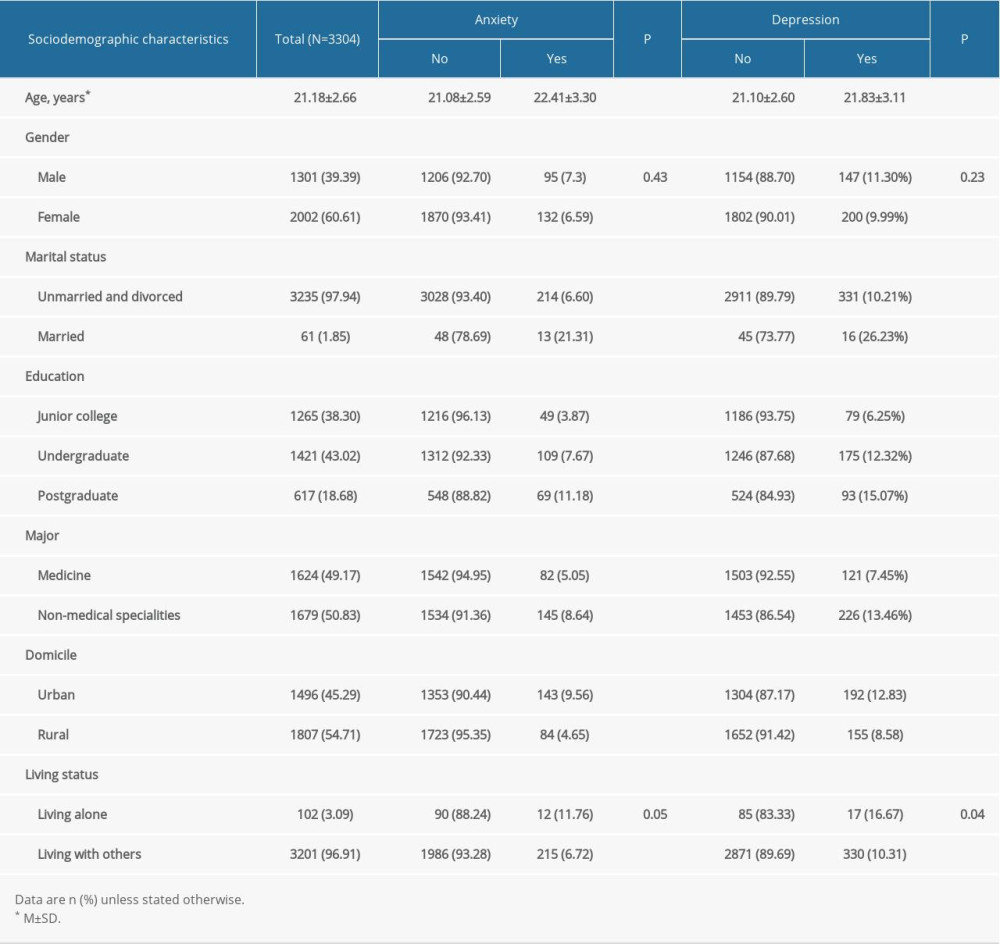 Table 2. COVID-19 related characteristics.
Table 2. COVID-19 related characteristics.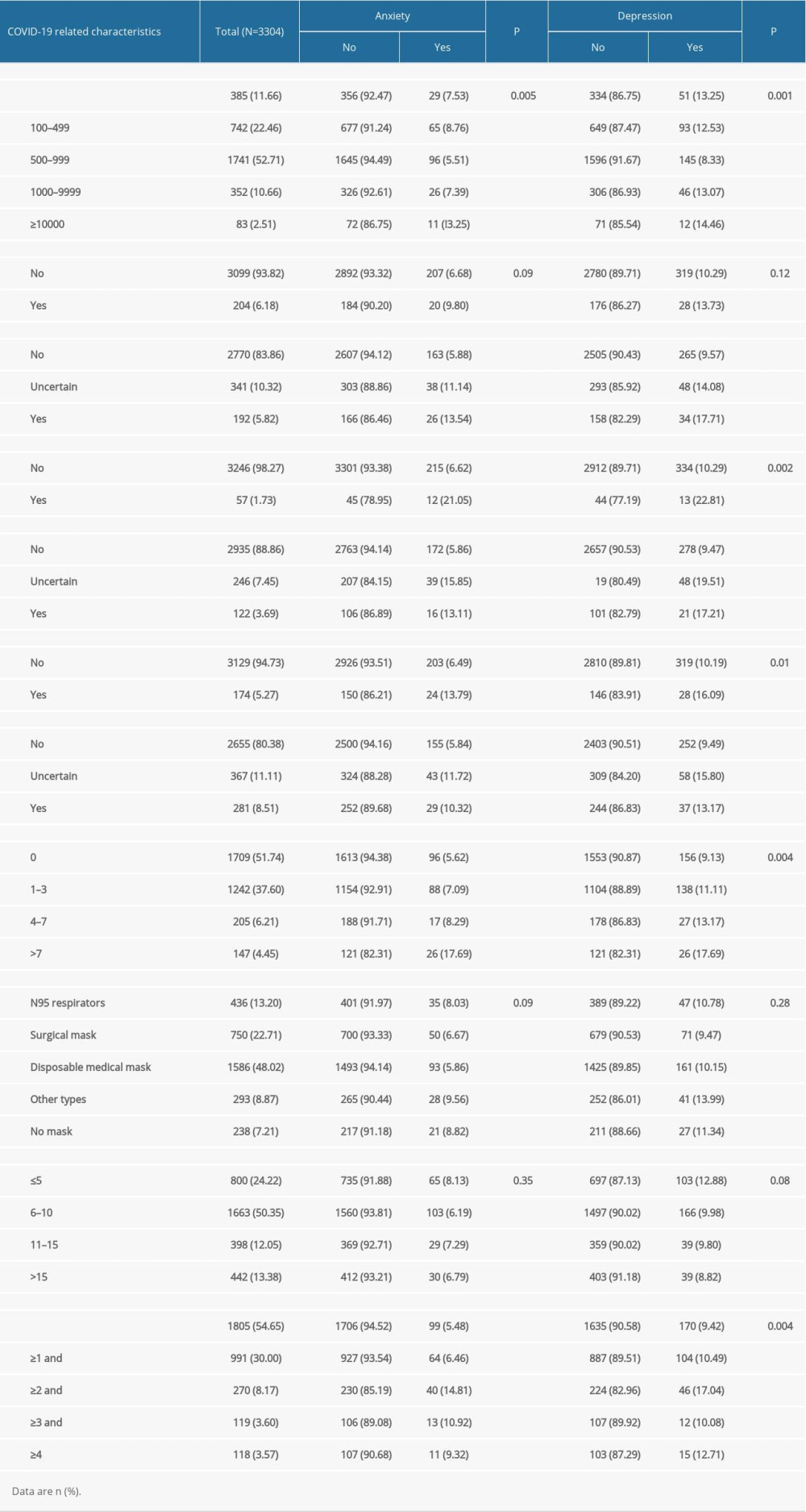 Table 3. The needs of school support (N=3304).
