17 August 2020: Clinical Research
Evaluation of Ovarian Tumors with Multidetector Computed Tomography and Tumor Markers: Differentiation of Stage I Serous Borderline Tumors and Stage I Serous Malignant Tumors Presenting as Solid-Cystic Mass
Xin-Ping Yu1BCE, Ying Liu2C, Jin-Wen Jiao1D, Hong-Juan Yang1B, Rui-Jing Wang1D, Shuai Zhang3ACF*DOI: 10.12659/MSM.924497
Med Sci Monit 2020; 26:e924497
Abstract
BACKGROUND: The aim of this study was to determine multidetector computed tomography (MDCT) features and tumor markers for differentiating stage I serous borderline ovarian tumors (SBOTs) from stage I serous malignant ovarian tumors (SMOTs).
MATERIAL AND METHODS: In total, 48 patients with stage I SBOTs and 54 patients with stage I SMOTs who underwent MDCT and tumor markers analysis were analyzed. MDCT features included location, shape, margins, texture, papillary projections, vascular abnormalities, size, and attenuation value. Tumor markers included serum cancer antigen 125 (CA125), carbohydrate antigen 19-9 (CA19-9), carcinoembryonic antigen (CEA), and human epididymis protein 4 (HE4). Parameters of clinical characteristic, MDCT features, and tumor markers were compared using a chi-square test and Mann-Whitney U tests. A binary logistic regression analysis was performed to detect predictors for SMOTs. A receiver operating characteristic (ROC) curve analysis was used to assess the potential diagnostic value of the quantitative parameters. Kappa and intraclass correlation coefficients were used to evaluate interobserver reproducibility for MDCT features.
RESULTS: Median ages between patients with SBOTs and SMOTs were significantly different. Compared with SBOTs, vascular abnormalities were significantly more common in SMOTs. CA125, HE4, the maximum thickness of the wall, the maximum thickness of the septa, and the maximum diameter of the solid portions were significantly higher in patients with SMOTs. A binary logistic regression analysis revealed that age, vascular abnormalities, and the maximum diameter of the solid portion were independent factors of SMOTs. ROC analysis was used to assess the potential diagnostic value for predicting SMOTs. Moderate or good interobserver reproducibility for MDCT features were identified.
CONCLUSIONS: Age, vascular abnormalities, and the maximum diameter of the solid portion were independent factors for differentiating SBOTs from SMOTs. The combined analysis of age, vascular abnormalities, and the maximum diameter of the solid portion may allow better differentiation between SBOTs and SMOTs.
Keywords: multidetector computed tomography, Ovarian Neoplasms, Tumor Markers, Biological, ROC Curve
Background
Ovarian cancer is a common disease in women worldwide, and epithelial ovarian tumors that result from ovarian cancer account for 60% of all ovarian tumors [1,2]. Depending on histologic grade of differentiation and biologic behavior, epithelial ovarian tumors are categorized as benign, borderline, and malignant. Depending on the different histological sources, epithelial ovarian tumors can be further divided into serous tumors, mucinous tumors, endometrioid tumors, clear cell tumors, and Brenner tumors, with the serous type being the most common[3,4].
Benign epithelial tumors are mainly cystic, while borderline or malignant tumors often present as a solid-cystic mass or solid mass. When presenting as a solid-cystic mass, it is vital to preoperatively distinguish borderline and malignant tumors. This is because stage I borderline tumors are usually treated by conservative fertility-sparing laparoscopic surgery in patients who desire fertility preservation, and require long-term follow-up [5,6]. Meanwhile, malignant ovarian tumors always require a comprehensive staging surgery and require postoperative chemotherapy [1].
Multidetector computed tomography (MDCT) has been widely used in the diagnosis and follow-up of ovarian tumors in recent years, and it can provide clinically relevant information for various ovarian lesions and stage ovarian cancer, as well as evaluate surgical resectability [7–9]. However, when medical imaging methods were used to distinguish borderline and malignant tumors, previous studies focused on the shape of the tumor itself [10–12] or the tumor vascular changes [13], ignoring the combination of tumor morphology with tumor vascular changes.
Biomarkers, such as serum cancer antigen 125 (CA125), carbohydrate antigen 19-9 (CA19-9), carcinoembryonic antigen (CEA), and human epididymis protein 4 (HE4), all have potential value in early-stage ovarian cancer detection. CA125 is the most commonly used tumor biomarker for the diagnosis of ovarian tumors [14]. HE4 has advantages in monitoring the progression of ovarian cancer over CA125 [15–17]. Though usually used in the digestive tract tumors, CA19-9 and CEA are also elevated in ovarian cancer [18]. Currently, some studies tend to value only the differences between CA125 values for borderline and malignant tumors, and ignore the comprehensive analysis of different tumor biomarkers, especially when combined with imaging features [19,20]. In addition, in a recent study on differentiating ovarian metastases in colorectal cancer from primary ovarian cancer, the method of combining morphology and tumor markers has been reported to be useful [21]. Based on this background, the aim of our study was to retrospectively analyze the diagnostic ability of MDCT, emphasizing the tumor vascular changes and combining these with various tumor markers, in order to differentiate stage I serous borderline ovarian tumors (SBOTs) from stage I serous malignant ovarian tumors (SMOTs).
Material and Methods
STUDY POPULATION:
The Institutional Research Board of our hospital approved this study. Informed consent was obtained from all patients and patients were informed of the possibility of a reaction to the MDCT contrast agent. Clinical and imaging data from consecutive patients ultimately all diagnosed with SBOTs and SMOTs between December 2017 and December 2019 were collected. We initially collected data from 161 patients with SBOTs and 267 patients with SMOTs. The inclusion criteria of this study were as follows: first, the diagnosis of stage I SBOTs or SMOTs was based on the surgical pathology according to International Federation of Gynecology and Obstetrics (FIGO) [22] and the 2014 World Health Organization (WHO) classification of tumors of female reproductive organs [23]; second, the imaging demonstrated a solid-cystic tumor. The exclusion criteria were as follows: first, patients that had other diseases that could influence tumor marker levels, such as celiac or pelvic inflammation, were excluded; second, patients whose clinical data were incomplete, such as absence of MDCT imaging or tumor markers, were excluded; third, those whose surgical pathology confirmed stage II–IV ovarian tumors were also excluded. Finally, we collected data from 48 patients (47.1%) with SBOTs and 54 patients (52.9%) with SMOTs. Clinical symptoms of the patients included abdominal distension, abdominal pain, increased abdominal size, accidentally-discovered adnexal masses in a health examination, and abnormal vaginal bleeding.
MULTIDETECTOR COMPUTED TOMOGRAPHY (MDCT) PROTOCOLS:
Contrast-enhanced pelvic CT scans were performed using 5 different CT scanners: Aquilion ONE (Canon medical systems), Discovery CT750 HD (GE medical systems), Optima CT670 (GE medical systems), iCT 256 (PHILIPS), SOMATOM Definition Flash (SIEMENS). All examinations were performed after intravenous contrast (80–100 mL iohexol, 300 mg iodine/mL; Beijing Beilu Pharmaceutical, Beijing, China). The contrast agent was injected at the rate of 2.0–3.0 mL/s by using an automatic power injector. Patients were scanned on MDCT scanners with the following parameters: 100 mAs; 120 kV; rotation time of 0.6 s; tube current of 600 mA; helical pitch of 0.984; thickness of 1–1.2 mm. Each patient underwent 3-phase contrast-enhanced CT examinations of the pelvic cavity. Arterial phase was performed a delay time of 13–17 s after abdominal aorta attenuation reached 100 Hounsfield unit (Hu) using the tracking technique. Portal phase was performed 30 s after the arterial phase. Equilibrium phase scanning was performed 180 s after the portal phase. The reformats in volume rendering and three dimensionally reconstructed images were acquired in all patients. All patients underwent surgery within 1 week after the MDCT scan.
IMAGE ANALYSIS:
Two board-certified radiologists with 7 and 9 years of experience in gynecologic radiology separately and independently viewed the imaging and recorded the following qualitative data: a) location, unilateral or bilateral; b) tumor shape, lobulated or round/oval; c) margins, smooth or irregular; d) texture, predominantly cystic or predominantly solid; e) papillary projections, absent or present; f) papillary projections with papillary surface, absent or present; g) discontinuous septa, absent or present; h) ascites, absent or present; and i) vascular abnormalities, absent or present. In patients with bilateral ovarian lesions, the MDCT feature was considered positive if at least one ovarian lesion was observed. Papillary projections were defined as solid structure into the cystic space growing from the cyst wall or septum. Discontinuous septa were defined as existing 2 or more interrupts of septa on cross-sectional image of the same level. Location, tumor shape, margins, texture, and ascites were evaluated on axial image. Vascular abnormalities were defined as existence at least one of the following conditions: a)serpentine and, or chaotic course of vessels, manifesting distortion of the feeding artery with blurred boundaries of its branches; b)presence of microaneurysms; c) presence of arterio-venous fistula [13]. Vascular abnormalities that exist in septa, papillary projection, or solid parts of the tumor are all considered positive with or without abnormal blood vessels outside the tumor. Vascular abnormalities are evaluated on axial image with reference to maximal intensity projection (MIP) algorithm and volume rendering (VR) algorithm. Any discrepancies between the interpretations were resolved by discussion to obtain a consensus decision.
The quantitative data included tumor markers (CA125, CA19-9, CEA, and HE4), size (maximum thickness of wall, septa, and solid component) and attenuation value. If the largest solid part was a papillary projection, it was considered as both a papillary projection and solid portion of the mass. We selected the largest slice of the solid portion to measure the lesion attenuation value. Two measurements were obtained, and mean attenuation values were recorded. For both the qualitative and quantitative data, in cases of bilateral ovarian masses, if SBOTs and SMOTs were in the same case, the SMOT lesions were analyzed. If the bilateral ovarian masses had the same pathology results, the lesion with the features that tend indicated malignancy (a more solid texture) was analyzed.
