18 August 2020: Clinical Research
Root Anatomy and Root Canal Morphology of Maxillary Second Permanent Molars in a Chongqing Population: A Cone-Beam Computed Tomography Study
Yu Xia123CDEF, Xin Qiao123BC, Ya-jing Huang123CD, Yue-heng Li123AE*, Zhi Zhou123AGDOI: 10.12659/MSM.922794
Med Sci Monit 2020; 26:e922794
Abstract
BACKGROUND: To investigate variations in the anatomy of root canals in permanent second molars of the upper jaw in a population in Chongqing, China, using cone-beam computed tomography (CBCT).
MATERIAL AND METHODS: CBCT imaging data of 400 second permanent molars of the upper jaws of 200 patients were retrospectively reviewed. Patients’ gender, age, numbers of roots and canals, root fusion of permanent second molars of the maxilla on both sides, and morphological categories of root canals of mesiobuccal roots were recorded. The distances from the apices of the distobuccal and mesiobuccal roots to the buccal bone plate were measured.
RESULTS: Of the 400 permanent second maxillary molars, 312 (78.0%) had three roots and 247 (61.75%) had three canals. Fused roots were observed in 126 (31.5%) teeth; of these, 67 (53.2%) had three canals and 44 (34.9%) had two canals. Morphologically, 297 (74.25%), 29 (7.25%), nine (2.25%) and 65 (16.25%) teeth had type I, II, III, and IV mesiobuccal root canals, respectively, with 103 (25.75%) having secondary mesiobuccal canals. The distances from the apices of the mesiobuccal, distobuccal, and single buccal roots to the surface of the buccal osseous lamella were 7.34±1.89 mm, 6.26±1.74 mm, and 8.60±2.56 mm, respectively.
CONCLUSIONS: The root form and canal shape of permanent second molars of the upper jaw varied greatly among the population of Chongqing, China. CBCT is a valuable method for assessing the complex anatomic morphology of teeth.
Keywords: Cone-Beam Computed Tomography, Tooth, Tooth Root, Maxilla, Molar, young adult
Background
Pulpal and periapical diseases are the most common types of dental diseases. Teeth with these conditions frequently undergo root canal treatment, which plays a significant role in preserving natural teeth [1,2]. The success of endodontic therapy depends on the complete removal of infected substances from the root canal system, the elimination of sources of infection, and tight filling of the root canal system, preventing reinfection by microorganisms [3,4]. Root canals that have not been completely treated or are missed are the main causes of failure of endodontic therapy [5,6]. The configuration of root canals in human teeth is quite complicated and varies among different populations and races [3,7,8]. However, the complexity of the internal anatomical structure is usually masked by the relatively simple external anatomy [9].
The second molars of the upper jaw have the most intricate root canal system in human teeth [10,11]. The rate of occurrence of a secondary mesiobuccal canal (MB2) in permanent second molars of the upper jaw have been reported to be as high as 93.7% [12], and the likelihood of having two palatal canals was found to range from 1.37% to 6.34% [13,14]. A study of distobuccal roots found that the likelihood of having two canals in the mesiodistal direction was 4%, whereas the likelihood of having two canals in the buccolingual direction was 6% [15]. These findings indicate that complete comprehension of the anatomic structure of roots and canals can guide their treatment.
Among the methods currently used to assess the configuration of canal systems are the diaphanization technique, dental hard tissue sectioning, X-ray imaging, micro-computed tomography (micro-CT) imaging and cone-beam computed tomography (CBCT) [3,9,15–21]. Although the diaphanization technique and dental hard tissue sectioning can accurately determine the anatomy of root canals, these methods can only be used to study isolated dental specimens, which may destroy the integrity of these teeth [15,17]. X-ray imaging has been utilized traditionally to determine root canal anatomy, but this method produces two-dimensional (2D) images of three-dimensional (3D) objects, resulting in distortion and overlap. X-ray images therefore cannot accurately reflect the morphological features of canals and their anatomic correlation with neighboring tissue [18]. Micro-CT does not damage specimens, with image reconstruction even determining the fine anatomical structure of root canals [20]. However, scanning time is long and patients are exposed to high doses of radiation, limiting the application of micro-CT to studies investigating extracted teeth [20,21]. CBCT, first utilized in endodontic research in 1990, has several advantages when compared with micro-CT, including a shorter scanning time and exposure to lower doses of radiation [22]. CBCT can therefore provide clear and accurate 3D reconstructed images of root canal systems without damaging the dental structure [23,24]. CBCT has been used to assess the morphology of root canal systems
Material and Methods
SUBJECTS:
The study protocol was approved by the Ethics Committee of Stomatological Hospital Affiliated to Chongqing Medical University (2019-74). Patients who required CBCT for the diagnosis and treatment of maxillofacial trauma, for orthodontic treatment, and for implant restoration at the Stomatological Hospital Affiliated to Chongqing Medical University from January 2018 through April 2018, inclusive, were randomly selected. CBCT imaging data, age and gender were recorded. Subjects were included if 1) they or their guardians provided written informed consent for the use of their CBCT imaging data; 2) they were not missing bilateral maxillary second permanent molars; 3) the development of the root apex was complete; 4) maxillary second permanent molars were not restored with dental filling materials or crowns due to carious or noncarious lesions of hard dental tissues; 5) there was no evidence of root resorption or inflammation in tissue surrounding the bone; 6) they did not undergo root canal treatment and did not show root canal calcification or resorption; and 7) their CBCT images were clear with high resolution and no artifacts. Subjects were excluded if 1) they or their guardians refused consent for the use of CBCT imaging data; 2) maxillary second permanent molars were missing on one or both sides; 3) root apices were open and flared in shape; 4) maxillary second permanent molars had been restored with dental filling materials or crowns; 5) root resorption and/or inflammation were observed in tissue surrounding the bone; 6) they had undergone root canal treatment and showed root canal calcification or resorption; or 7) the collected CBCT images were unclear.
CBCT EQUIPMENT AND SCANNING:
CBCT scans were performed using an i-CAT CBCT scanner (I-CAT Vision; Imaging Science International, Hatfield, PA, USA) with a voltage of 120 kV, a current of 5 mA, a voxel resolution of 0.4×0.4 mm, and an exposure time of 8–9 s. The scanning data were converted to DICOM format and entered into the i-CAT software for three-dimensional reconstruction. All scans were performed strictly in accordance with the technical manual of the instrument, and all images were reviewed by an experienced radiographer.
IMAGING ANALYSIS:
All CBCT images were independently evaluated by an experienced endodontist. To insure the credibility of the endodontist’s assessment, 50 images were randomly selected and reviewed by the same endodontist at two different time points according to the evaluation criteria. The consistency and reliability of results observed at different times were determined with Kappa statistics. Kappa values of 0.61–0.8 (substantial agreement) indicated that assessment by the observer of the tissue surrounding the area of the procedure was reliable. The CBCT images of the permanent second molars of the upper jaw were evaluated on both sides in the coronal, axial and sagittal planes. Other factors analyzed included subject gender, age, number of roots, fused roots and canals, morphological categories of canals of the mesiobuccal root and the distances from the apices of the distobuccal and mesiobuccal roots to the buccal bone plate. Canal morphology was assessed using Vertucci’s classification (Figure 1) [3,10].
STATISTICAL ANALYSIS:
Categorical variables were reported as number (%) and compared using the chi-square test or Fisher’s exact test, as appropriate. Differences in distances from the apices of the distobuccal and mesiobuccal roots to the buccal osseous lamella between genders and right and left teeth were compared using the rank sum test, and differences in distances from the apex of a single buccal root to the buccal bone plate between genders and right and left teeth were analyzed by two-sample independent t-tests. All statistical analyses were performed using SPSS22.0 software, with the significance level set at α=0.05.
Results
NUMBER OF ROOTS:
Of the 400 permanent second molars of the upper jaw, 312 (78.0%) had three roots, 49 (12.25%) had two roots, and 39 (9.75%) had one root (Table 1; Figure 1B1–1B3). None of these teeth had four roots. There were no significant differences in the occurrence rates of numbers of roots between men and women or between teeth on the left and right sides (P>0.05 each).
NUMBER OF ROOT CANALS:
Of the 400 teeth, five (1.25%), 45 (11.25%) 247 (61.75%) and 103 (25.75%) had one, two, three and four root canals, respectively (Table 2). These percentages did not differ significantly in men and women or between teeth on the left and right sides (P>0.05 each).
RATES OF ROOT FUSION AND NUMBER OF CANALS IN TEETH WITH FUSED ROOTS:
Root fusion was present in 126 (31.50%) teeth (Table 3), with no significant differences in rate of root fusion between men and women or between teeth on the left and right sides (P>0.05 each). Of the 126 teeth with fused roots, five (3.97%), 44 (34.92%), 67 (53.17%) and ten (7.94%) had one, two, three and four root canals, respectively (Figure 1C1–1F3), with no significant differences between men and women or between teeth on the left and right sides (P>0.05 each).
RATES OF MB2 AND MORPHOLOGICAL CANAL CATEGORIES OF MESIOBUCCAL ROOTS:
Based on the Vertucci classification of root canals, 297 (74.25%), 29 (7.25%), nine (2.25%) and 65 (16.25%) permanent second molars of the upper jaw had type I, II, III, and IV mesiobuccal root canals, respectively (Figure 2A–2D3; Table 4). These rates did not differ significantly in men and women mesiobuccal root between genders or between teeth on the left and right sides (P>0.05 each). Of these 400 teeth, 103 (25.75%) had MB2 canals (Table 5), with the rate being markedly higher in men than in women (P=0.007). In contrast, these rates were similar in teeth on the right and left sides (p>0.05).
DISTANCES FROM THE APICES OF THE DISTOBUCCAL AND MESIOBUCCAL ROOTS TO THE BUCCAL SURFACE OF THE OSSEOUS LAMELLA:
The mean distances from the apices of the mesiobuccal, distobuccal, and single buccal roots to the buccal surface of the bone lamella were 7.34±1.89 mm, 6.26±1.74 mm, and 8.60±2.56 mm, respectively (Figure 2E1–2E3, Table 6). The distance from the mesiobuccal apex to the buccal bone plate was significantly greater than the distance from the distobuccal root apex to the buccal bone plate (P<0.05). The distance from the mesiobuccal apex and the disiobuccal apex to the buccal bone plate on the right and left sides also differed significantly (P<0.05). The distances from the single buccal apices to the buccal bone plate, however, did not differ significantly in men and women or in teeth on the right and left sides (P>0.05 each).