Table 3. The needs of school support (N=3304).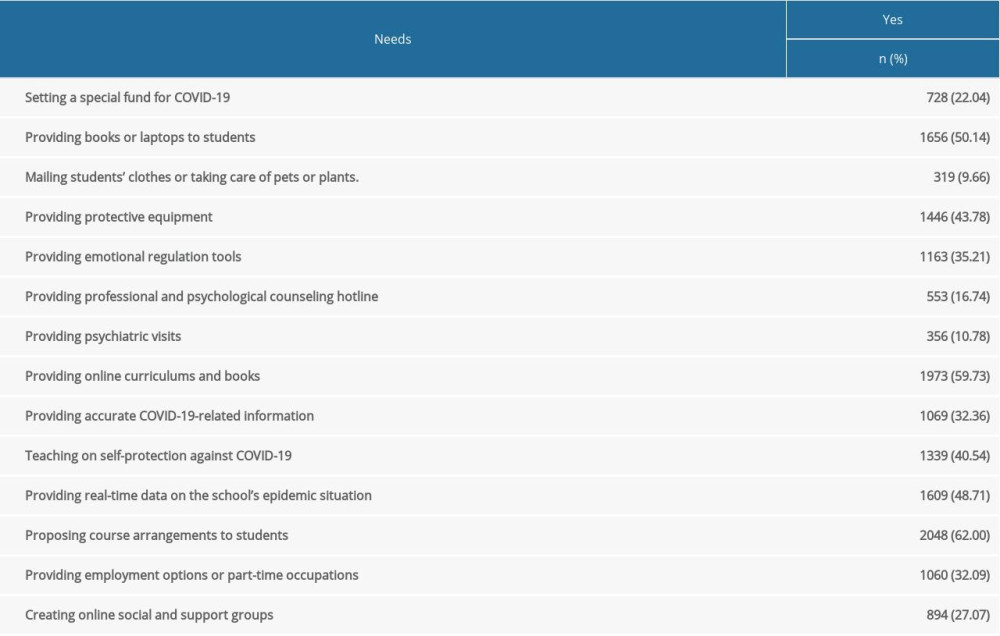 Table 4. Anxiety, depression among college students (N=3304).
Table 4. Anxiety, depression among college students (N=3304). Table 5. The logistics regression model of anxiety (N=3304).