STATISTICAL ANALYSIS:
Statistical analyses were performed using SPSS software (version 23.0, SPSS, Inc., Chicago, IL, USA) for Windows. Qualitative variables were recorded as frequencies and percentages. Quantitative variables were presented as medians. The chi-squared test or Fisher’s exact test was used to evaluate whether the qualitative variables were significantly different between SBOTs and SMOTs. Mann-Whitney U tests were used to compare the differences between SBOTs or SMOTs in terms of the quantitative variables. A binary logistic regression analysis was used to detect significant independent predictors of SMOTs in terms of qualitative and quantitative variables that had significant differences, according to a univariate analysis. A receiver operating characteristic (ROC) analysis was used to assess the relative potential diagnostic value in predicting SMOTs. Interobserver reproducibility for MDCT features was evaluated using the kappa statistic (κ) for the qualitative variables and the intra-class correlation coefficient (ICC) for the quantitative variables.
Results
CLINICAL DATA OF SBOTS AND SMOTS:
The clinical data are shown in Table 1. The median ages between patients with SBOTs and SMOTs were significantly different (42 versus 52 years, P<0.001). Patients with SMOTs had higher proportion of menopause compared with patients with SBOTs (51.9% versus 18.8%, P=0.001).
COMPARISON OF QUALITATIVE DATA BETWEEN SBOTS AND SMOTS:
The qualitative MDCT features of the patients with SBOTs and SMOTs are shown in Table 2. Vascular abnormalities (16.7% versus 66.7%, P<0.001) were significantly more common in patients with SMOTs, compared to patients with SBOTs (Figures 1–3).
COMPARISON OF QUANTITATIVE DATA BETWEEN SBOTS AND SMOTS:
The quantitative data of patients with SBOTs and SMOTs are shown in Table 3. The levels of CA125 (130.3 versus 328.8 U/mL, P=0.005), HE4 (74.6 versus 123.3 pmol/L, P<0.001), the maximum thickness of the wall (2.6 versus 3.45 mm, P=0.001), the maximum thickness of the septa (2.6 versus 3.5 mm, P=0.002), and the maximum diameter of the solid portion (31.5 versus 43.5 mm, P<0.001) in the SMOT patients were higher than that in the SBOT patients.
BINARY LOGISTIC REGRESSION ANALYSIS BETWEEN SBOTS AND SMOTS:
Univariate and multivariate logistic regression analyses predicting SMOTs are shown in Table 4. In the univariate regression analysis, age (OR 1.098, P<0.001), the level of CA125 (OR 1.002, P=0.007), the level of HE4 (OR 1.015, P=0.001), vascular abnormalities (OR 10.000, P<0.001), maximum thickness of the wall (OR 2.339, P=0.001), maximum thickness of the septa (OR 1.979, P=0.005), and maximum diameter of the solid portion (OR 1.104, P<0.001) were identified as significant predictors for diagnosing SMOTs. In the multivariate logistic regression analysis, age (OR 1.089, P=0.014) vascular abnormalities (OR 11.12, P=0.001), and the maximum diameter of the solid portion (OR 1.069, P=0.045) were identified as significant predictors for diagnosing SMOTs. The area under the ROC curves, sensitivities, specificities, and threshold values are shown in Table 5, and the combination of age, vascular abnormalities, and the maximum diameter of the solid portion had a high sensitivity (88.9%) and specificity (85.4%) and the highest AUC (0.939) (Figure 4).
INTEROBSERVER AGREEMENT OF MDCT FEATURES:
The interobserver agreement between the 2 radiologists was moderate or good for MDCT features of SBOTs and SMOTs (κ range: 0.697–1.000; ICC range: 0.749–0.854) (Table 6).
Discussion
SBOTs and SMOTs are common in women. They are 2 different entities with different grades of cell differentiation, different prognoses, and different operation methods. However, differentiating SBOTs from SMOTs using imaging is often difficult. To the best of our knowledge, no published studies have compared SBOTs and SMOTs using a comprehensive analysis of their clinical characteristics, tumor markers, and CT features. Thus, we carried out a comprehensive analysis of these factors, and focused on identifying independent factors for differentiating SBOTs from SMOTs. We also wanted to see whether their diagnostic abilities improved after combining the aforementioned factors, in order to improve differential diagnosis and to allow treatments to be carried out in a more timely and effective manner.
In our research, the median age of SMOTs diagnosis was 10 years older than for SBOTs, which was in agreement with previous studies [24]. Additionally, 51.9% of SMOT patients were menopausal, compared to 18.8% of SBOT patients, which was an anticipated finding due to the age difference between the 2 groups. Published papers have suggested that SBOT patients are more likely to be asymptomatic compared to SMOT patients [5]. In our study, 33.3% of patients with SBOTs were asymptomatic, with an accidentally-discovered adnexal mass after a health examination, which was not as common in patients with SMOTs. SBOT patients are more likely to have a longer duration before diagnosis compared to SMOT patients [25], which is likely because SBOTs behave benignly at first. However, in our study, there was no significant difference in duration between SBOT and SMOT diagnosis. We speculated that with the development of a better economy and society, people’s health consciousness has been improved; therefore, if symptoms are found, medical attention will be promptly provided. Although there were differences in the symptoms between the 2 groups in our study, symptoms alone might not be sufficient to accurately distinguish SBOTs from SMOTs due to symptom overlaps.
MDCT is currently considered the best imaging technique for staging ovarian tumor and is used to predict their relative resectability [9]. Therefore, we used MDCT as a tool to distinguish SBOTs from SMOTs in this study. Several researchers have attempted to find useful imaging features and criteria to discriminate SBOTs and SMOTs, testing various imaging modalities [26–28]. In our study, location, tumor shape, margins, texture, and papillary projections were not significantly different between the 2 groups. A previous study [11] showed that SMOTs tend to manifest with irregular margins, which was inconsistent with our findings. We speculated that the included patients in our study who were stage I, had not yet manifested aggressive features in their imaging. However, our results demonstrated that vascular abnormalities were more frequent in SMOTs than in SBOTs, which was concordant with another previous study [13]. The mechanism might be that the growth of the malignant tumor is dependent on the neovascularization, and angiogenesis is the path through which tumors transition from benign to malignant. Therefore, the malignant tumors have a high blood vessel density, manifesting as serpentine and chaotic courses of vessels in medical imaging. Additionally, the blood vessels of malignant tumors are immature, and the capillary wall of a malignant tumor is composed of a single layer of endothelial cells, and the outer membrane lacks an inelastic basement. In cases where there is increased blood flow and increased pressure, the wall of the vessels is vulnerable to rupture, causing microaneurysms and arterio-venous fistulas.
In our study, SMOTs and SBOTs enhanced papillary projections and solid components, which is in accordance with previous literature [29]. However, the attenuation values of arterial, venous, and equilibrium phases were not significantly different between SBOT and SMOT patients. Therefore, the attenuation values in enhanced CT images did not appear to be important in distinguishing the 2 groups. However, enhanced CT imaging is still necessary due to its ability to demonstrate vascular abnormalities, and should be considered for the differentiation of other adnexal space-occupying lesions. The maximum thickness of the wall, the maximum thickness of the septa, and the maximum diameter of the solid portion in patients with SMOTs were larger than in the SBOT patients. This was in agreement with our expectations, and previous studies [11].
However, due to the overlapping features of SMOTs and SBOTs, a definitive diagnosis should not be made based on imaging alone or single tumor biomarkers. Several studies depending on imaging combined with tumor markers and multi-biomarker methods have been applied to increase the sensitivity and specificity of diagnosing early-stage ovarian cancer [14,19,30]. Guo et al. [18] reported that the combination of CA125, CA19-9, and CEA markers was a promising method for detecting epithelial ovarian cancer. HE4, as a novel biomarker, is also a useful preoperative test for differentiating between benign and malignant ovarian tumors [15–17]. The risk of ovarian malignancy algorithm (ROMA), a well-known risk model, combines the results of CA125, HE4, and menopausal status to provide a quantitative assessment of the probability of ovarian cancer [31]. Our results showed that the levels of CA125 and HE4 were significantly increased in the SMOTs.
In the multivariate logistic regression analysis, our study showed that age, vascular abnormalities, and the maximum diameter of the solid portion were identified as significant predictors for diagnosing SMOTs. When combining age, vascular abnormalities, and the maximum diameter of the solid portion, the AUC, sensitivity, and specificity were 0.939, 88.9%, and 85.4% respectively. Therefore, our study showed that in order to differentiate SBOTs from SMOTs, age, vascular abnormalities, and the solid portions should be analyzed comprehensively. By combining age, vascular abnormalities, and solid portions, radiologists can create better treatment recommendations for gynecologists.
Our study had several limitations. First, there are other similar kinds of solid and cystic ovarian tumors to differentiate from, such as mucinous cystic tumors, endometrial cancers, and metastatic tumors. Therefore, the exclusion of these other tumors needs to be studied in the future. Second, this was a retrospective study, and images of patients were derived from different CT scanners, which may have resulted in minor differences in the measurements. Third, in the multivariate analysis of our study, many variables were analyzed compared to the number of samples, which may cause a bias.
Conclusions
Age, vascular abnormalities, and the maximum diameter of the solid portion were independent factors for differentiating SBOTs from SMOTs. The combined analysis of age, vascular abnormalities, and the maximum diameter of the solid portion may allow for better differentiation between SBOTs and SMOTs.
Figures
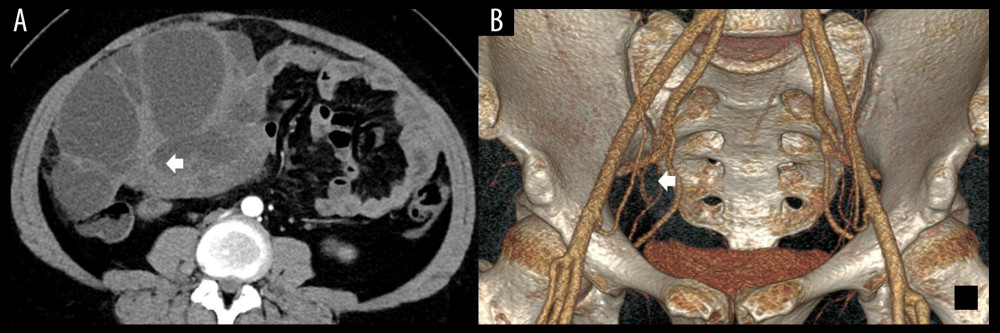 Figure 1. (A) The enhanced axial multidetector computed tomography images of a 32-year-old female with SBOTs showed a solid-cystic mass with thick wall and thick septa (arrow); however, with few vascular abnormalities in the endophytic part of the tumor. (B) The reformat in VR algorithm. Scant tiny vessels in the endophytic part of the tumor (arrow). SBOTs – serous borderline ovarian tumors; VR – volume rendering.