Discussion
Successful root canal treatment depends on familiarity with the anatomic morphology of the root canal system in each individual tooth [25]. Anatomic morphology can be determined by completely removing the injured tissue inside the root canals and tightly filling the root canal system [4,26]. Because incompletely filled or missed root canals can lead to microbial recolonization and trigger inflammation [27], careful clinical and imaging examinations are essential for high-quality root canal treatment. CBCT has been extensively used to examine the morphological structure of roots and canals due to its ability to acquire high-resolution 3D images and the lack of image distortion [13,14,23–25]. The guidelines of the American Association of Endodontists and of the American Academy of Maxillofacial Radiology have recommended the use of CBCT for the diagnosis and treatment of teeth that may have additional canals or complex anatomy [28]. CBCT, however, is more expensive than 2-dimensional X-rays, suggesting the need for a risk/benefit assessment prior to using CBCT. Because it is necessary to determine whether the risk of exposure to radiation is less than the potential benefits to patients, CBCT should not be used routinely in clinical practice [29]. The present study analyzed CBCT imaging data from patients who had been assessed by CBCT for diagnosis and treatment.
Analysis of 400 permanent second molars of the upper jaw in a Chongqing population showed that 78.0% had three roots, whereas 12.25% had two and 9.75% had one root, with none of these teeth having four roots. Moreover, 61.75% of these teeth had three canals, 25.75% had four canals, 11.25% had two canals, and 1.25% had one canal. In addition, 25.75% of these teeth had MB2; of these, 28.2%, 8.7%, and 63.1% had types II, III, and IV, respectively. These results were similar to those of previous studies (Tables 7, 8) [30,31]. Population-based CBCT studies in China, Iran, India, Thailand, Greece, Brazil, Spain, Portugal, Egypt, and North Korea have shown that the percentages of permanent second molars of the upper jaw with three roots ranged from 45.1% to 93.1%, with 4.2% to 13.2% of these teeth having two roots, 0.9% to 16.9% having one root, and from 0% to 1.24%, having four roots (Table 7) [14,21,30,32–37]. Moreover, the prevalence of MB2 ranged from 19.2% to 78.9% (Table 8) [14,15,30–35,37–44]. A study of an Iranian population found that 67.5% of permanent second molars of the upper jaw had four canals, followed by 31.2% with three canals and 1.3% with five canals, with none of these teeth having one or two root canals [45]. These differences in root and canal numbers and MB2 percentages may be associated with racial background, research techniques, images and sample sizes. The scanning resolution of CBCT in the present study was 400 μm, which is considered a study limitation. The prevalence of MB2 determined by the diaphanization technique and dental hard tissue sectioning was found to be higher than that determined using conventional X-rays and CBCT [38,40,41,43].
This study found that the occurrence of MB2 was significantly higher in men than in women (32.6%
This study also found that the rate of root fusion in permanent second molars of the upper jaw was 31.5%, with 53.2% of these teeth having three canals. A micro-CT evaluation of 187 extracted second molars of the upper jaw in a Chinese population found fused roots in 42.25% [47], much higher than in our study. Micro-CT may provide higher resolution 3D images than CBCT. However, the rate of root fusion in second permanent molars of the upper jaw in our study was markedly higher than rates in Korean (10.7%) and Iranian (8.8%) populations [36,48]. This difference may be due to different definitions of fused roots. Roots in the present study were defined as fused roots when the distance from the cementoenamel junction (CEJ) to the lower point of root fusion was not less than 70% of the distance from the CEJ to the apex of the root [47]. In contrast, earlier studies regarded fusion extending over the entire root surface as a fused root.
Apical microsurgery should be considered when the infected tissue in the apical part of the canal cannot be eliminated completely. Apical surgery is usually performed through a buccal approach, with accurate positioning of the apex being a prerequisite for successful apical surgery [49]. The distance from the apex of the buccal root to the surface of the bone plate is an important reference for localization of the apex. In the present study, the mean horizontal distances from the apices to the buccal surface of the osseous lamella were 7.34±1.89 mm for the mesiobuccal and 6.26±1.74 mm for the distobuccal roots, similar to previous findings [50]. These results indicated that the distance from the distobuccal root apex to the buccal surface of the osseous lamella was significantly lower than the distance from the mesiobuccal root to the buccal surface of the osseous lamella (P<0.05). The distance from the buccal apex to the buccal surface of the osseous lamella in permanent second molars of the maxilla with only one buccal root was 8.60±2.56 mm, with the buccal apical position being more lingual than teeth with mesiobuccal and distobuccal roots. Because few permanent second molars of the upper jaw in our study had only one buccal root, further research with a larger sample size is needed to confirm the results. The distances from the apices to the buccal surface of the osseous lamella can be used as references to locate the buccal root apex of second molars of the upper jaw during surgery. These distances can provide an anatomical basis for apical surgery and are essential to prevent excessive bone removal, deep drilling, and damage to the root apices.
Conclusions
Most permanent second molars of the upper jaw in subjects from Chongqing had three roots and three canals. According to Vertucci’s classification, type IV was the most common anatomic morphology of the mesiobuccal roots of permanent second molars of the maxilla when MB2 was present. The distance from the apex of the distobuccal root to the buccal surface of the osseous lamella plate was significantly lower than the distance from the apex of the mesiobuccal root to the buccal surface. These findings indicate that the anatomic morphology of roots and canals of maxillary permanent second molars of patients from Chongqing vary considerably. These results can help in understanding the root and canal configuration of second molars of the maxilla, improving success rates of endodontic treatment and apical surgery. Moreover, these findings showed that CBCT is effective in assessing the complex anatomical morphology of teeth.
Figures
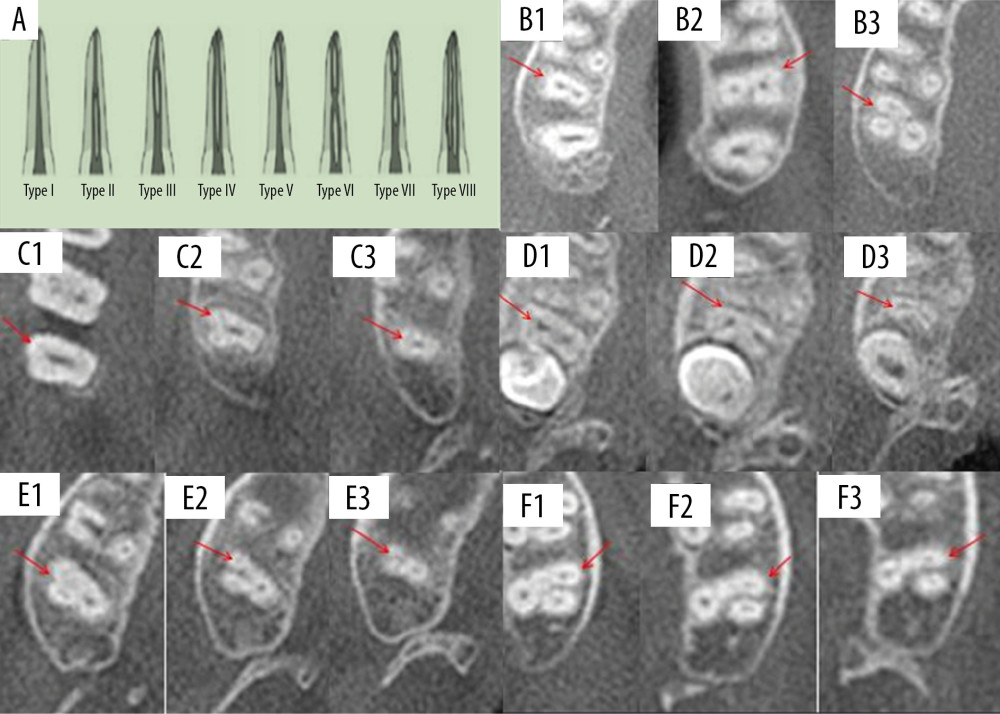 Figure 1. Schematic diagrams showing Vertucci’s classification of root canal morphology and canal configuration of permanent second molars of the upper jaw with fused roots. (A) Classification of the anatomic morphology of canals. (B) Teeth with one (B1), two (B2), and three (B3) roots. (C) Fused root with one root canal (C1, coronal 1/3; C2, middle 1/3; and C3, apical 1/3). (D) Fused root with two root canals (D1, coronal 1/3; D2, middle 1/3; D3, apical 1/3). (E) Fused root with three root canals (E1, coronal 1/3; E2, middle 1/3; E3, apical 1/3). (F) Fused root with four root canals (F1, coronal 1/3; F2, middle 1/3; F3, apical 1/3).
Figure 1. Schematic diagrams showing Vertucci’s classification of root canal morphology and canal configuration of permanent second molars of the upper jaw with fused roots. (A) Classification of the anatomic morphology of canals. (B) Teeth with one (B1), two (B2), and three (B3) roots. (C) Fused root with one root canal (C1, coronal 1/3; C2, middle 1/3; and C3, apical 1/3). (D) Fused root with two root canals (D1, coronal 1/3; D2, middle 1/3; D3, apical 1/3). (E) Fused root with three root canals (E1, coronal 1/3; E2, middle 1/3; E3, apical 1/3). (F) Fused root with four root canals (F1, coronal 1/3; F2, middle 1/3; F3, apical 1/3). 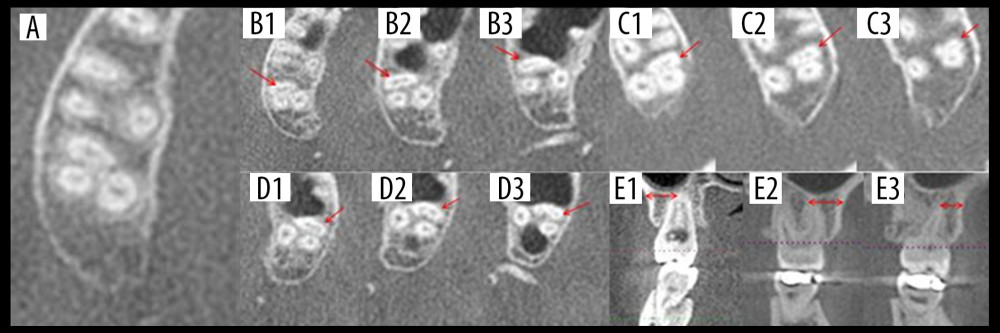 Figure 2. Types of canal configuration in mesiobuccal roots of permanent second molars of the upper jaw and horizontal distances from the buccal root apices to the surface of buccal cortical bone plate. (A) Type I. (B) Type II (B1, coronal 1/3; B2, middle 1/3; B3, apical 1/3). (C) Type III (C1, coronal 1/3; C2, middle 1/3; C3, apical 1/3). (D) Type IV (D1, coronal 1/3; D2, middle 1/3; D3, apical 1/3). (E) Horizontal distances from single buccal root (E1), mesiobuccal root (E2), and distobuccal root (E3) apices to the surface of the buccal cortical bone plate.