Table 5. The logistics regression model of anxiety (N=3304).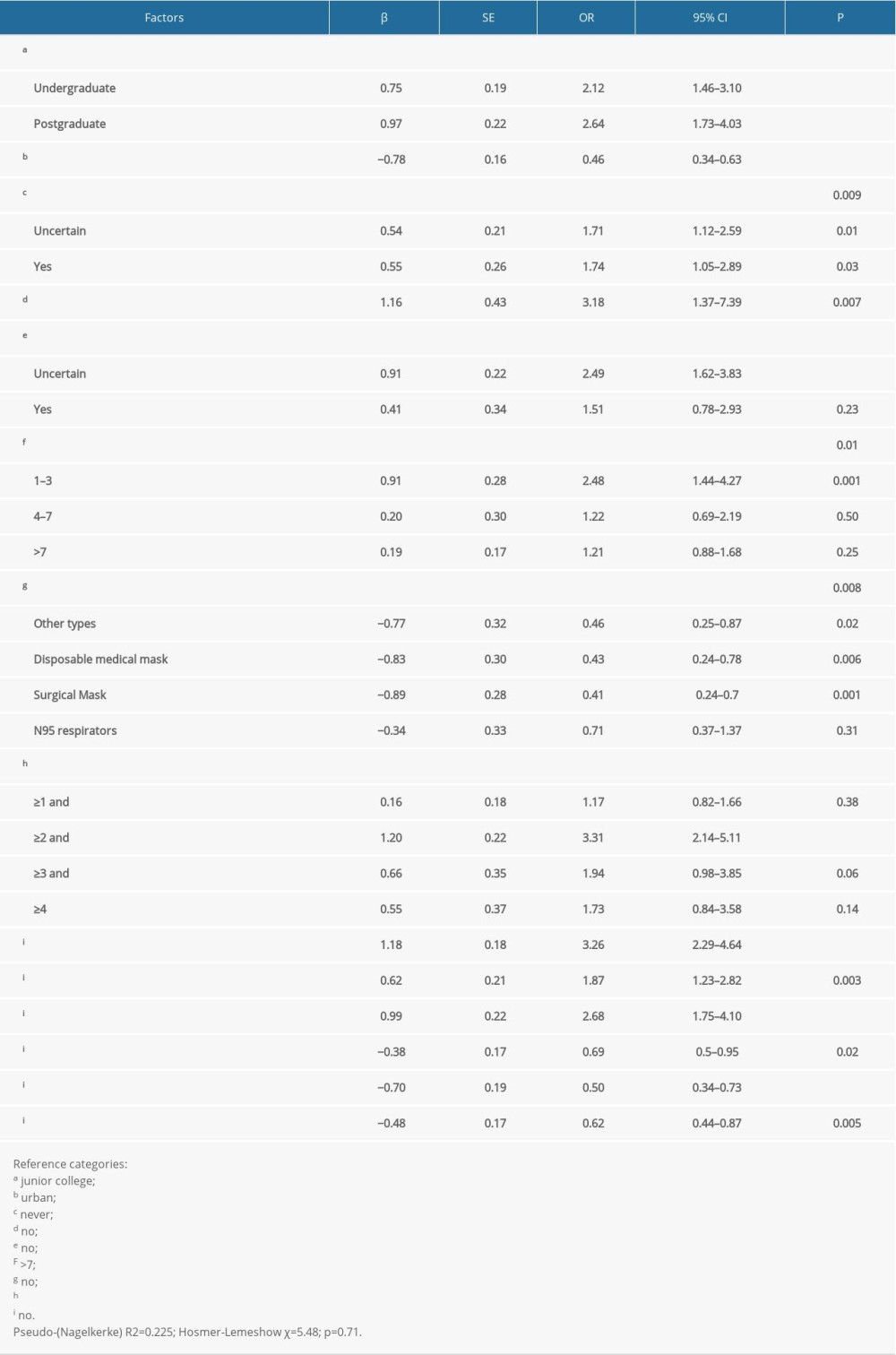 Table 6. The logistics regression model of depression (N=3304).
Table 6. The logistics regression model of depression (N=3304).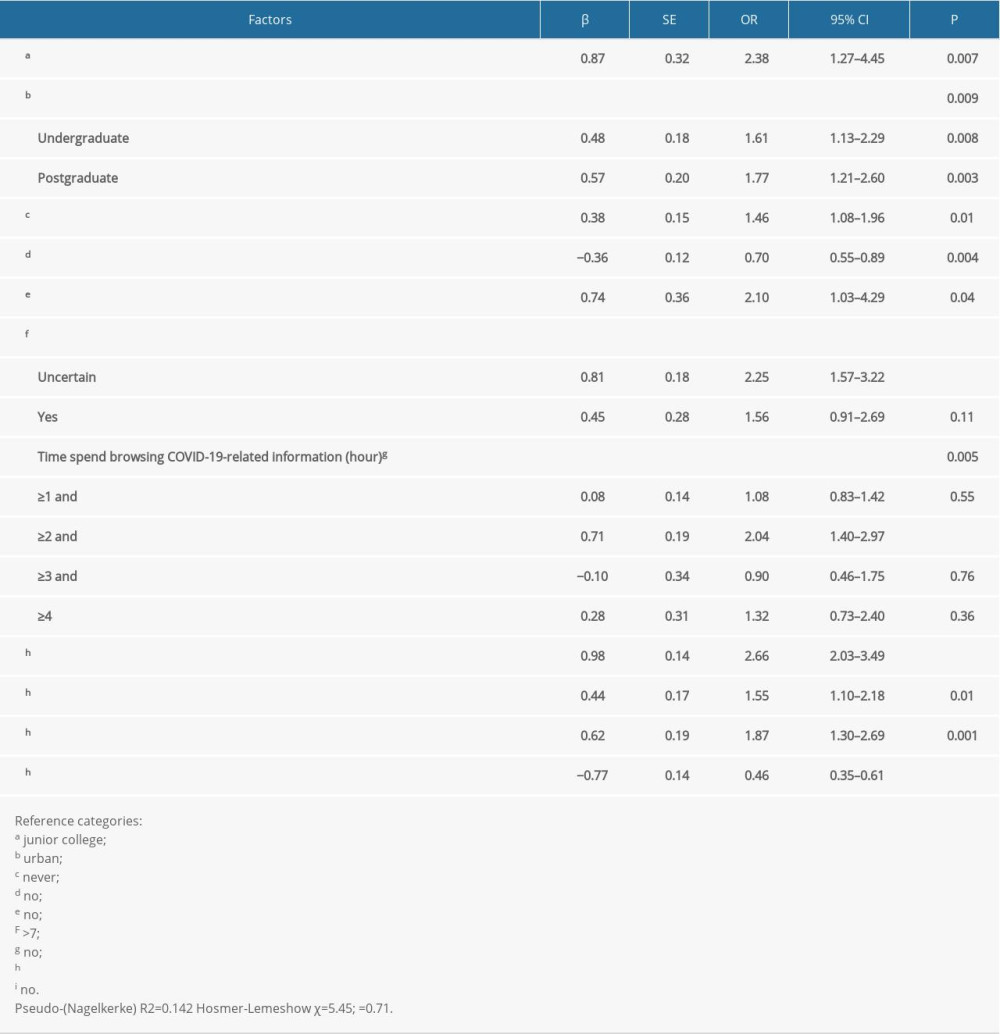
References
1. Lu R, Zhao X, Li J, Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding: Lancet, 2020; 395(10224); 565-74
2. Cook TM, Personal protective equipment during the coronavirus disease (COVID) 2019 pandemic – a narrative review: Anaesthesia, 2020; 75(7); 920-27
3. WHO: Coronavirus disease 2019–2020 https://www.who.int/emergencies/diseases/novel-coronavirus-2019
4. Yang Y, Peng F, Wang R, The deadly coronaviruses: The 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China: J Autoimmun, 2020; 109; 102434
5. Shah K, Chaudhari G, Kamrai D, How essential is to focus on physician’s health and burnout in coronavirus (COVID-19) pandemic?: Cureus, 2020; 12(4); e7538
6. Shah K, Kamrai D, Mekala H, Focus on mental health during the coronavirus (COVID-19) pandemic: Applying learnings from the past outbreaks: Cureus, 2020; 12(3); e7405
7. Zhai Y, Du X, Addressing collegiate mental health amid COVID-19 pandemic: Psychiatry Res, 2020; 288; 113003
8. Yang R, Gui X, Zhang Y, The challenge of resuming classes for young students in Wuhan, China: Expert Rev Respir Med, 2020; 14(8); 763-66
9. Jenei K, Cassidy-Matthews C, Virk P, Challenges and opportunities for graduate students in public health during the COVID-19 pandemic: Can J Public Health, 2020; 111(3); 408-9
10. Araujo FJO, de Lima LSA, Cidade PIM, Impact of Sars-Cov-2 and its reverberation in global higher education and mental health: Psychiatry Res, 2020; 288; 112977
11. Wang C, Pan R, Wan XT, Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China: Int J Environ Res Public Health, 2020; 17(5); 1729