Figure 1. (A) The enhanced axial multidetector computed tomography images of a 32-year-old female with SBOTs showed a solid-cystic mass with thick wall and thick septa (arrow); however, with few vascular abnormalities in the endophytic part of the tumor. (B) The reformat in VR algorithm. Scant tiny vessels in the endophytic part of the tumor (arrow). SBOTs – serous borderline ovarian tumors; VR – volume rendering. 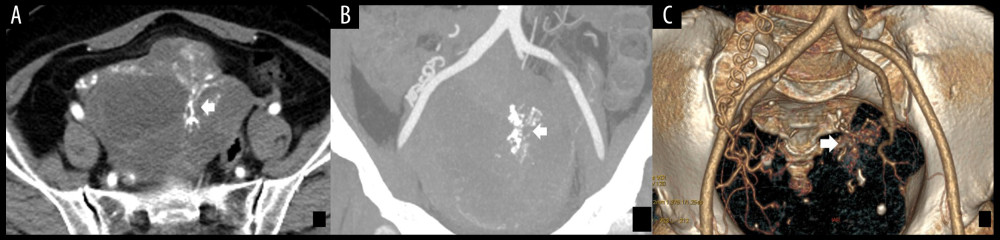 Figure 2. (A) The enhanced axial multidetector computed tomography images of a 65-year-old female with SMOTs showed a solid-cystic mass with relatively thick wall and thick septa, with serpentine and chaotic course of vessels and microaneurysms (arrow). (B, C) The reformat in MIP and VR algorithm. Serpentine and chaotic course of vessels and multiple microaneurysms in the solid parts of the tumor (arrow). SMOTs – serous malignant ovarian tumors; MIP – maximal intensity projection; VR – volume rendering.
Figure 2. (A) The enhanced axial multidetector computed tomography images of a 65-year-old female with SMOTs showed a solid-cystic mass with relatively thick wall and thick septa, with serpentine and chaotic course of vessels and microaneurysms (arrow). (B, C) The reformat in MIP and VR algorithm. Serpentine and chaotic course of vessels and multiple microaneurysms in the solid parts of the tumor (arrow). SMOTs – serous malignant ovarian tumors; MIP – maximal intensity projection; VR – volume rendering. 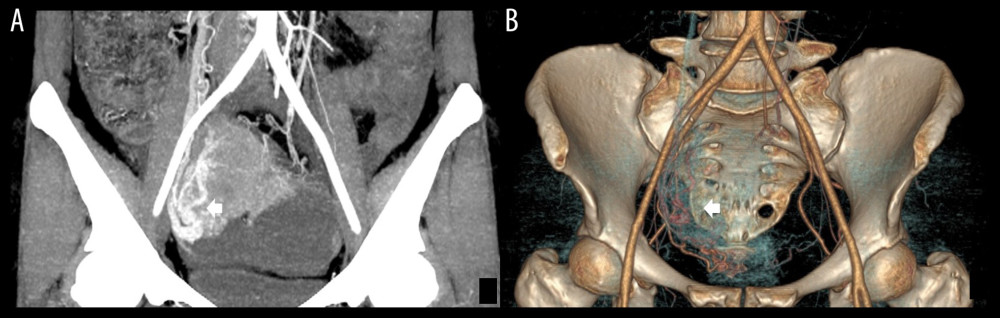 Figure 3. (A, B) Multidetector computed tomography arterial phase of a 67-year old woman with SMOT. The reformat in MIP and VR algorithm. Early venous outflow as an indirect sign of arteriovenous shunting in solid parts of the tumor (arrow). SMOT – serous malignant ovarian tumor; MIP – maximal intensity projection; VR – volume rendering.
Figure 3. (A, B) Multidetector computed tomography arterial phase of a 67-year old woman with SMOT. The reformat in MIP and VR algorithm. Early venous outflow as an indirect sign of arteriovenous shunting in solid parts of the tumor (arrow). SMOT – serous malignant ovarian tumor; MIP – maximal intensity projection; VR – volume rendering. 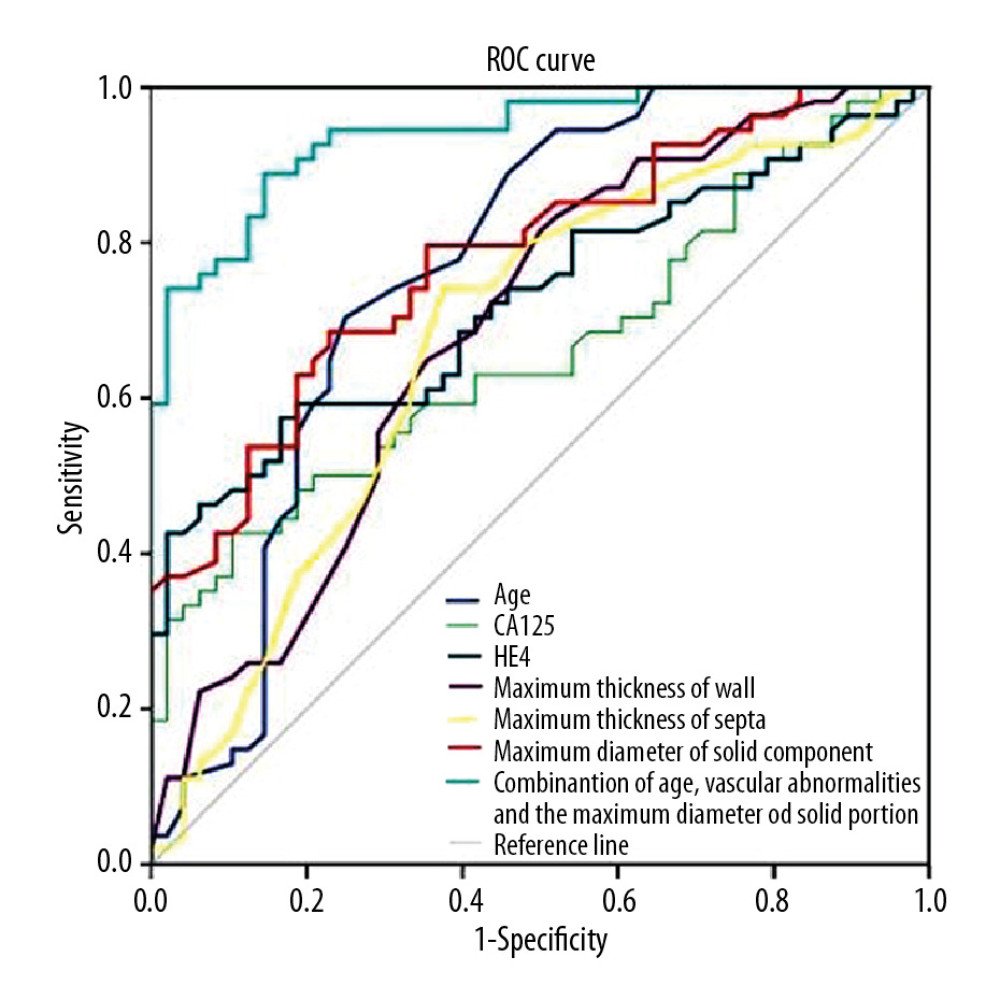 Figure 4. Receiver operating characteristic curves for age, CA125, HE4, maximum thickness of wall, maximum thickness of septa, maximum diameter of solid component and combination of age, vascular abnormalities and maximum diameter of solid component in differentiating SBOTs and SMOTs. CA125 – cancer antigen 125; HE4 – human epididymis protein 4; SBOTs – serous borderline ovarian tumors; SMOTs – serous malignant ovarian tumors.
Figure 4. Receiver operating characteristic curves for age, CA125, HE4, maximum thickness of wall, maximum thickness of septa, maximum diameter of solid component and combination of age, vascular abnormalities and maximum diameter of solid component in differentiating SBOTs and SMOTs. CA125 – cancer antigen 125; HE4 – human epididymis protein 4; SBOTs – serous borderline ovarian tumors; SMOTs – serous malignant ovarian tumors. Tables
Table 1. Clinical characteristics of SBOTs and SMOTs.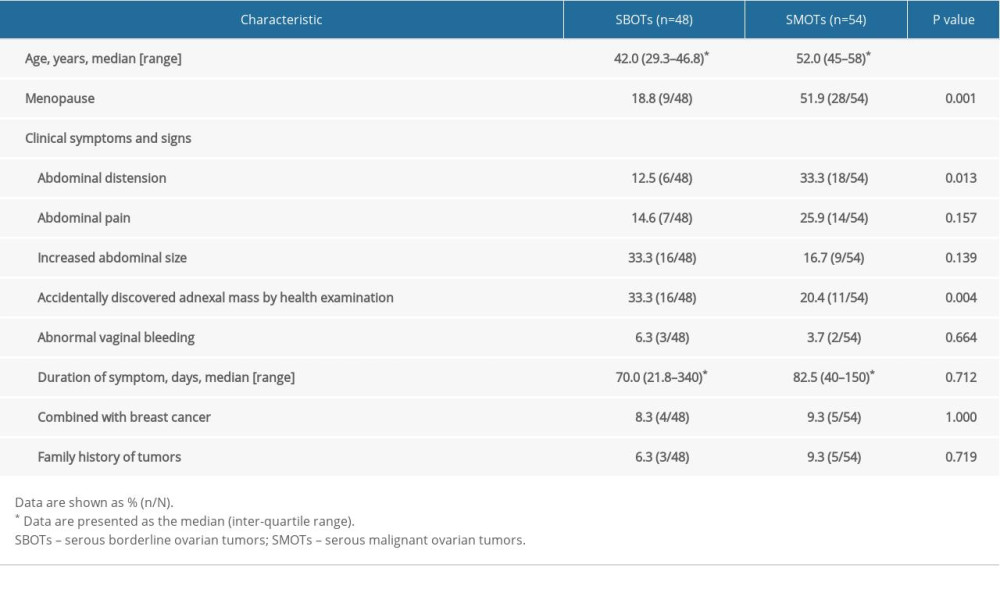 Table 2. Comparison of qualitative MDCT features of SBOTs and SMOTs.