Figure 2. Types of canal configuration in mesiobuccal roots of permanent second molars of the upper jaw and horizontal distances from the buccal root apices to the surface of buccal cortical bone plate. (A) Type I. (B) Type II (B1, coronal 1/3; B2, middle 1/3; B3, apical 1/3). (C) Type III (C1, coronal 1/3; C2, middle 1/3; C3, apical 1/3). (D) Type IV (D1, coronal 1/3; D2, middle 1/3; D3, apical 1/3). (E) Horizontal distances from single buccal root (E1), mesiobuccal root (E2), and distobuccal root (E3) apices to the surface of the buccal cortical bone plate. Tables
Table 1. Numbers of roots.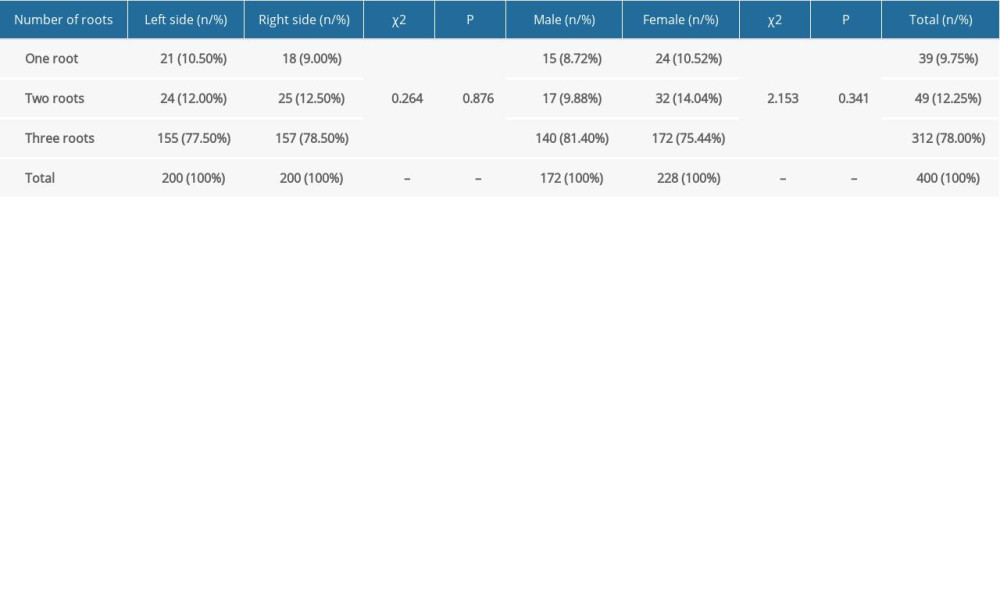 Table 2. Numbers of root canals.
Table 2. Numbers of root canals.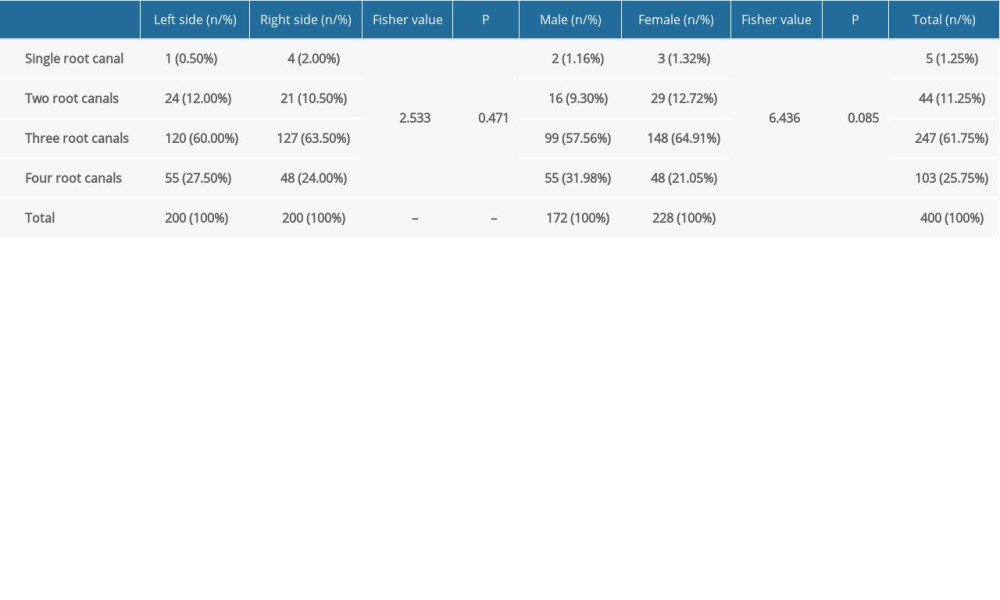 Table 3. Rates of root fusion.
Table 3. Rates of root fusion.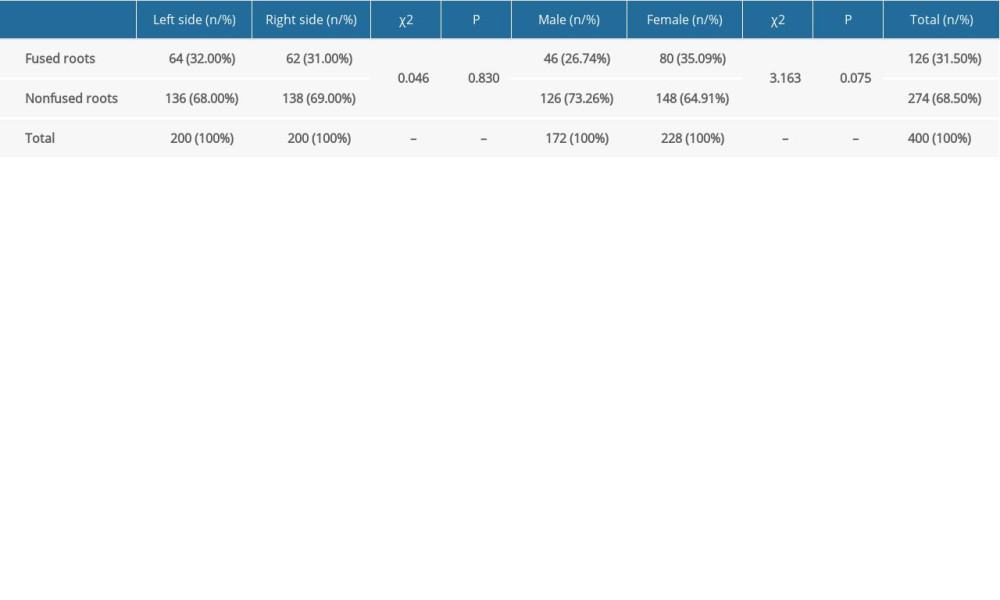 Table 4. Root canal configurations of mesiobuccal roots.
Table 4. Root canal configurations of mesiobuccal roots.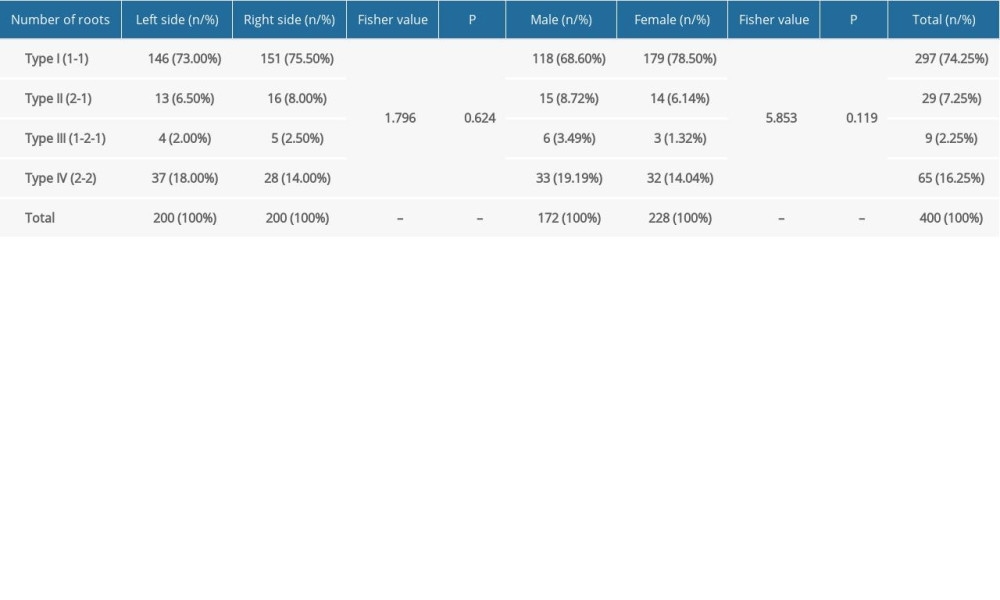 Table 5. Prevalence of MB2 canals
Table 5. Prevalence of MB2 canals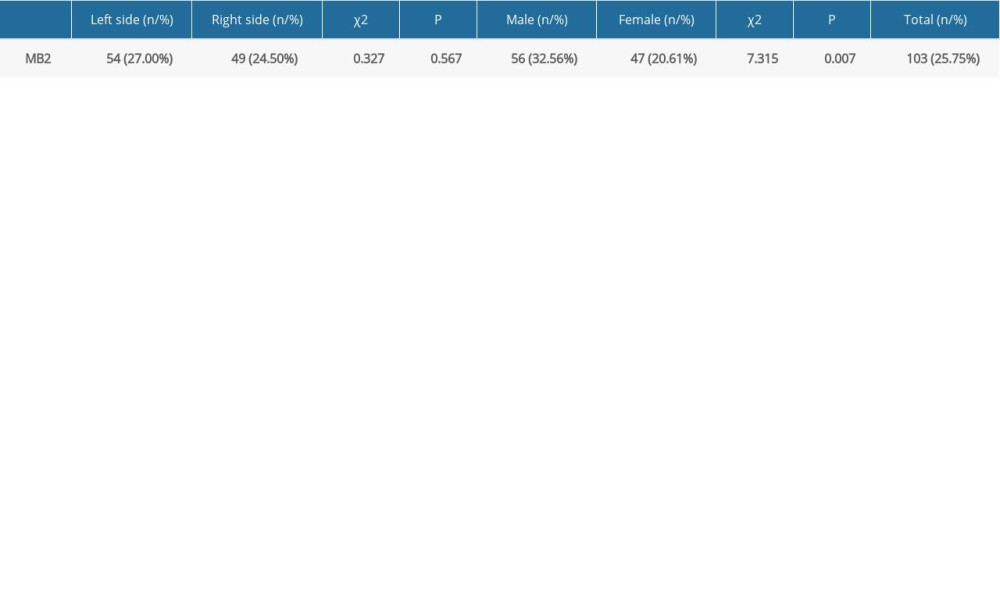 Table 6. Distances from the buccal root apices to the surface of the buccal cortical bone plate.