12. Zhou SJ, Zhang LG, Wang LL, Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19: Eur Child Adolesc Psychiatry, 2020; 29(6); 749-58
13. Xie L, Luo H, Li M, The immediate psychological effects of Coronavirus Disease 2019 on medical and non-medical students in China: Int J Public Health, 2020; 65(8); 1445-53
14. Sun YY, Wang DY, Han ZT, Disease prevention knowledge, anxiety, and professional identity during COVID-19 pandemic in nursing students in Zhengzhou, China: J Korean Acad Nurs, 2020; 50(4); 533-40
15. Saraswathi I, Saikarthik J, Kumar KS, Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: A prospective longitudinal study: Peer J, 2020; 8; e10164
16. Dhar BK, Ayittey FK, Sarkar SM, Impact of COVID-19 on psychology among the university students: Glob Chall, 2020; 4(11); 2000038
17. Grubic N, Badovinac S, Johri AM, Student mental health in the midst of the COVID-19 pandemic: A call for further research and immediate solutions: Int J Soc Psychiatr, 2020; 66(5); 517-18
18. Spitzer RL, Kroenke K, Williams JB, A brief measure for assessing generalized anxiety disorder: the GAD-7: Arch Intern Med, 2006; 166(10); 1092-97
19. Kroenke K, Spitzer RL, Williams JB, The PHQ-9: Validity of a brief depression severity measure: J Gen Intern Med, 2001; 16(9); 606-13
20. Cao W, Fang Z, Hou G, The psychological impact of the COVID-19 epidemic on college students in China: Psychiatry Res, 2020; 287; 112934
21. Pan XF, Wen Y, Zhao Y, Prevalence of depressive symptoms and its correlates among medical students in China: A national survey in 33 universities: Psychol Health Med, 2016; 21(7); 882-89
22. Aker S, Midik O, The views of medical faculty students in Turkey concerning the COVID-19 pandemic: J Community Health, 2020; 45(4); 684-88
23. Wang ZH, Yang HL, Yang YQ, Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: A large cross-sectional study: J Affect Disorders, 2020; 275; 188-93