Table 2. Comparison of qualitative MDCT features of SBOTs and SMOTs.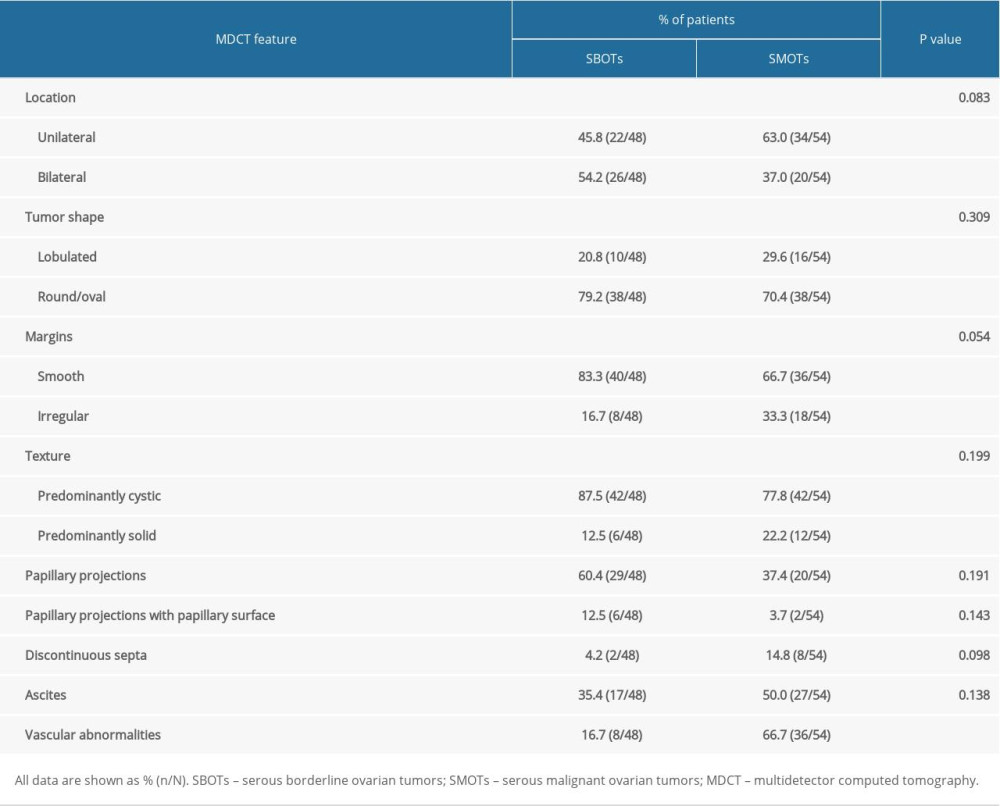 Table 3. Comparison of quantitative measures of SBOTs and SMOTs.
Table 3. Comparison of quantitative measures of SBOTs and SMOTs.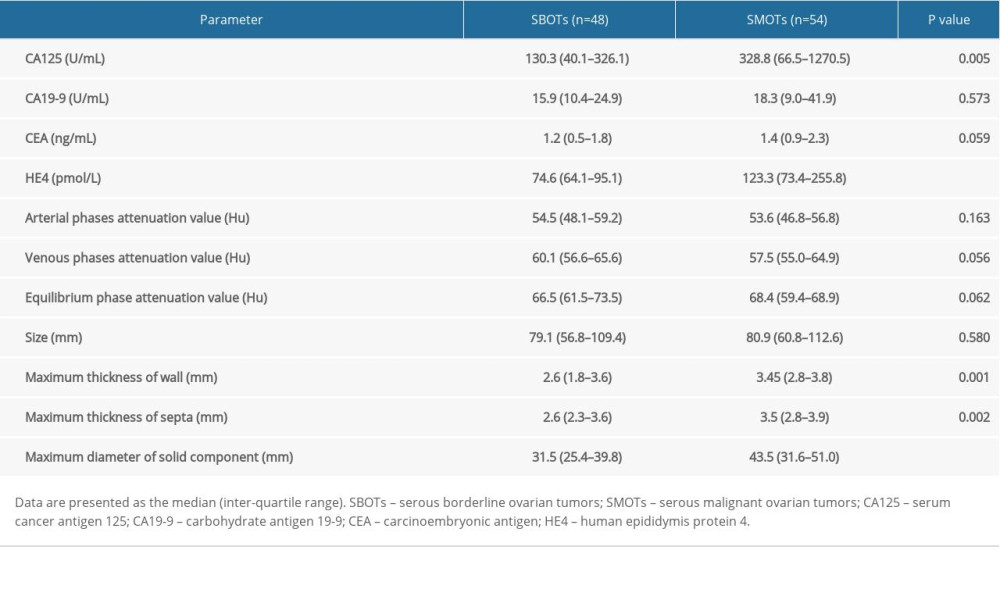 Table 4. Predicting SMOTs by multivariate analysis of age, tumor markers and MDCT features.
Table 4. Predicting SMOTs by multivariate analysis of age, tumor markers and MDCT features.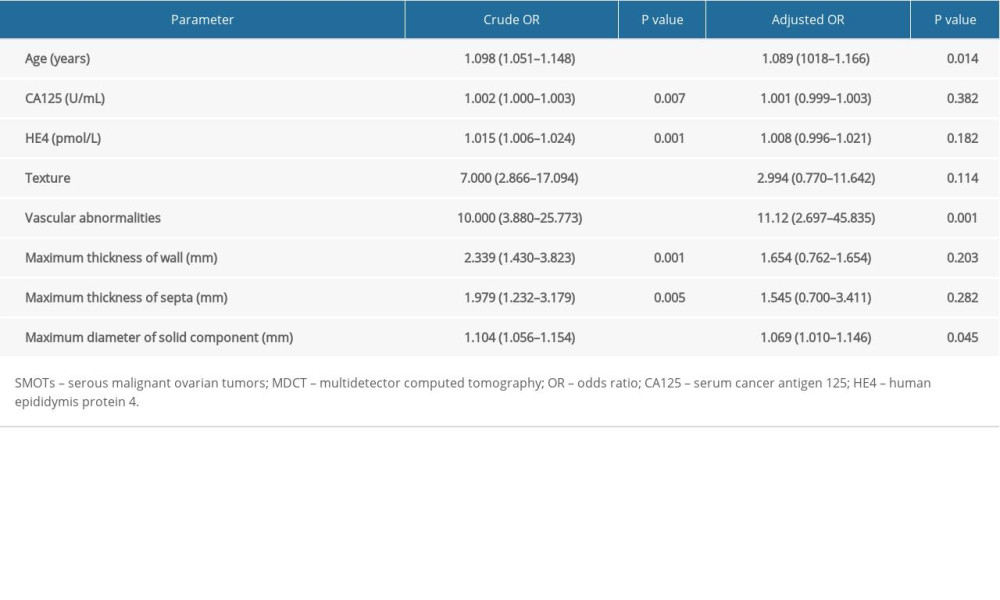 Table 5. Diagnostic performance of tumor markers and MDCT parameter for predicting SMOTs by ROC analyses.
Table 5. Diagnostic performance of tumor markers and MDCT parameter for predicting SMOTs by ROC analyses.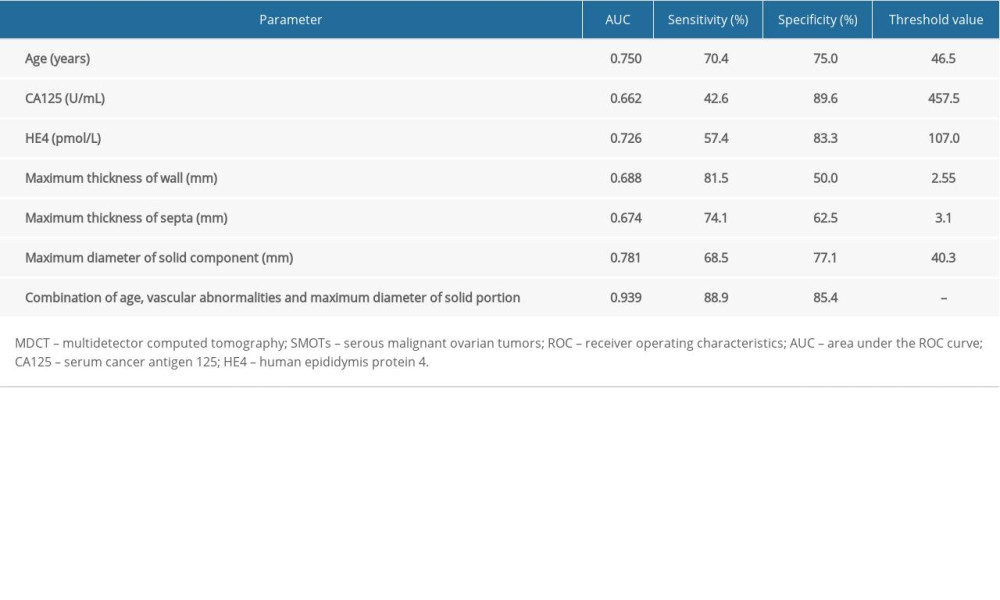 Table 6. The interobserver reproducibility of MDCT features.