Table 6. Distances from the buccal root apices to the surface of the buccal cortical bone plate.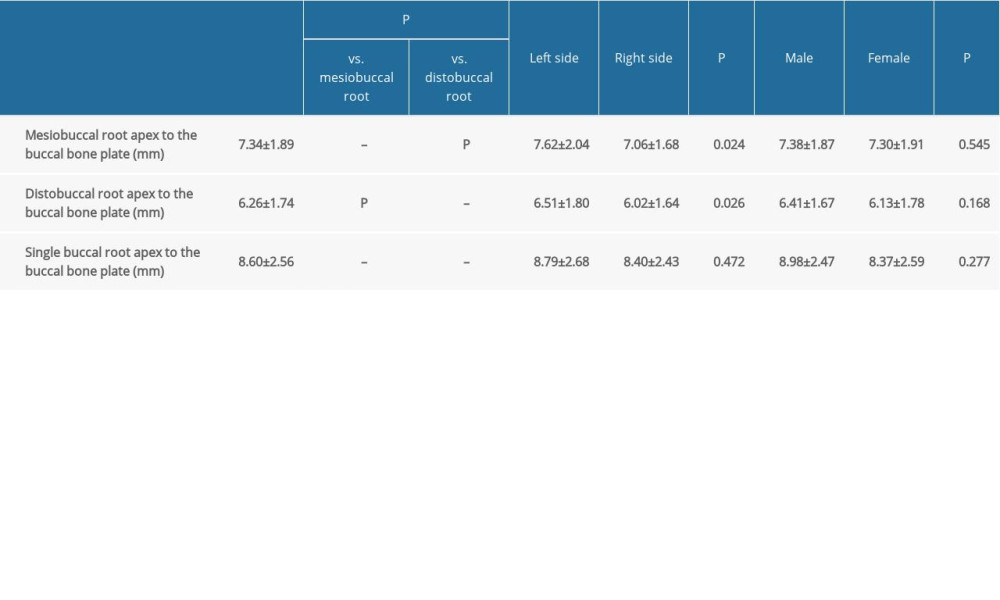 Table 7. Numbers of roots in maxillary permanent second molars reported in previous studies.
Table 7. Numbers of roots in maxillary permanent second molars reported in previous studies. Table 8. Rates of MB2 and root canal configurations of the mesiobuccal roots of the maxillary permanent second molars reported in previous studies.
Table 8. Rates of MB2 and root canal configurations of the mesiobuccal roots of the maxillary permanent second molars reported in previous studies.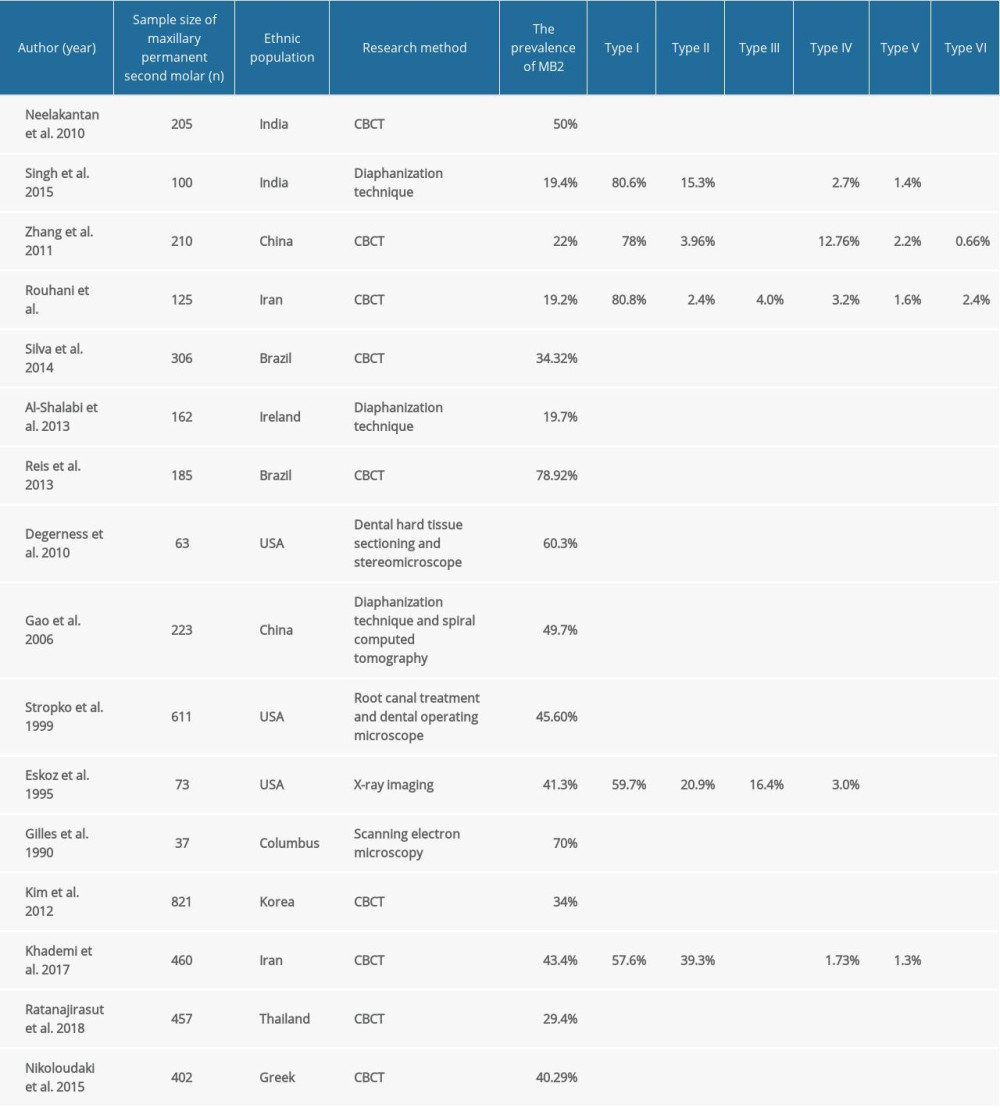
References
1. Lee CB, Chang YH, Wen PC, Li CY, Association of failed root canal treatment with dentist and institutional volumes: A population-based cohort study in Taiwan: J Endod, 2017; 43; 1628-34
2. Raedel M, Hartmann A, Bohm S, Walter MH, Three-year outcomes of root canal treatment: Mining an insurance database: J Dent, 2015; 43; 412-17
3. Vertucci FJ, Root canal morphology and its relationship to endodontic procedure: Endodontic Topics, 2005; 10; 3-29
4. Azim AA, Griggs JA, Huang GTJ, The Tennessee Study: Factors affecting treatment outcome and healing time following nonsurgical root canal treatment: Int Endod J, 2016; 49; 6-16
5. England MC, Hartwell GR, Lance JR, Detection and treatment of multiple canals in mandibular premolars: J Endod, 1991; 17; 174-78
6. Slowey RR, Root canal anatomy. Road map to successful endodontics: Dent Clin North Am, 1979; 23; 555-73
7. Altunsoy M, Ok E, Nur BG, Root canal morphology analysis of maxillary permanent first and second molars in a southeastern Turkish population using cone-beam computed tomography: J Dent Sci, 2015; 10; 401-7
8. Neelakantan P, Subbarao C, Subbarao CV, Ravindranath M, Root and canal morphology of mandibular second molars in an Indian population: J Endod, 2010; 36; 1319-22
9. Ng YL, Aung TH, Alavi A, Gulabivala K, Root and canal morphology of Burmese maxillary molars: Int Endod J, 2001; 34; 620-30
10. Zeng C, Shen Y, Guan X, Rare root canal configuration of bilateral maxillary second molar using cone-beam computed tomographic scanning: J Endod, 2016; 42; 673-77
11. Nosrat A, Verma P, Hicks ML, Variations of palatal canal morphology in maxillary molars: A case series and literature review: J Endod, 2017; 43; 1888-96
12. Schwarze T, Baethge C, Stecher T, Geurtsen W, Identification of second canals in the mesiobuccal root of maxillary first and second molars using magnifying loupes or an operating microscope: Aust Endod J, 2002; 28; 57-60
13. Tian XM, Yang XW, Qian L, Analysis of the root and canal morphologies in maxillary first and second molars in a Chinese population using cone-beam computed tomography: J Endod, 2016; 42; 696-701
14. Neelakantan P, Subbarao C, Ahuja R, Cone-beam computed tomography study of root and canal morphology of maxillary first and second molars in an Indian population: J Endod, 2010; 36; 1622-27
15. Singh S, Pawar M, Root canal morphology of South Asian Indian maxillary molar teeth: Eur J Dent, 2015; 9; 133-44
16. Alavi AM, Opasanon A, Ng YL, Gulabivala K, Root and canal morphology of Thai maxillary molars: Int Endod J, 2002; 35; 478-85
17. Alhadainy HA, Canal configuration of mandibular first premolars in an Egyptian population: J Adv Res, 2013; 4; 123-28
18. Paes da Silva Ramos Fernandes LM, Rice D, Ordinola-Zapata R, Detection of various anatomic patterns of root canals in mandibular incisors using digital periapical radiography, 3 cone-beam computed tomographic scanners, and micro-computed tomographic imaging: J Endod, 2014; 40; 42-45
19. Chen J, Li X, Su Y, A micro-computed tomography study of the relationship between radicular grooves and root canal morphology in mandibular first premolars: Clin Oral Investig, 2015; 19; 329-34
20. Domark JD, Hatton JF, Benison RP, Hildebolt CF: J Endod, 2013; 39; 901-5
21. Ghobashy AM, Nagy MM, Bayoumi AA, Evaluation of root and canal morphology of maxillary permanent molars in an Egyptian population by cone-beam computed tomography: J Endod, 2017; 43; 1089-92
22. Tachibana H, Matsumoto K, Applicability of X-ray computerized tomography in endodontics: Endod Dent Traumatol, 1990; 6; 16-20
23. Kiarudi AH, Eghbal MJ, Safi Y, The applications of cone-beam computed tomography in endodontics: A review of literature: Iran Endod J, 2015; 10; 16-25
24. Patel S, Dawood A, Whaites E, Pitt Ford T, New dimensions in endodontic imaging: Part 1. Conventional and alternative radiographic systems: Int Endod J, 2009; 42; 447-62
25. Celikten B, Tufenkci P, Aksoy U, Cone beam CT evaluation of mandibular molar root canal morphology in a Turkish Cypriot population: Clin Oral Investig, 2016; 20; 2221-26
26. Al-Qudah AA, Awawdeh LA, Root and canal morphology of mandibular first and second molar teeth in a Jordanian population: Int Endod J, 2009; 42; 775-84
27. Barbizam JVB, Ribeiro RG, Tanomaru Filho M, Unusual anatomy of permanent maxillary molars: J Endod, 2004; 30; 668-71
28. Special Committee to Revise the Joint AAE/AAOMR Position Statement on use of CBCT in Endodontics, AAE and AAOMR joint position statement: use of cone beam computed tomography in endodontics 2015 update: Oral Surg Oral Med Oral Pathol Oral Radiol, 2015; 120; 508-12
29. Panel SGD: Cone Beam CT for Dental and Maxillofacial Radiology (Evidence Based Guidelines), 2012, European Commission: Directorate-General for Energy
30. Zhang R, Yang H, Yu X, Use of CBCT to identify the morphology of maxillary permanent molar teeth in a Chinese subpopulation: Int Endod J, 2011; 44; 162-69