24. Wang H, Xia Q, Xiong Z, The psychological distress and coping styles in the early stages of the 2019 coronavirus disease (COVID-19) epidemic in the general mainland Chinese population: A web-based survey: PLoS One, 2020; 15(5); e0233410
25. Lei L, Huang X, Zhang S, Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in Southwestern China: Med Sci Monit, 2020; 26; e924609
26. Giammanco MD, Gitto L, Coping, uncertainty and health-related quality of life as determinants of anxiety and depression on a sample of hospitalized cardiac patients in Southern Italy: Qual Life Res, 2016; 25(11); 2941-56
27. Kmietowicz Z, Covid-19: Highest risk patients are asked to stay at home for 12 weeks: BMJ, 2020; 368; m1170
28. Yarımkaya E, Esentürk OK, Promoting physical activity for children with autism spectrum disorders during Coronavirus outbreak: Benefits, strategies, and examples: Int J Dev Disabil, 2020; 1-6
29. Huang Y, Zhao N, Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey: Psychiatry Res, 2020; 288; 112954
30. Torales J, O’Higgins M, Castaldelli-Maia JM, The outbreak of COVID-19 coronavirus and its impact on global mental health: Int J Soc Psychiatr, 2020; 66(4); 317-20
31. Jo W, Lee J, Park J, Online information exchange and anxiety spread in the early stage of the novel coronavirus (COVID-19) outbreak in South Korea: Structural topic model and network analysis: J Med Internet Res, 2020; 22(6); e19455
32. Park CL, Russell BS, Fendrich M, Americans’ COVID-19 stress, coping, and adherence to CDC guidelines: J Gen Intern Med, 2020; 35(8); 2296-303
33. Taghrir MH, Borazjani R, Shiraly R, COVID-19 and Iranian medical students; A survey on their related-knowledge, preventive behaviors and risk perception: Arch Iran Med, 2020; 23(4); 249-54
34. Ozdin S, Bayrak Ozdin S, Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender: Int J Soc Psychiatr, 2020; 66(5); 504-11