Table 6. The interobserver reproducibility of MDCT features.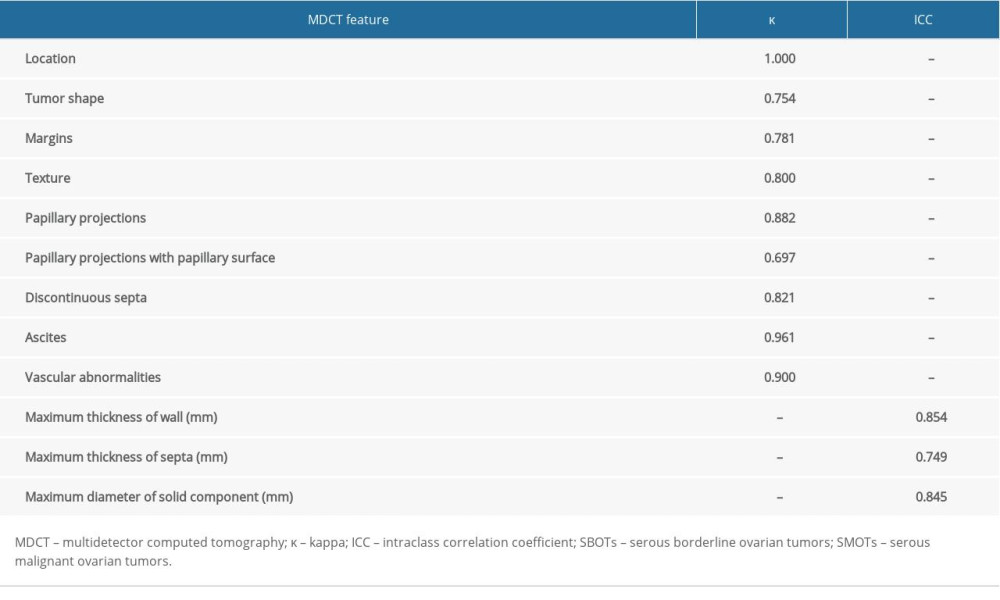
References
1. Lheureux S, Gourley C, Vergote I, Oza AM, Epithelial ovarian cancer: Lancet, 2019; 393(10177); 1240-53
2. Prat J, Pathology of borderline and invasive cancers: Best Pract Res Clin Obstet Gynaecol, 2017; 41; 15-30
3. Hart WR, Borderline epithelial tumors of the ovary: Mod Pathol, 2005; 18(Suppl 2); S33-50
4. Fischerova D, Zikan M, Dundr P, Cibula D, Diagnosis, treatment, and follow up of borderline ovarian tumors: Oncologist, 2012; 17(12); 1515-33
5. Morotti M, Menada MV, Gillott DJ, The preoperative diagnosis of borderline ovarian tumors: A review of current literature: Arch Gynecol Obstet, 2012; 285(4); 1103-12
6. Bentivegna E, Gouy S, Maulard A, Fertility-sparing surgery in epithelial ovarian cancer: a systematic review of oncological issues: Ann Oncol, 2016; 27(11); 1994-2004
7. Kawamoto S, Urban BA, Fishman EK, CT of epithelial ovarian tumors: Radiographics, 1999; 19(Spec No); S85-264
8. Jung SE, Lee JM, Rha SE, CT and MR imaging of ovarian tumors with emphasis on differential diagnosis: Radiographics, 2002; 22(6); 1305-25
9. Tsili AC, Argyropoulou MI, Adnexal incidentalomas on multidetector CT: How to manage and characterise: J Obstet Gynaecol, 2019 [Online ahead of print]
10. deSouza NM, O’Neill R, McIndoe GA, Borderline tumors of the ovary: CT and MRI features and tumor markers in differentiation from stage I disease: Am J Roentgenol, 2005; 184(3); 999-1003
11. Nougaret S, Lakhman Y, Molinari N, CT features of ovarian tumors: Defining key differences between serous borderline tumors and low-grade serous carcinomas: Am J Roentgenol, 2018; 210(4); 918-26
12. Naqvi J, Nagaraju E, Ahmad S, MRI appearances of pure epithelial papillary serous borderline ovarian tumours: Clin Radiol, 2015; 70(4); 424-32
13. Grabowska-Derlatka L, Derlatka P, Palczewski P, Differentiation of ovarian cancers from borderline ovarian tumors on the basis of evaluation of tumor vascularity in multi-row detector computed tomography – comparison with histopathology: Int J Gynecol Cancer, 2013; 23(9); 1597-602
14. Muinao T, Deka Boruah HP, Pal M, Multi-biomarker panel signature as the key to diagnosis of ovarian cancer: Heliyon, 2019; 5(12); e02826
15. Ferraro S, Braga F, Lanzoni M: J Clin Pathol, 2013; 66(4); 273-81
16. Scaletta G, Plotti F, Luvero D, The role of novel biomarker HE4 in the diagnosis, prognosis and follow-up of ovarian cancer: A systematic review: Expert Rev Anticancer Ther, 2017; 17(9); 827-39
17. Lin J, Qin J, Sangvatanakul V, Human epididymis protein 4 for differential diagnosis between benign gynecologic disease and ovarian cancer: A systematic review and meta-analysis: Eur J Obstet Gynecol Reprod Biol, 2013; 167(1); 81-85
18. Guo J, Yu J, Song X, Mi H, Serum CA125, CA199 and CEA combined detection for epithelial ovarian cancer diagnosis: A meta-analysis: Open Med (Wars), 2017; 12; 131-37
19. Park SY, Oh YT, Jung DC, Differentiation between borderline and benign ovarian tumors: Combined analysis of MRI with tumor markers for large cystic masses (>/=5 cm): Acta Radiologica, 2016; 57(5); 633-39
20. Denewar FA, Takeuchi M, Urano M, Multiparametric MRI for differentiation of borderline ovarian tumors from stage I malignant epithelial ovarian tumors using multivariate logistic regression analysis: Eur Journal Radiol, 2017; 91; 116-23
21. Kurokawa R, Nakai Y, Gonoi W, Differentiation between ovarian metastasis from colorectal carcinoma and primary ovarian carcinoma: Evaluation of tumour markers and “mille-feuille sign” on computed tomography/magnetic resonance imaging: Eur J Radiol, 2020; 124 108823
22. Javadi S, Ganeshan DM, Qayyum A, Ovarian cancer, the revised FIGO staging system, and the role of imaging: Am J Roentgenol, 2016; 206(6); 1351-60
23. Kurman RJ, Carcangiu ML, Herrington CS, Young RH: WHO classification of tumours of female reproductive organs, 2014; 6, Geneva, Switzerland, WHO Press
24. Gershenson DM, Management of borderline ovarian tumours: Best Pract Res Clin Obstet Gynaecol, 2017; 41; 49-59
25. Webb PM, Purdie DM, Grover S, Symptoms and diagnosis of borderline, early and advanced epithelial ovarian cancer: Gynecol Oncol, 2004; 92(1); 232-39
26. Timmerman D, Testa AC, Bourne T, Simple ultrasound-based rules for the diagnosis of ovarian cancer: Ultrasound Obstet Gynecol, 2008; 31(6); 681-90
27. Kinkel K, Lu Y, Mehdizade A, Indeterminate ovarian mass at US: Incremental value of second imaging test for characterization – meta-analysis and Bayesian analysis: Radiology, 2005; 236(1); 85-94
28. Sohaib SA, Mills TD, Sahdev A, The role of magnetic resonance imaging and ultrasound in patients with adnexal masses: Clin Radiol, 2005; 60(3); 340-48
29. Jeong YY, Outwater EK, Kang HK, Imaging evaluation of ovarian masses: Radiographics, 2015; 20(5); 1445-70
30. Guo B, Lian W, Liu S, Comparison of diagnostic values between CA125 combined with CA199 and ultrasound combined with CT in ovarian cancer: Oncol Lett, 2019; 17(6); 5523-28
31. Jeong TD, Cho EJ, Ko DH, A new strategy for calculating the risk of ovarian malignancy algorithm (ROMA): Clin Chem Lab Med, 2017; 55(8); 1209-14
Figures
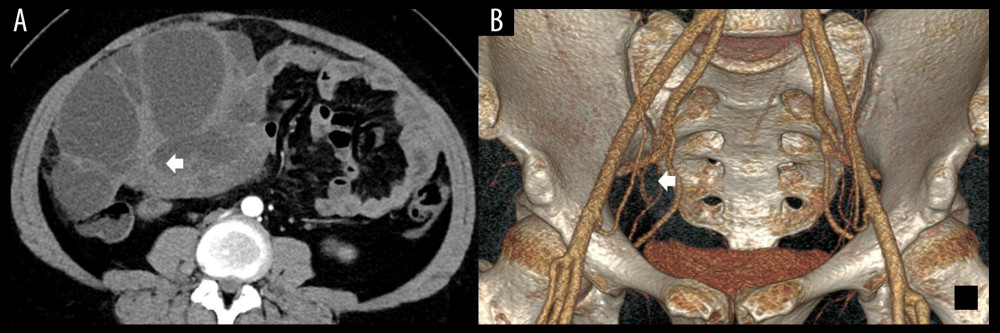 Figure 1. (A) The enhanced axial multidetector computed tomography images of a 32-year-old female with SBOTs showed a solid-cystic mass with thick wall and thick septa (arrow); however, with few vascular abnormalities in the endophytic part of the tumor. (B) The reformat in VR algorithm. Scant tiny vessels in the endophytic part of the tumor (arrow). SBOTs – serous borderline ovarian tumors; VR – volume rendering.
Figure 1. (A) The enhanced axial multidetector computed tomography images of a 32-year-old female with SBOTs showed a solid-cystic mass with thick wall and thick septa (arrow); however, with few vascular abnormalities in the endophytic part of the tumor. (B) The reformat in VR algorithm. Scant tiny vessels in the endophytic part of the tumor (arrow). SBOTs – serous borderline ovarian tumors; VR – volume rendering.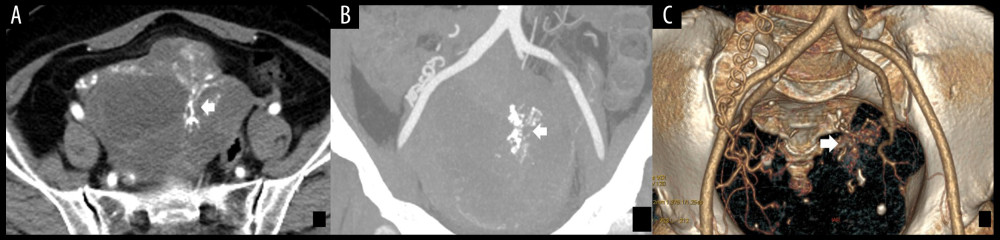 Figure 2. (A) The enhanced axial multidetector computed tomography images of a 65-year-old female with SMOTs showed a solid-cystic mass with relatively thick wall and thick septa, with serpentine and chaotic course of vessels and microaneurysms (arrow). (B, C) The reformat in MIP and VR algorithm. Serpentine and chaotic course of vessels and multiple microaneurysms in the solid parts of the tumor (arrow). SMOTs – serous malignant ovarian tumors; MIP – maximal intensity projection; VR – volume rendering.