31. Han X, Yang H, Li G, A study of the distobuccal root canal orifice of the maxillary second molars in Chinese individuals evaluated by cone-beam computed tomography: J Appl Oral Sci, 2012; 20; 563-67
32. Khademi A, Zamani Naser A, Bahreinian Z, Root morphology and canal configuration of first and second maxillary molars in a selected Iranian population: A cone-beam computed tomography evaluation: Iran Endod J, 2017; 12; 288-92
33. Ratanajirasut R, Panichuttra A, Panmekiate S, A cone-beam computed tomographic study of root and canal morphology of maxillary first and second permanent molars in a Thai population: J Endod, 2018; 44; 56-61
34. Nikoloudaki GE, Kontogiannis TG, Kerezoudis NP, Evaluation of the root and canal morphology of maxillary permanent molars and the incidence of the second mesiobuccal root canal in Greek population using cone-beam computed tomography: Open Dent J, 2015; 9; 267-72
35. Martins JNR, Gu Y, Marques D, Differences on the root and root canal morphologies between Asian and white ethnic groups analyzed by cone-beam computed tomography: J Endod, 2018; 44; 1096-104
36. Kim Y, Lee SJ, Woo J, Morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a Korean population: Variations in the number of roots and canals and the incidence of fusion: J Endod, 2012; 38; 1063-68
37. Silva EJNL, Nejaim Y, Silva AIV: J Endod, 2014; 40; 173-76
38. Al-Fouzan KS, Ounis HF, Merdad K, Al-Hezaimi K, Incidence of canal systems in the mesio-buccal roots of maxillary first and second molars in Saudi Arabian population: Aust Endod J, 2013; 39; 98-101
39. Reis AG, de AR, Grazziotin-Soares R, Barletta FB, Second canal in mesiobuccal root of maxillary molars is correlated with root third and patient age: A cone-beam computed tomographic study: J Endod, 2013; 39; 588-92
40. Degerness RA, Bowles WR, Dimension, anatomy and morphology of the mesiobuccal root canal system in maxillary molars: J Endod, 2010; 36; 985-89
41. Gao Y, An SF, Ling JQAn study on the incidence of the second mesiobuccal canal in the mesiobuccal root of the first and second maxillary molars: Zhonghua Kou Qiang Yi Xue Za Zhi, 2006; 41; 521-24 [in Chinese]
42. Stropko JJ, Canal morphology of maxillary molars: Clinical observations of canal configurations: J Endod, 1999; 25; 446-50
43. Eskoz N, Weine FS, Canal configuration of the mesiobuccal root of the maxillary second molar: J Endod, 1995; 21; 38-42
44. Gilles J, Reader A, An SEM investigation of the mesiolingual canal in human maxillary first and second molars: Oral Surg Oral Med Oral Pathol, 1990; 70; 638-43
45. Naseri M, Ali Mozayeni M, Safi Y, Root canal morphology of maxillary second molars according to age and gender in a selected Iranian population: A cone-beam computed tomography evaluation: Iran Endod J, 2018; 13; 373-80
46. Su CC, Huang RY, Wu YC, Detection and location of second mesiobuccal canal in permanent maxillary teeth: A cone-beam computed tomography analysis in a Taiwanese population: Arch Oral Biol, 2019; 98; 108-14
47. Zhang Q, Chen H, Fan B, Root and root canal morphology in maxillary second molar with fused root from a native Chinese population: J Endod, 2014; 40; 871-75
48. Rouhani A, Bagherpour A, Akbari M, Cone-beam computed tomography evaluation of maxillary first and second molars in Iranian population: A morphological study: Iran Endod J, 2014; 9; 190-94
49. Kim S, Kratchman S, Modern endodontic surgery concepts and practice: A review: J Endod, 2006; 32; 601-23
50. Lavasani SA, Tyler C, Roach SH, Cone-beam computed tomography: Anatomic analysis of maxillary posterior teeth-impact on endodontic microsurgery: J Endod, 2016; 42; 890-95
Figures
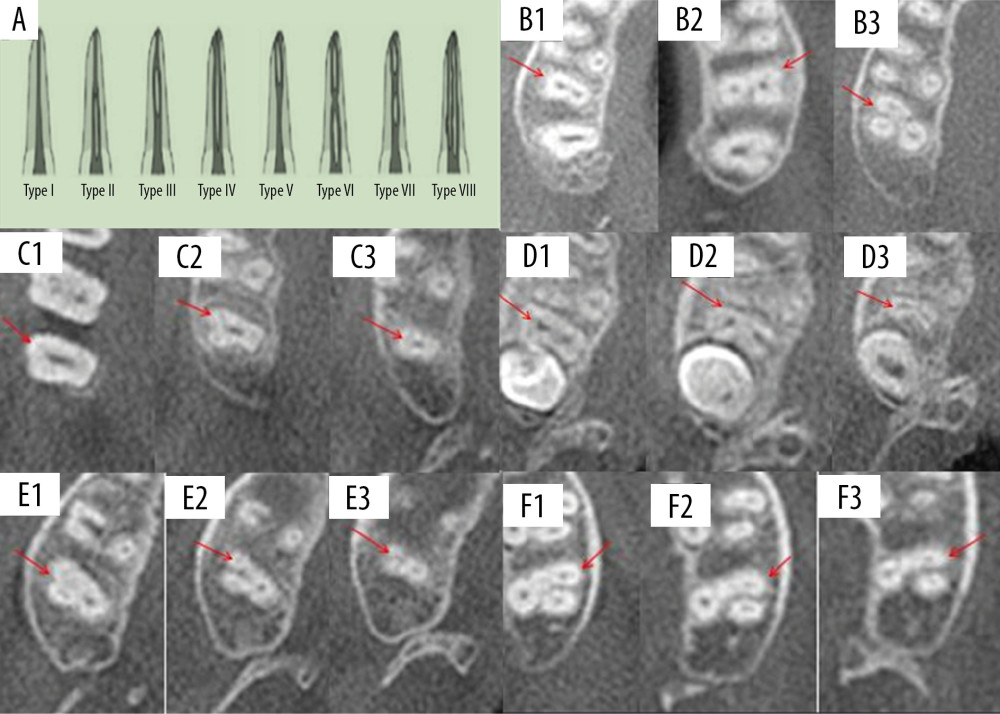 Figure 1. Schematic diagrams showing Vertucci’s classification of root canal morphology and canal configuration of permanent second molars of the upper jaw with fused roots. (A) Classification of the anatomic morphology of canals. (B) Teeth with one (B1), two (B2), and three (B3) roots. (C) Fused root with one root canal (C1, coronal 1/3; C2, middle 1/3; and C3, apical 1/3). (D) Fused root with two root canals (D1, coronal 1/3; D2, middle 1/3; D3, apical 1/3). (E) Fused root with three root canals (E1, coronal 1/3; E2, middle 1/3; E3, apical 1/3). (F) Fused root with four root canals (F1, coronal 1/3; F2, middle 1/3; F3, apical 1/3).
Figure 1. Schematic diagrams showing Vertucci’s classification of root canal morphology and canal configuration of permanent second molars of the upper jaw with fused roots. (A) Classification of the anatomic morphology of canals. (B) Teeth with one (B1), two (B2), and three (B3) roots. (C) Fused root with one root canal (C1, coronal 1/3; C2, middle 1/3; and C3, apical 1/3). (D) Fused root with two root canals (D1, coronal 1/3; D2, middle 1/3; D3, apical 1/3). (E) Fused root with three root canals (E1, coronal 1/3; E2, middle 1/3; E3, apical 1/3). (F) Fused root with four root canals (F1, coronal 1/3; F2, middle 1/3; F3, apical 1/3).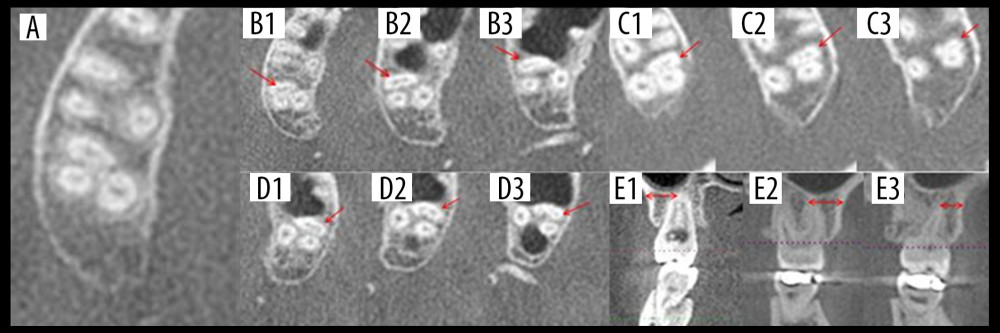 Figure 2. Types of canal configuration in mesiobuccal roots of permanent second molars of the upper jaw and horizontal distances from the buccal root apices to the surface of buccal cortical bone plate. (A) Type I. (B) Type II (B1, coronal 1/3; B2, middle 1/3; B3, apical 1/3). (C) Type III (C1, coronal 1/3; C2, middle 1/3; C3, apical 1/3). (D) Type IV (D1, coronal 1/3; D2, middle 1/3; D3, apical 1/3). (E) Horizontal distances from single buccal root (E1), mesiobuccal root (E2), and distobuccal root (E3) apices to the surface of the buccal cortical bone plate.