35. Abd-Alrazaq A, Alhuwail D, Househ M, Top concerns of tweeters during the COVID-19 pandemic: Infoveillance study: J Med Internet Res, 2020; 22(4); e19016
36. Yang H, Bin P, He AJ, Opinions from the epicenter: an online survey of university students in Wuhan amidst the COVID-19 outbreak1: Journal of Chinese Governance, 2020; 5(2); 234-48
37. Liao Q, Yuan J, Dong M, Public engagement and government responsiveness in the communications about COVID-19 during the early epidemic stage in China: Infodemiology study on social media data: J Med Internet Res, 2020; 22(5); e18796
38. Pather N, Blyth P, Chapman JA, Forced disruption of anatomy education in Australia and New Zealand: An acute response to the COVID-19 pandemic: Anat Sci Educ, 2020; 13(3); 284-300
39. Akers A, Blough C, Iyer MS, COVID-19 implications on clinical clerkships and the residency application process for medical students: Cureus, 2020; 12(4); e7800
40. Sahu P, Closure of universities due to coronavirus disease 2019 (COVID-19) : Impact on education and mental health of students and academic staff: Cureus, 2020; 12(4); e7541
41. Li W, Yang Y, Liu ZH, Progression of mental health services during the COVID-19 outbreak in China: Int J Biol Sci, 2020; 16(10); 1732-38
42. Lueck JA, Poe M, Bypassing the waitlist: examining barriers and facilitators of help-line utilization among college students with depression symptoms: J Ment Health, 2020 [Online ahead of print]
43. Cheng H-L, Wang C, McDermott RC, Self-stigma, mental health literacy, and attitudes toward seeking psychological help: Journal of Counseling & Development, 2018; 96(1); 64-74
Tables
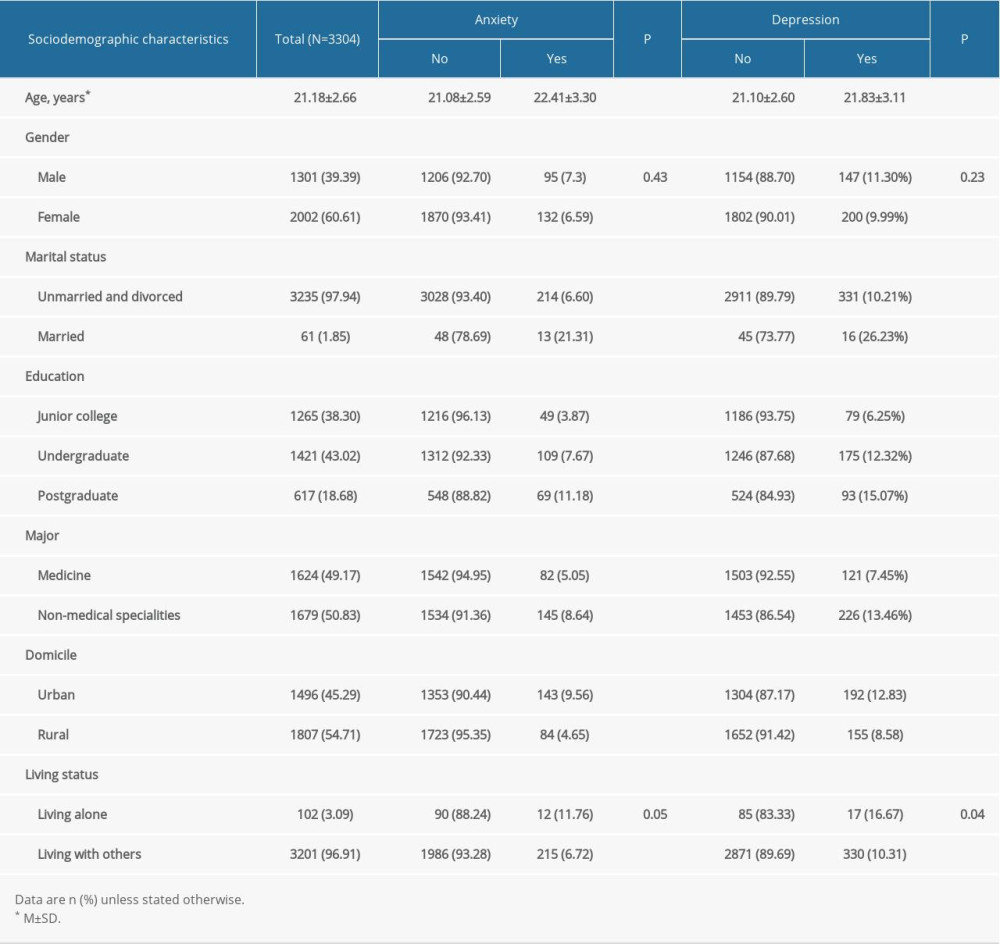 Table 1. Sociodemographic characteristics.
Table 1. Sociodemographic characteristics.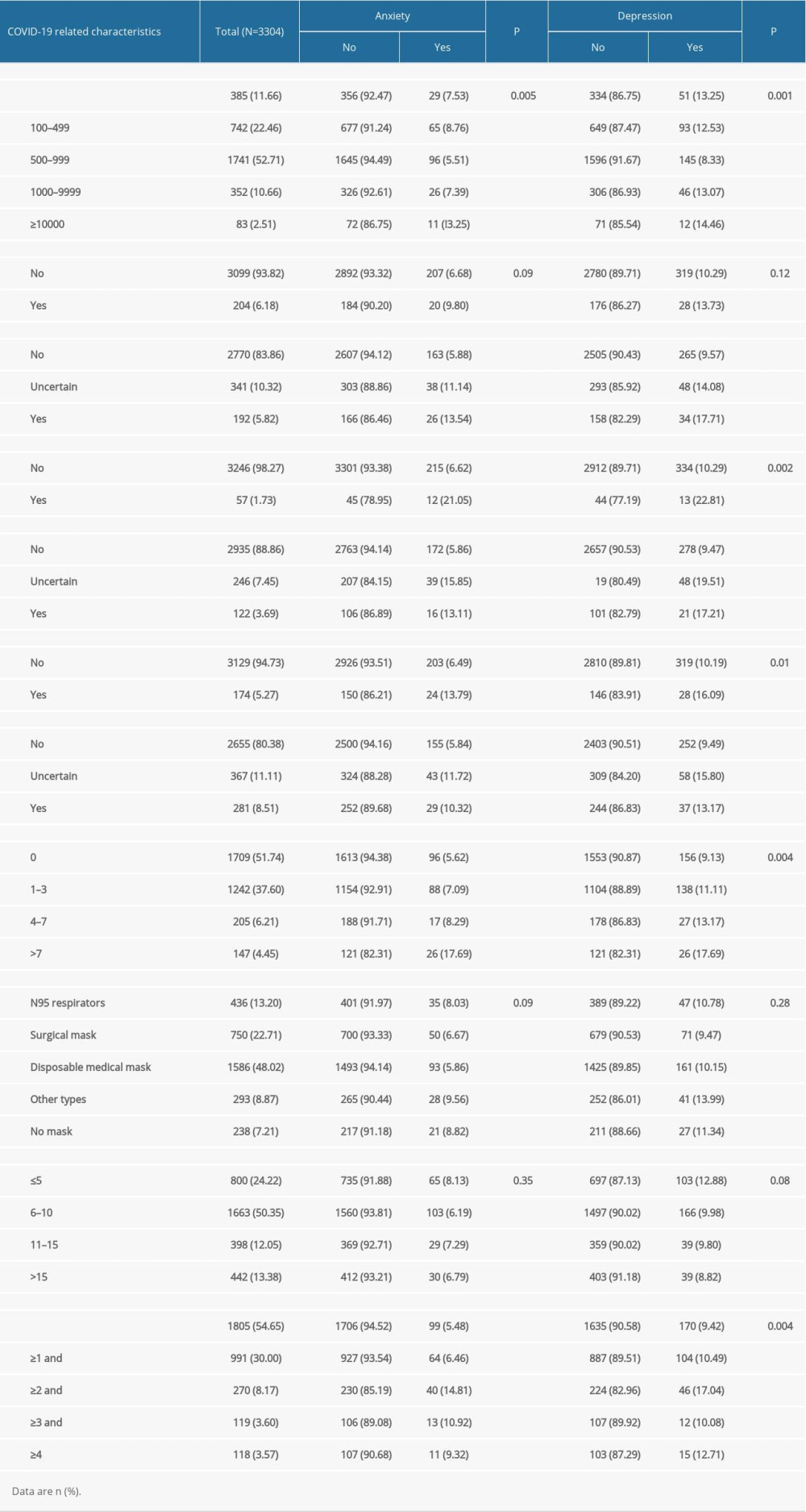 Table 2. COVID-19 related characteristics.