Figure 2. (A) The enhanced axial multidetector computed tomography images of a 65-year-old female with SMOTs showed a solid-cystic mass with relatively thick wall and thick septa, with serpentine and chaotic course of vessels and microaneurysms (arrow). (B, C) The reformat in MIP and VR algorithm. Serpentine and chaotic course of vessels and multiple microaneurysms in the solid parts of the tumor (arrow). SMOTs – serous malignant ovarian tumors; MIP – maximal intensity projection; VR – volume rendering.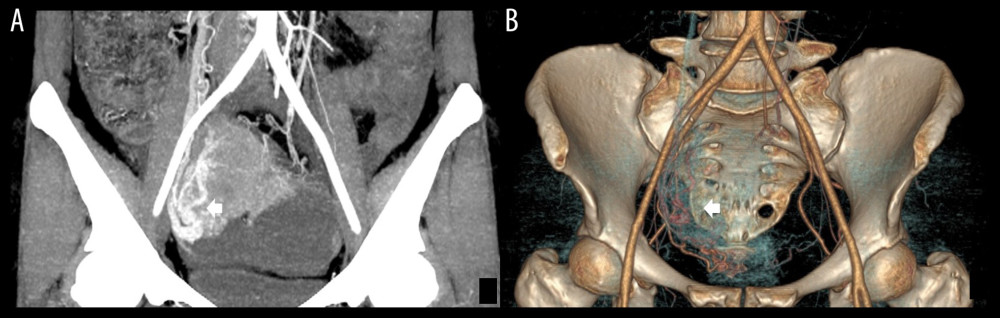 Figure 3. (A, B) Multidetector computed tomography arterial phase of a 67-year old woman with SMOT. The reformat in MIP and VR algorithm. Early venous outflow as an indirect sign of arteriovenous shunting in solid parts of the tumor (arrow). SMOT – serous malignant ovarian tumor; MIP – maximal intensity projection; VR – volume rendering.
Figure 3. (A, B) Multidetector computed tomography arterial phase of a 67-year old woman with SMOT. The reformat in MIP and VR algorithm. Early venous outflow as an indirect sign of arteriovenous shunting in solid parts of the tumor (arrow). SMOT – serous malignant ovarian tumor; MIP – maximal intensity projection; VR – volume rendering.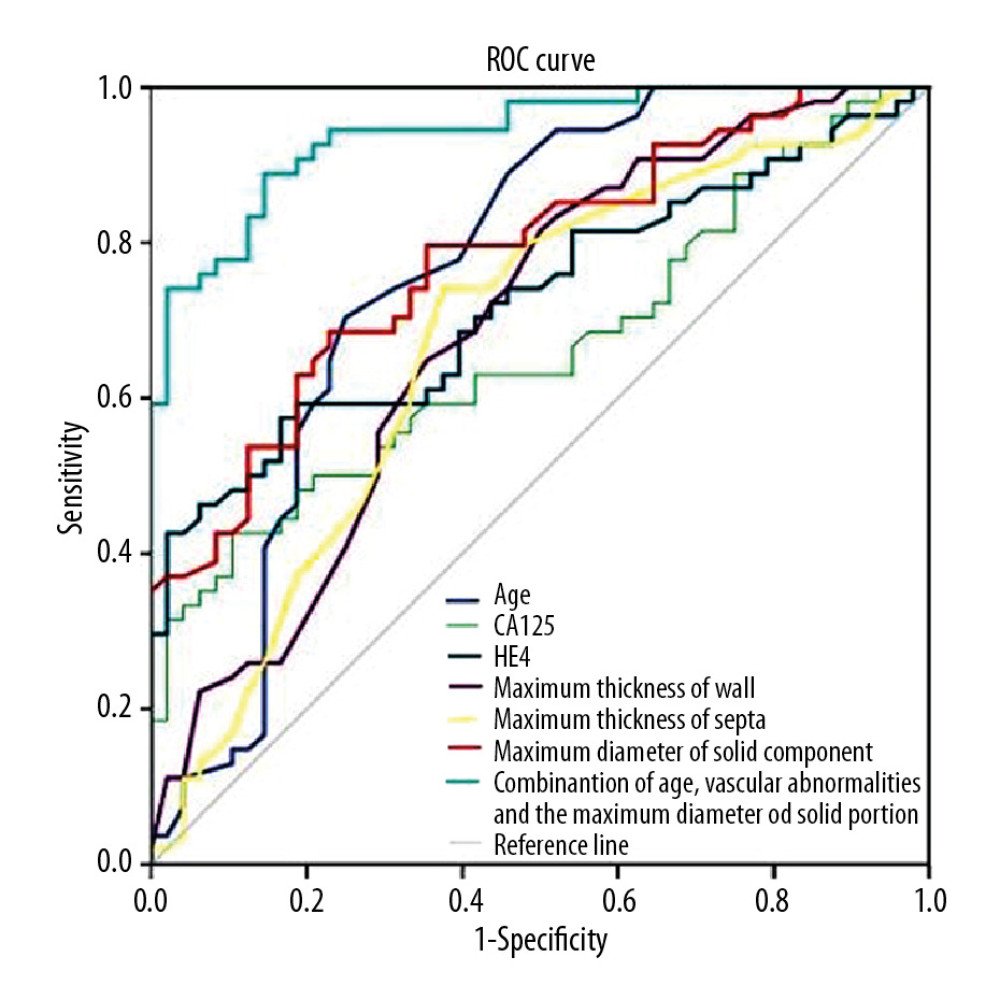 Figure 4. Receiver operating characteristic curves for age, CA125, HE4, maximum thickness of wall, maximum thickness of septa, maximum diameter of solid component and combination of age, vascular abnormalities and maximum diameter of solid component in differentiating SBOTs and SMOTs. CA125 – cancer antigen 125; HE4 – human epididymis protein 4; SBOTs – serous borderline ovarian tumors; SMOTs – serous malignant ovarian tumors.
Figure 4. Receiver operating characteristic curves for age, CA125, HE4, maximum thickness of wall, maximum thickness of septa, maximum diameter of solid component and combination of age, vascular abnormalities and maximum diameter of solid component in differentiating SBOTs and SMOTs. CA125 – cancer antigen 125; HE4 – human epididymis protein 4; SBOTs – serous borderline ovarian tumors; SMOTs – serous malignant ovarian tumors. Tables
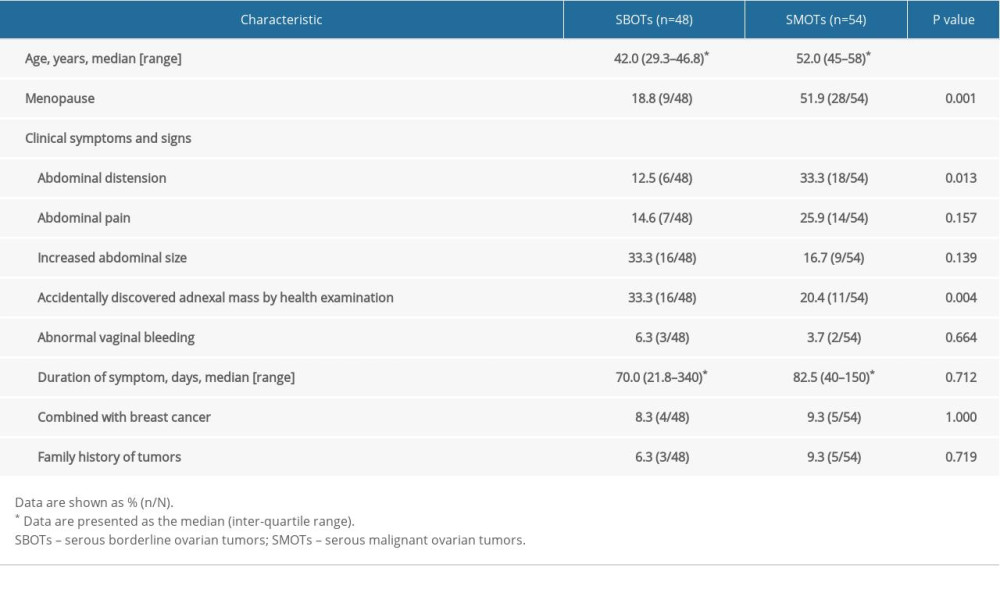 Table 1. Clinical characteristics of SBOTs and SMOTs.
Table 1. Clinical characteristics of SBOTs and SMOTs.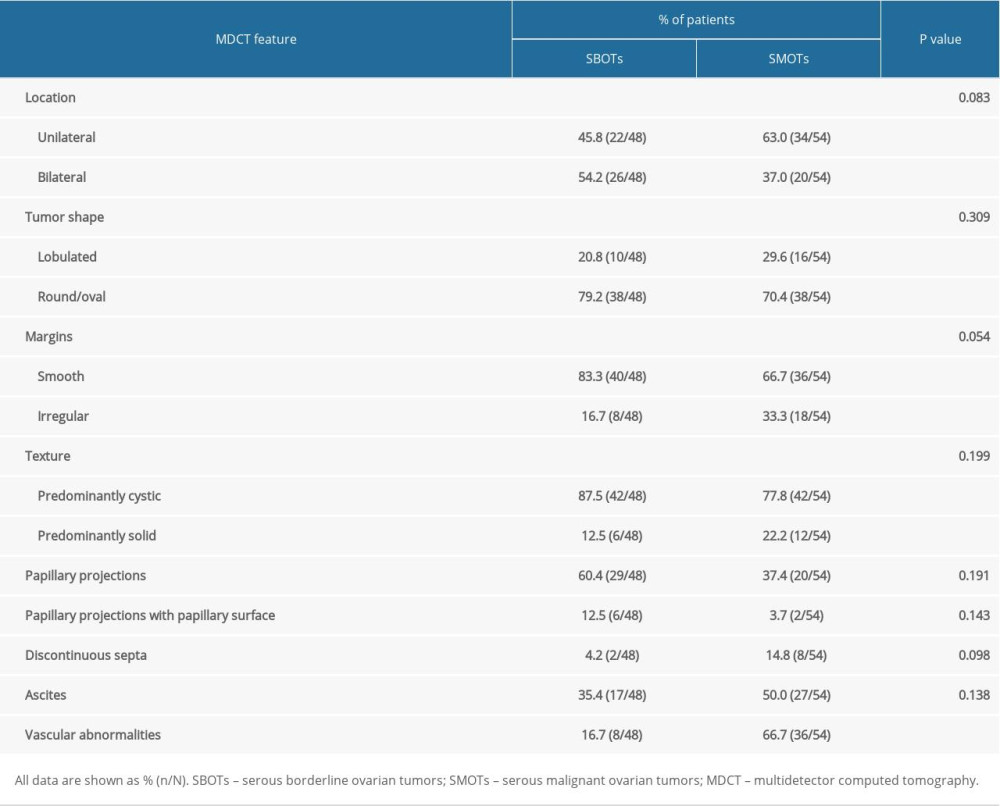 Table 2. Comparison of qualitative MDCT features of SBOTs and SMOTs.