Figure 2. Types of canal configuration in mesiobuccal roots of permanent second molars of the upper jaw and horizontal distances from the buccal root apices to the surface of buccal cortical bone plate. (A) Type I. (B) Type II (B1, coronal 1/3; B2, middle 1/3; B3, apical 1/3). (C) Type III (C1, coronal 1/3; C2, middle 1/3; C3, apical 1/3). (D) Type IV (D1, coronal 1/3; D2, middle 1/3; D3, apical 1/3). (E) Horizontal distances from single buccal root (E1), mesiobuccal root (E2), and distobuccal root (E3) apices to the surface of the buccal cortical bone plate. Tables
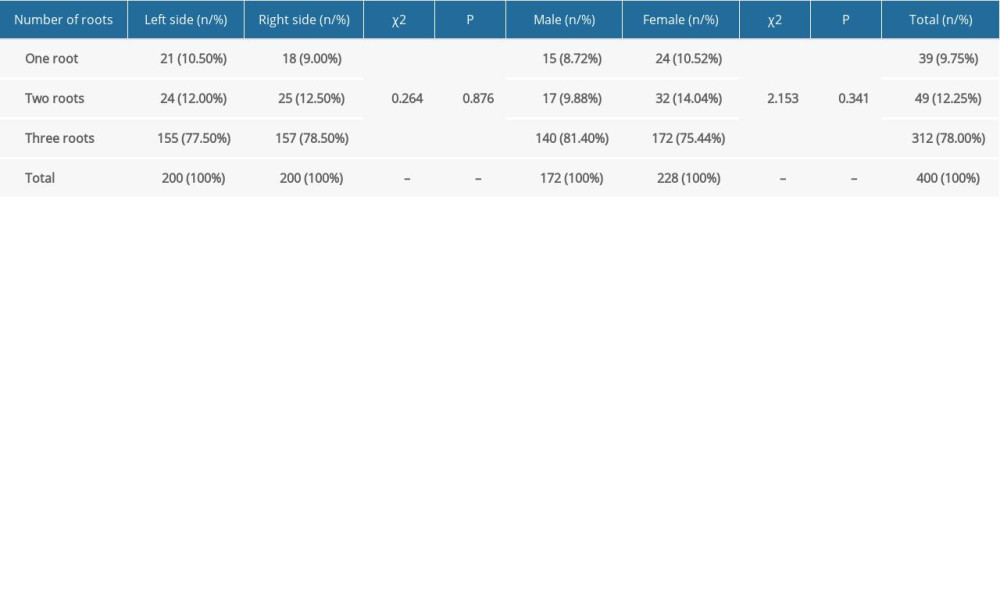 Table 1. Numbers of roots.
Table 1. Numbers of roots.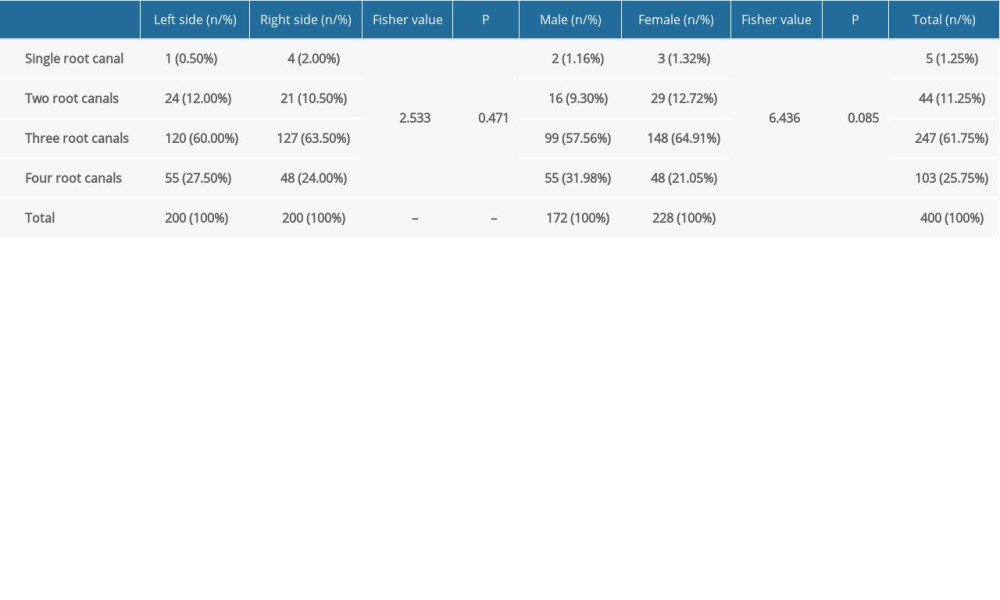 Table 2. Numbers of root canals.
Table 2. Numbers of root canals.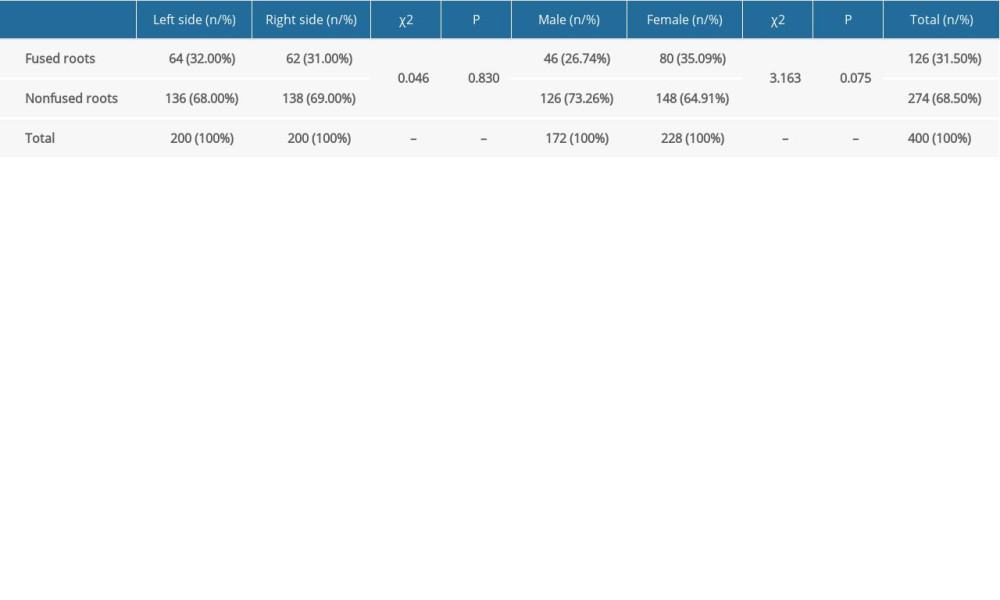 Table 3. Rates of root fusion.
Table 3. Rates of root fusion.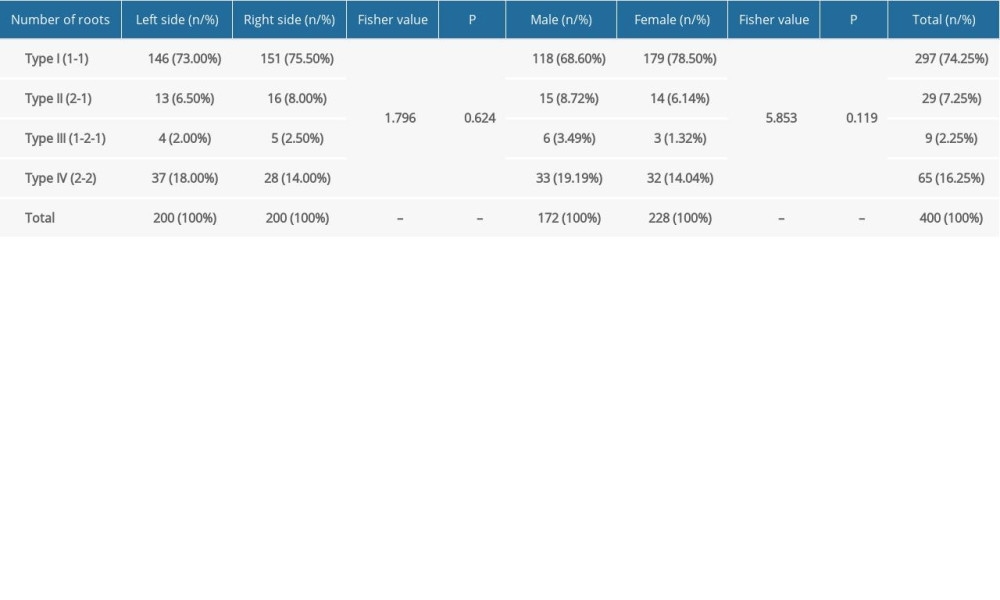 Table 4. Root canal configurations of mesiobuccal roots.
Table 4. Root canal configurations of mesiobuccal roots.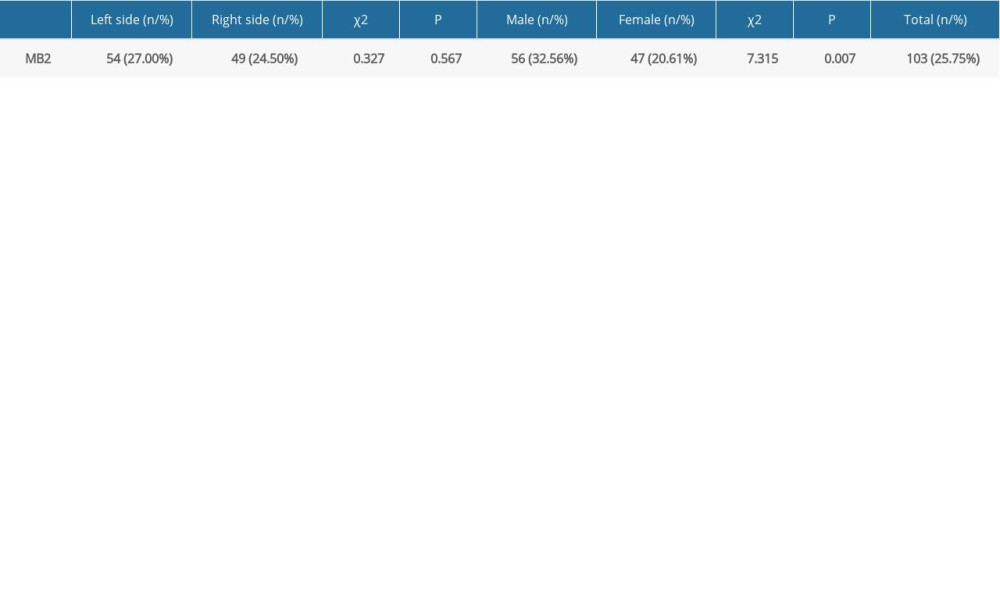 Table 5. Prevalence of MB2 canals
Table 5. Prevalence of MB2 canals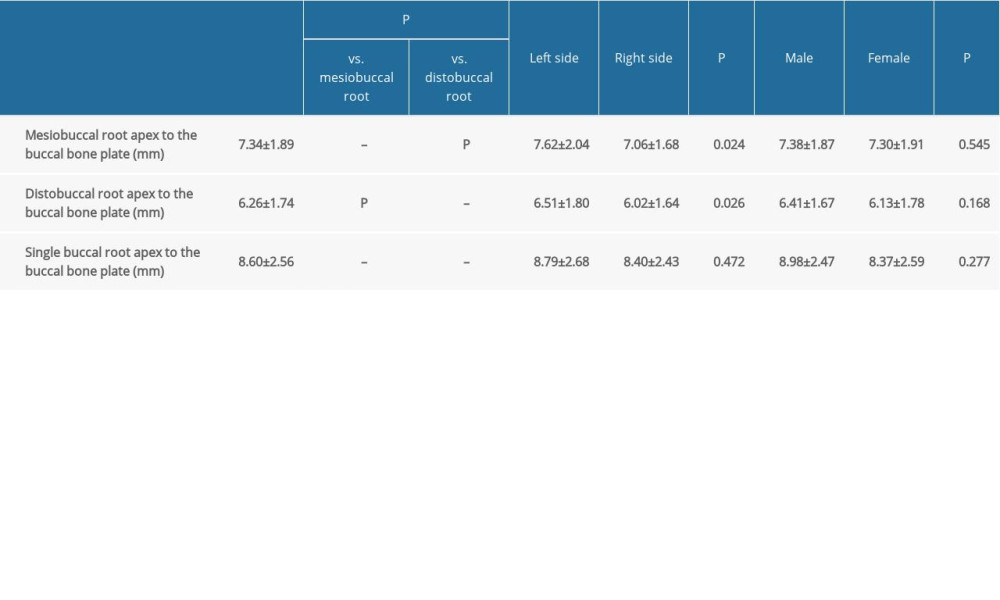 Table 6. Distances from the buccal root apices to the surface of the buccal cortical bone plate.