Table 2. COVID-19 related characteristics.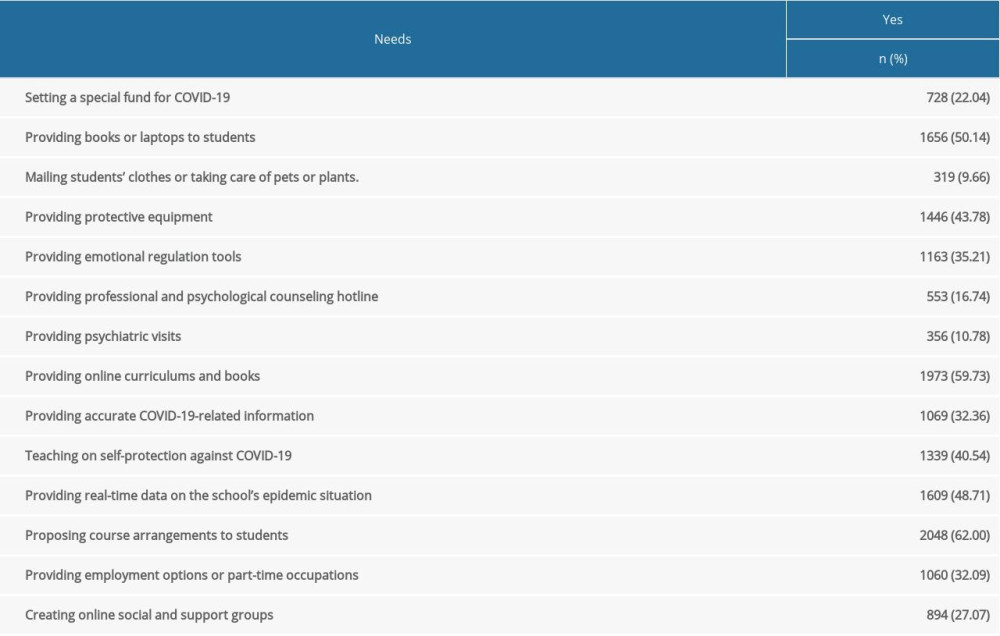 Table 3. The needs of school support (N=3304).
Table 3. The needs of school support (N=3304). Table 4. Anxiety, depression among college students (N=3304).
Table 4. Anxiety, depression among college students (N=3304).