Table 2. Comparison of qualitative MDCT features of SBOTs and SMOTs.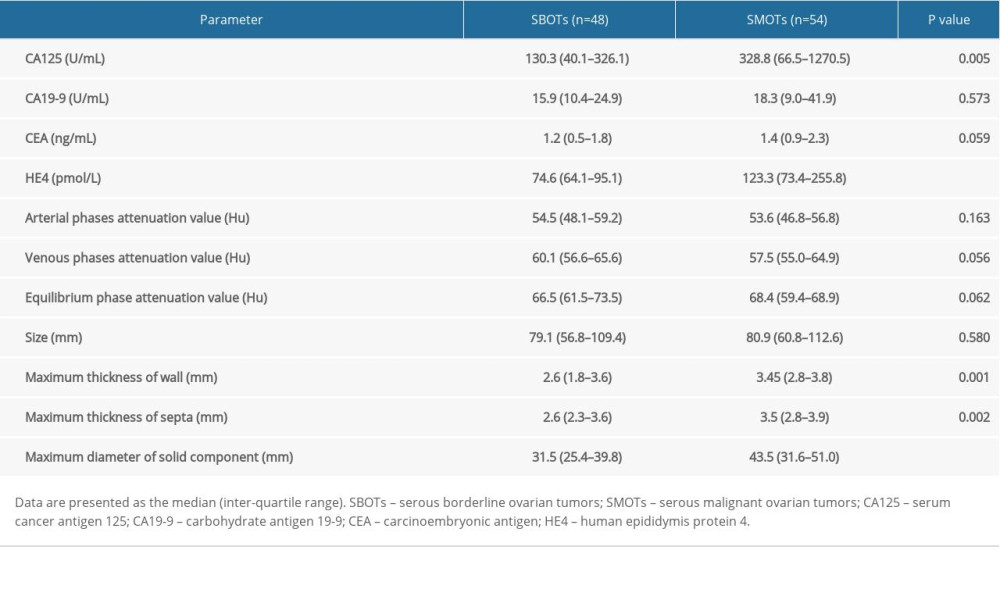 Table 3. Comparison of quantitative measures of SBOTs and SMOTs.
Table 3. Comparison of quantitative measures of SBOTs and SMOTs.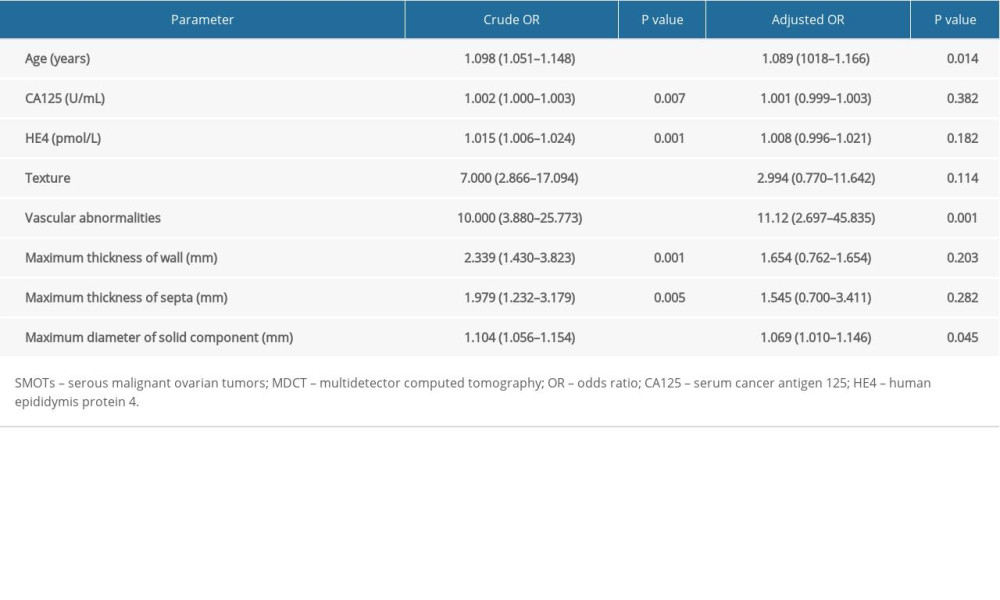 Table 4. Predicting SMOTs by multivariate analysis of age, tumor markers and MDCT features.
Table 4. Predicting SMOTs by multivariate analysis of age, tumor markers and MDCT features.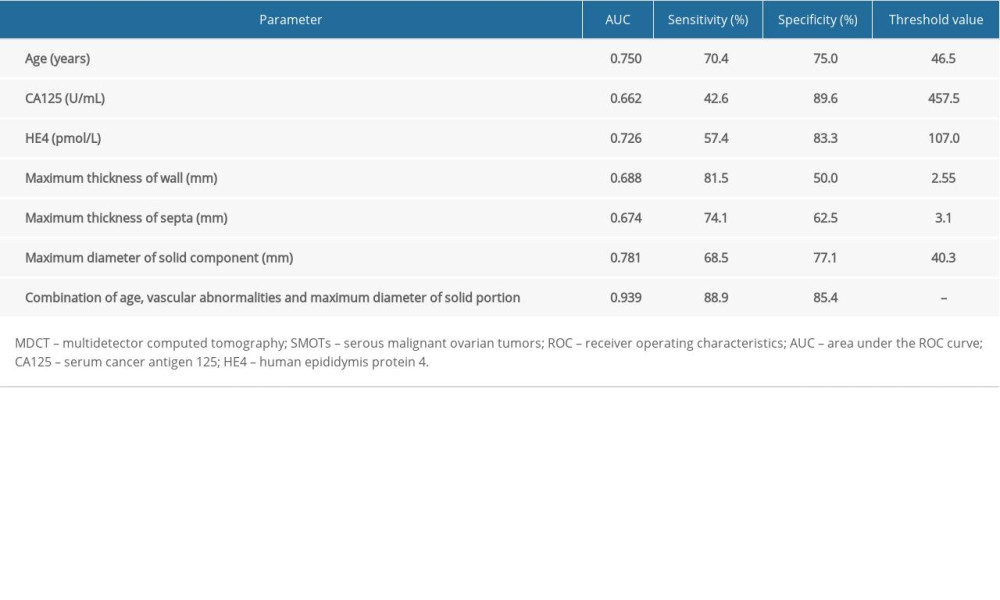 Table 5. Diagnostic performance of tumor markers and MDCT parameter for predicting SMOTs by ROC analyses.
Table 5. Diagnostic performance of tumor markers and MDCT parameter for predicting SMOTs by ROC analyses.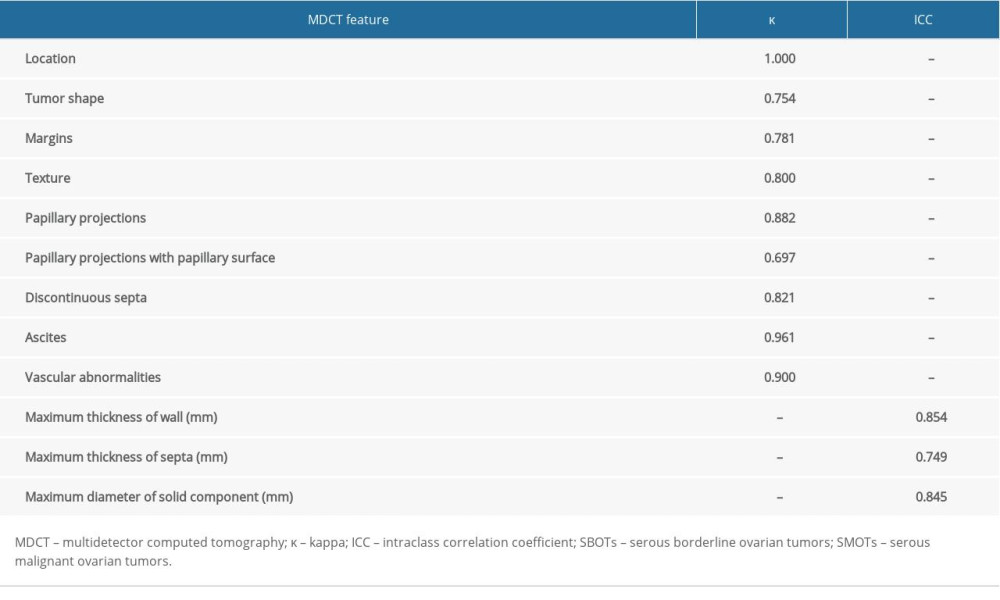 Table 6. The interobserver reproducibility of MDCT features.
Table 6. The interobserver reproducibility of MDCT features.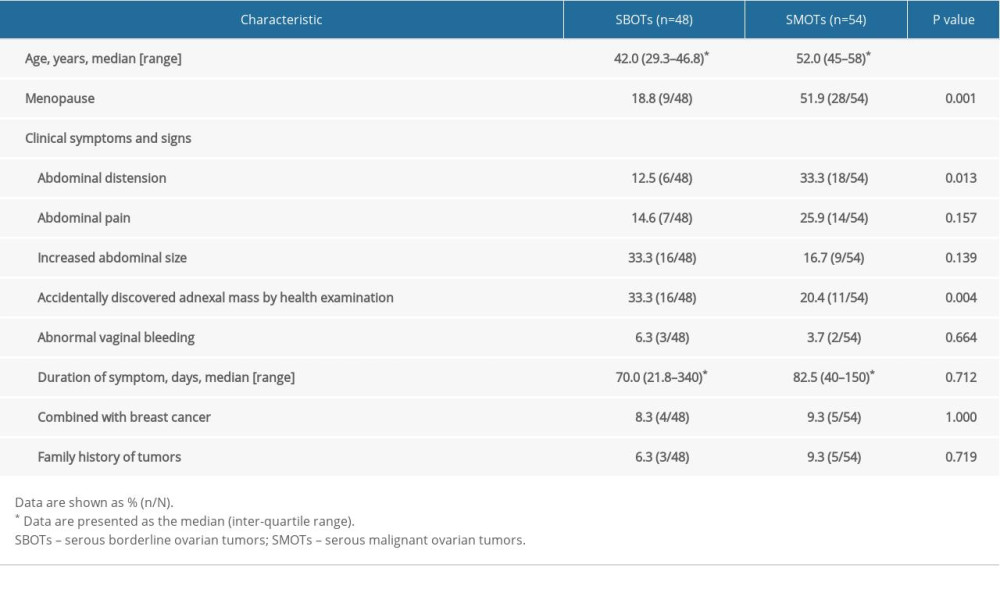 Table 1. Clinical characteristics of SBOTs and SMOTs.