Table 6. Distances from the buccal root apices to the surface of the buccal cortical bone plate. Table 7. Numbers of roots in maxillary permanent second molars reported in previous studies.
Table 7. Numbers of roots in maxillary permanent second molars reported in previous studies.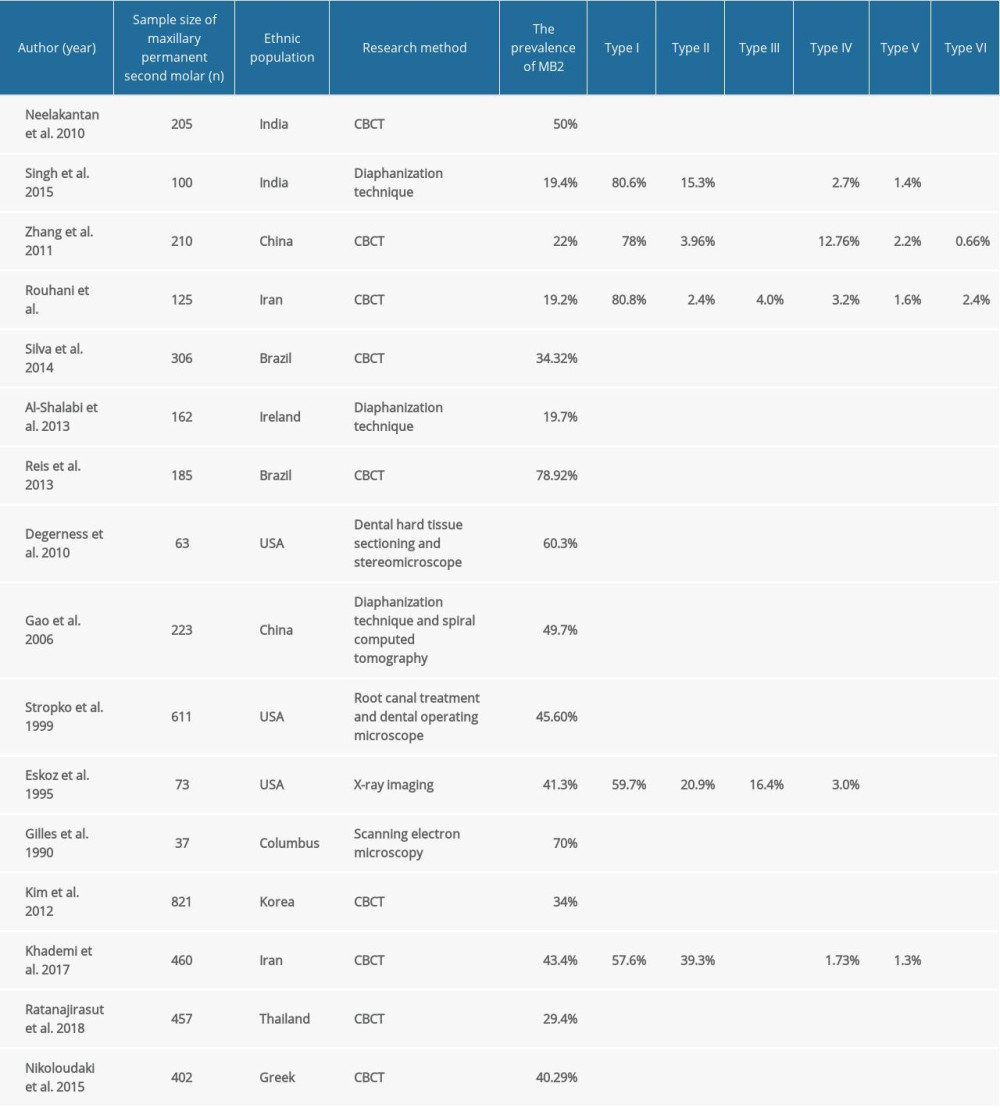 Table 8. Rates of MB2 and root canal configurations of the mesiobuccal roots of the maxillary permanent second molars reported in previous studies.
Table 8. Rates of MB2 and root canal configurations of the mesiobuccal roots of the maxillary permanent second molars reported in previous studies.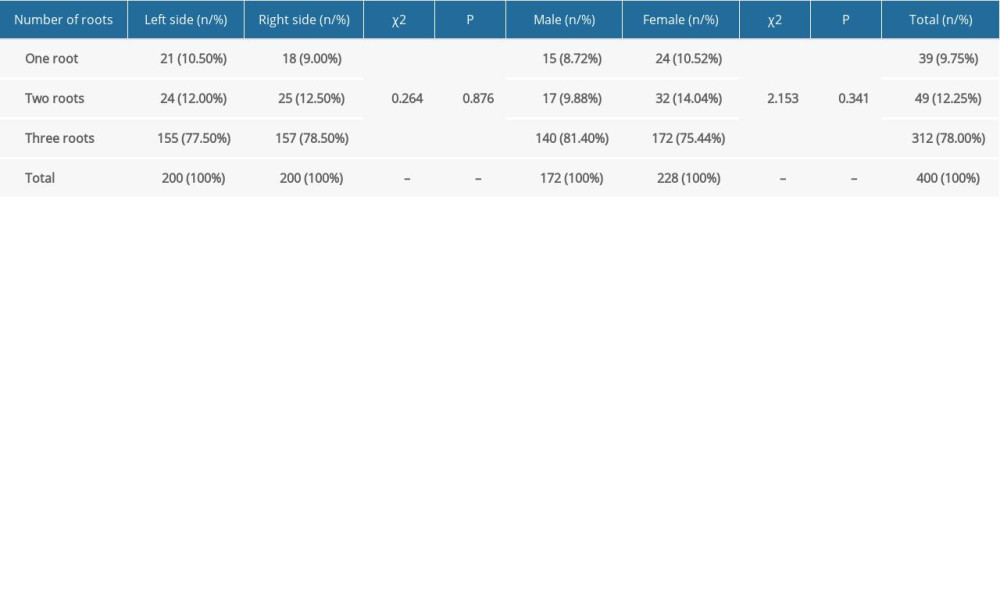 Table 1. Numbers of roots.
Table 1. Numbers of roots.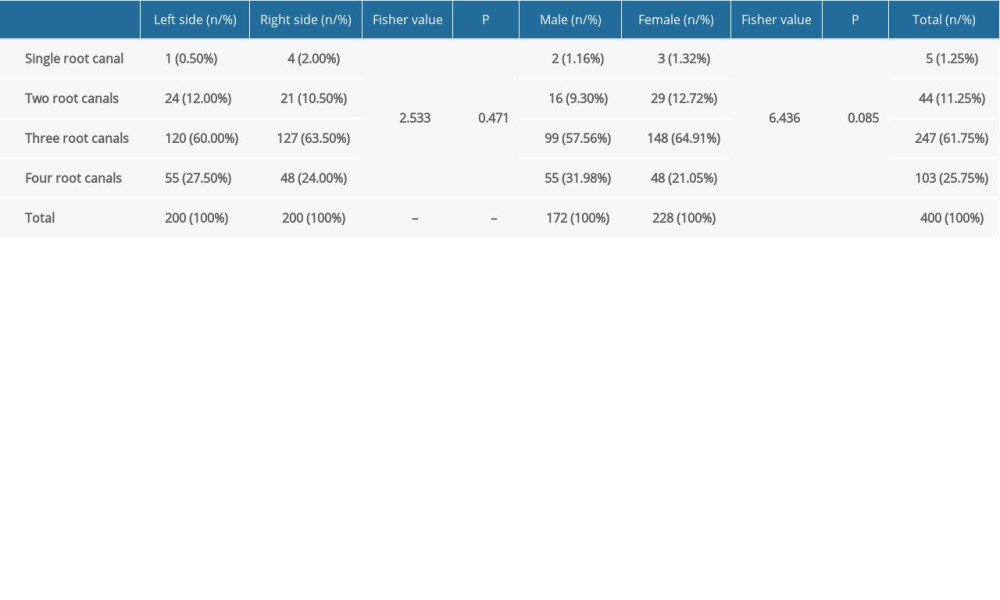 Table 2. Numbers of root canals.
Table 2. Numbers of root canals.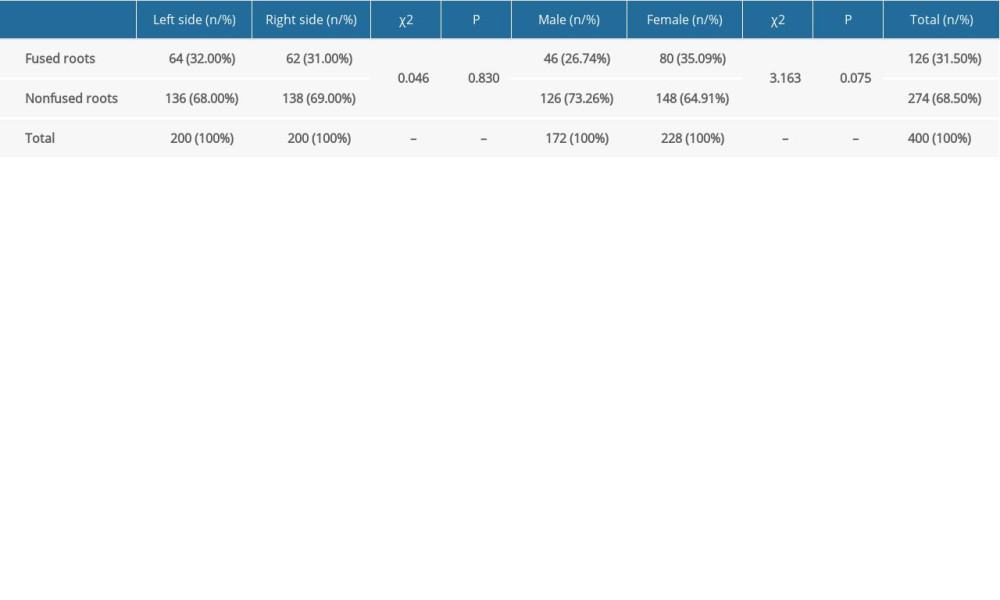 Table 3. Rates of root fusion.