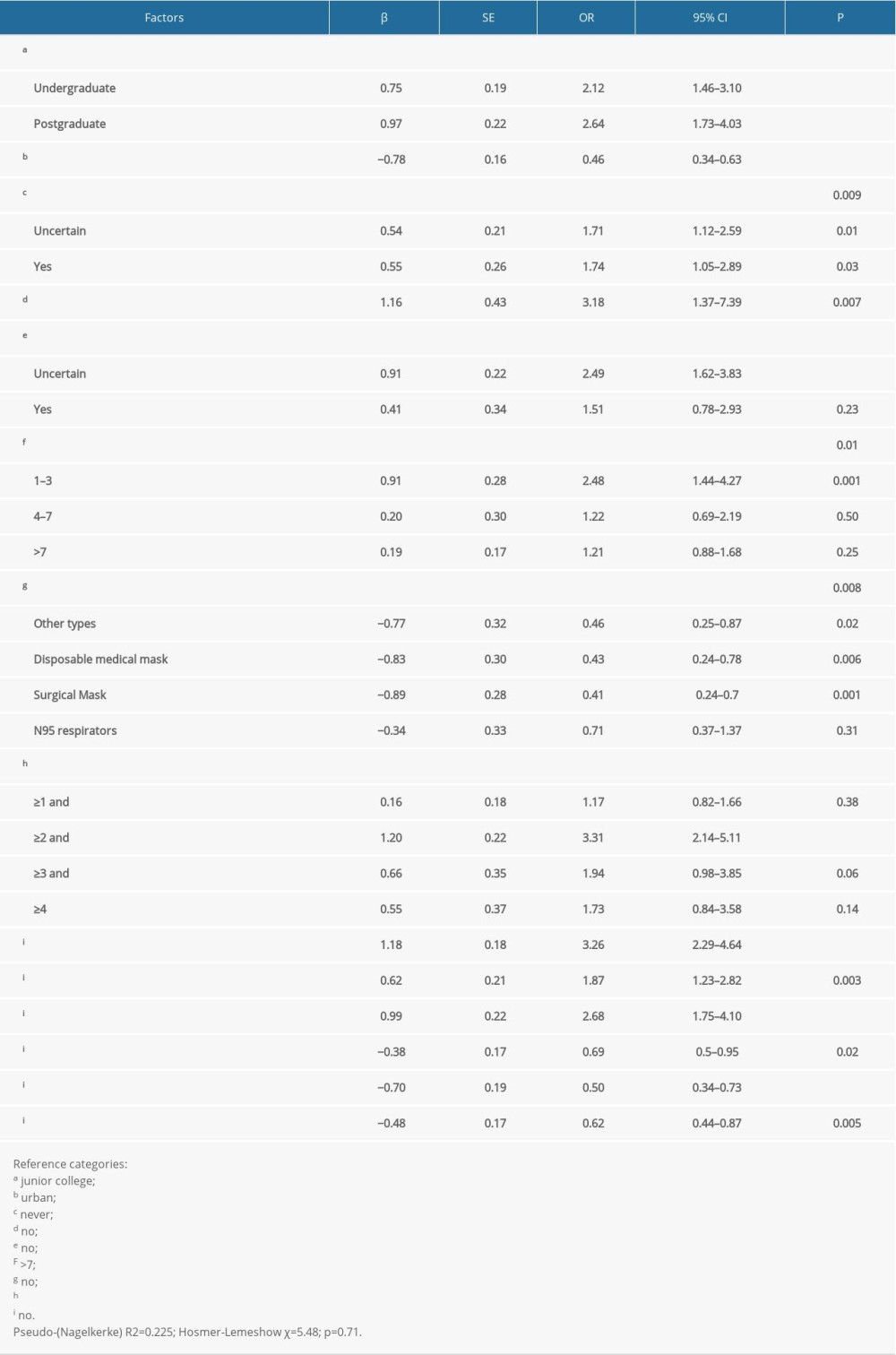 Table 5. The logistics regression model of anxiety (N=3304).
Table 5. The logistics regression model of anxiety (N=3304).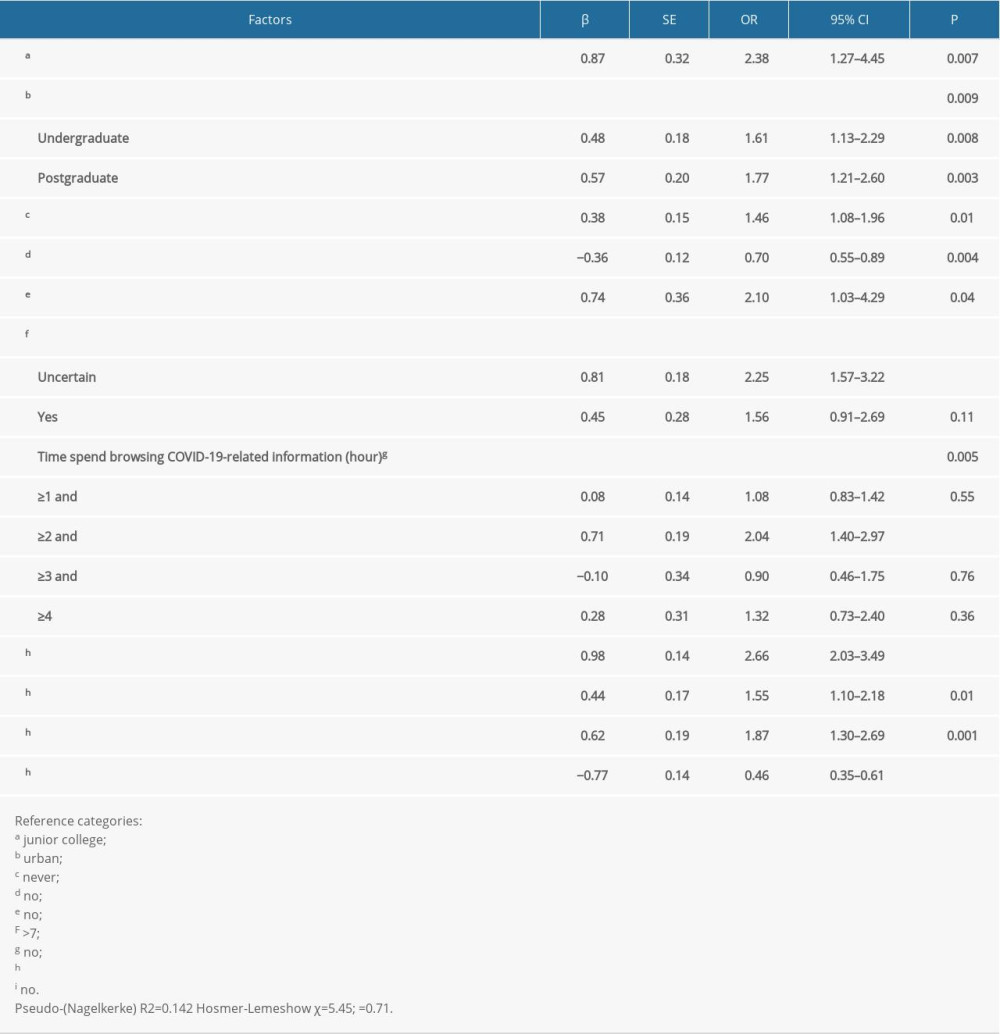 Table 6. The logistics regression model of depression (N=3304).
Table 6. The logistics regression model of depression (N=3304). In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