Table 3. Rates of root fusion.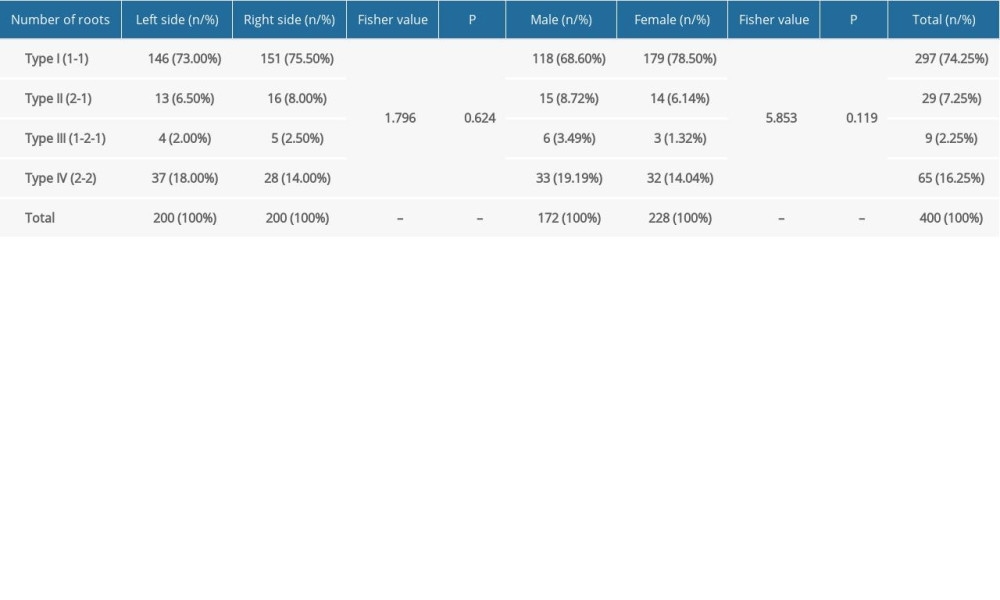 Table 4. Root canal configurations of mesiobuccal roots.
Table 4. Root canal configurations of mesiobuccal roots.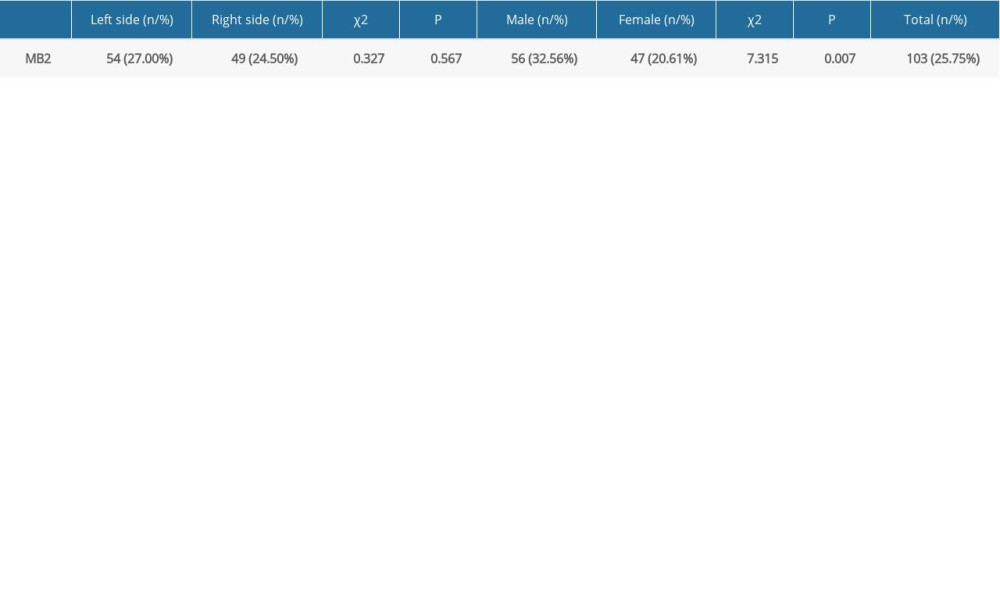 Table 5. Prevalence of MB2 canals
Table 5. Prevalence of MB2 canals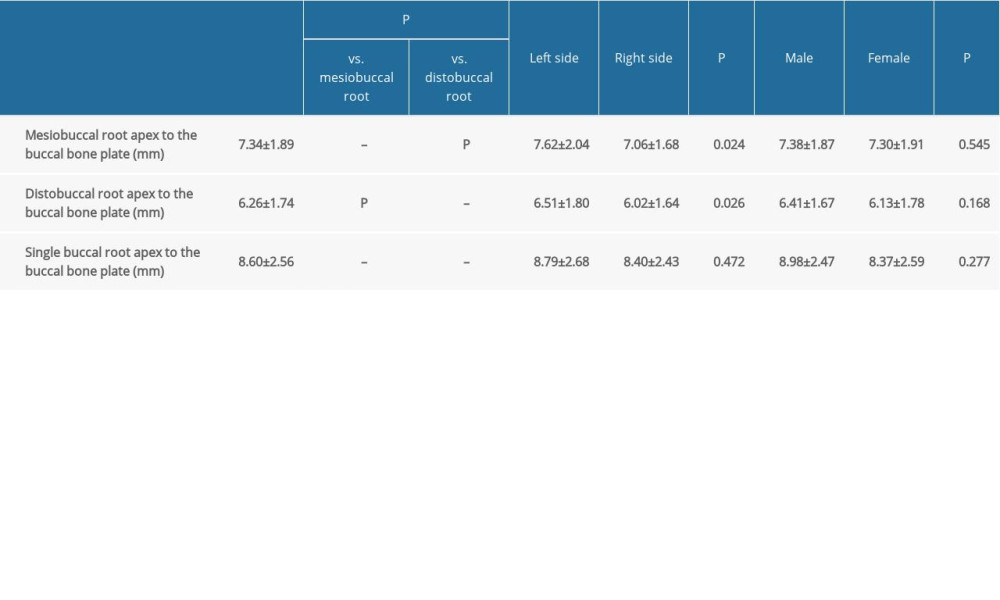 Table 6. Distances from the buccal root apices to the surface of the buccal cortical bone plate.
Table 6. Distances from the buccal root apices to the surface of the buccal cortical bone plate. Table 7. Numbers of roots in maxillary permanent second molars reported in previous studies.
Table 7. Numbers of roots in maxillary permanent second molars reported in previous studies.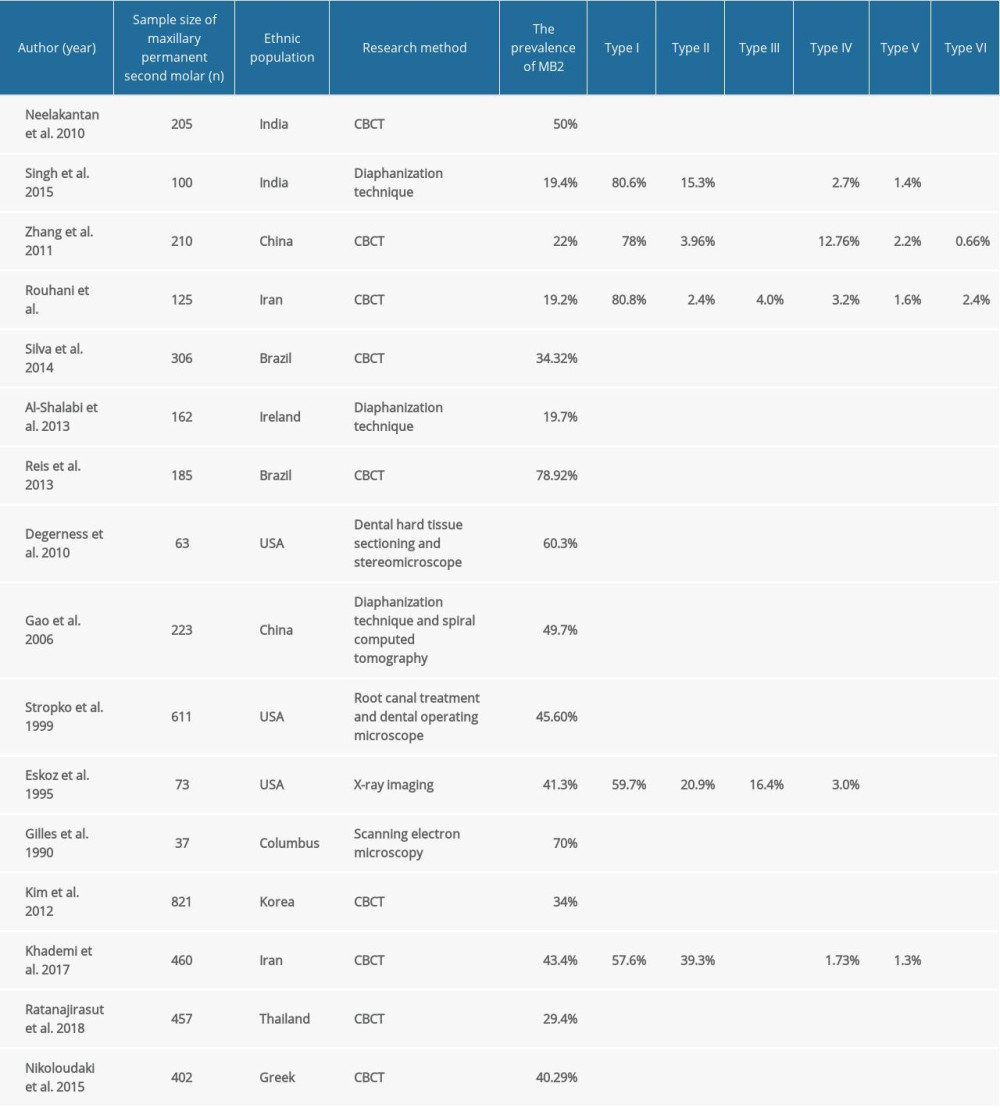 Table 8. Rates of MB2 and root canal configurations of the mesiobuccal roots of the maxillary permanent second molars reported in previous studies.
Table 8. Rates of MB2 and root canal configurations of the mesiobuccal roots of the maxillary permanent second molars reported in previous studies. In Press
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