Table 1. Clinical characteristics of SBOTs and SMOTs.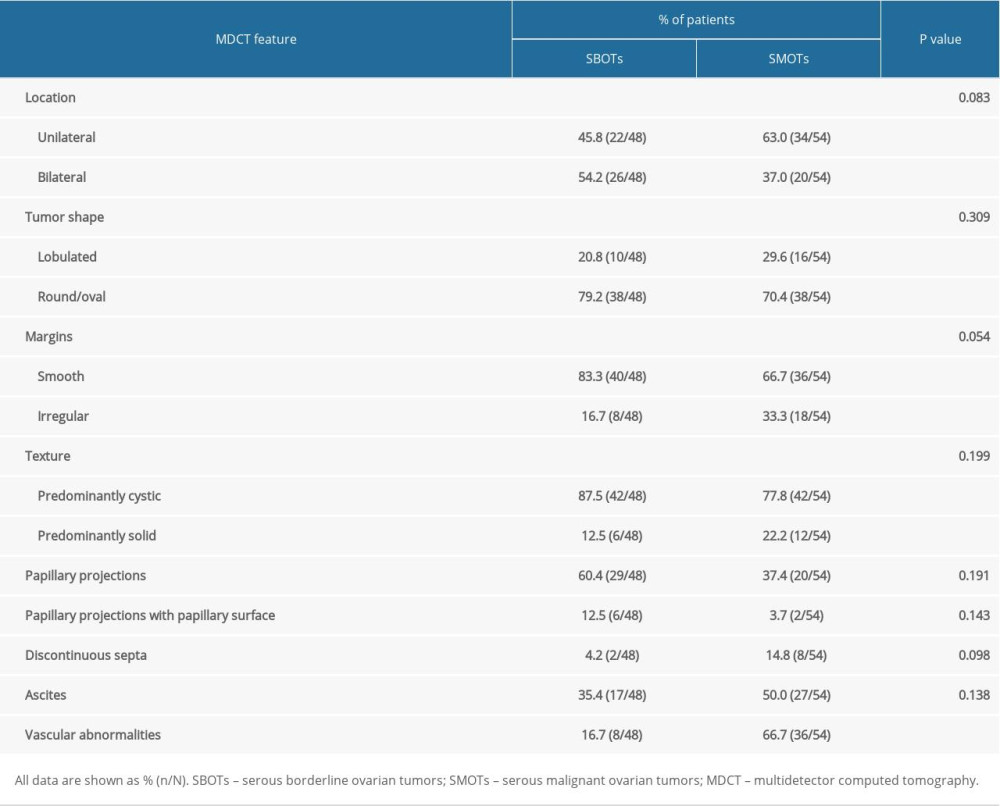 Table 2. Comparison of qualitative MDCT features of SBOTs and SMOTs.
Table 2. Comparison of qualitative MDCT features of SBOTs and SMOTs.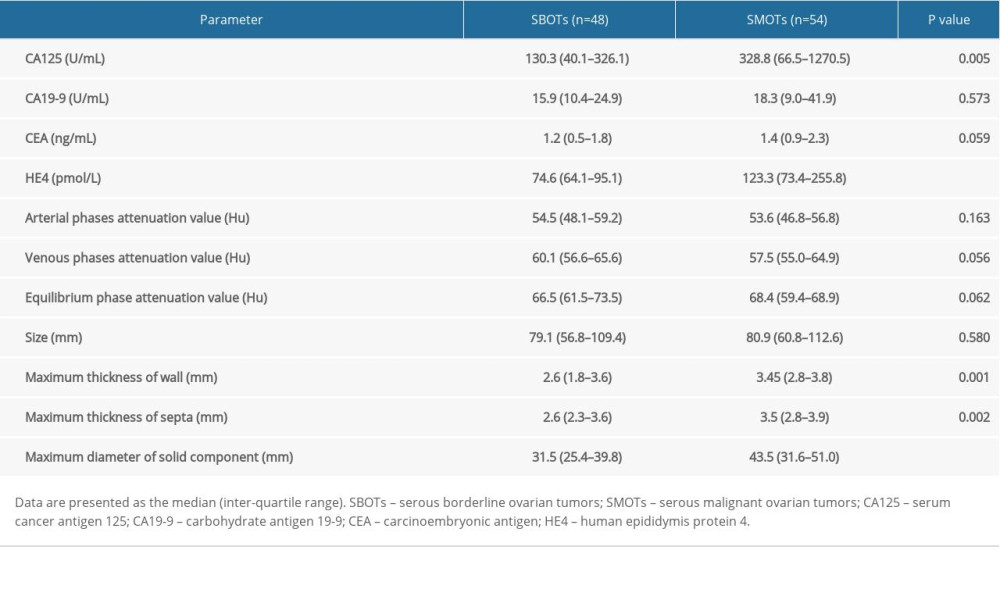 Table 3. Comparison of quantitative measures of SBOTs and SMOTs.
Table 3. Comparison of quantitative measures of SBOTs and SMOTs.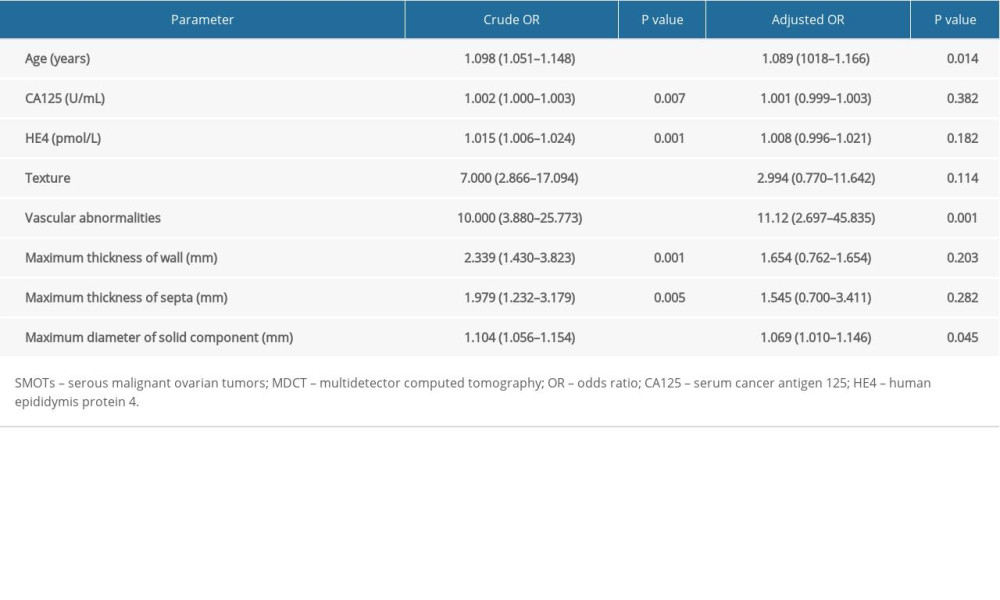 Table 4. Predicting SMOTs by multivariate analysis of age, tumor markers and MDCT features.
Table 4. Predicting SMOTs by multivariate analysis of age, tumor markers and MDCT features.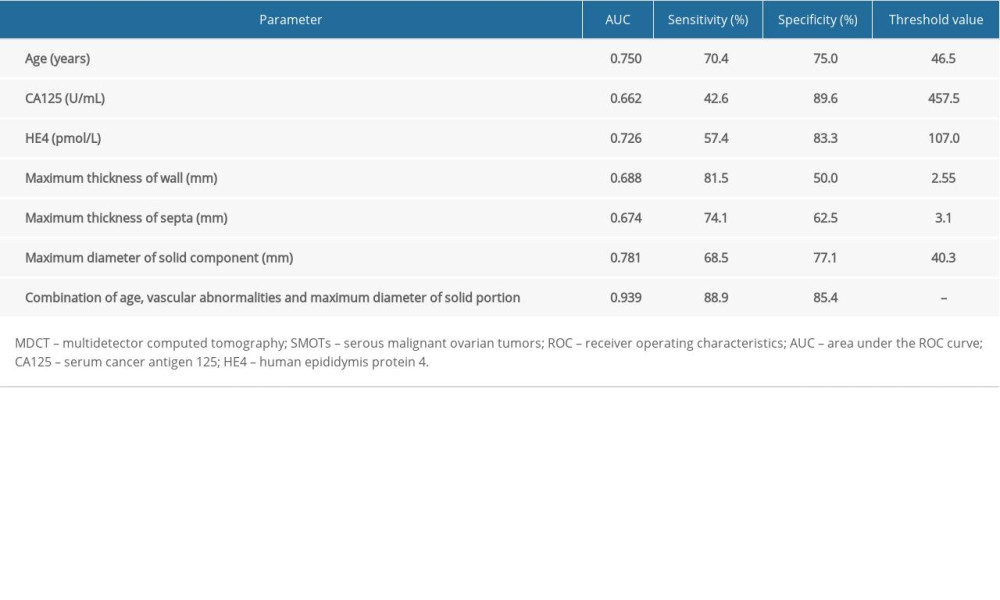 Table 5. Diagnostic performance of tumor markers and MDCT parameter for predicting SMOTs by ROC analyses.
Table 5. Diagnostic performance of tumor markers and MDCT parameter for predicting SMOTs by ROC analyses.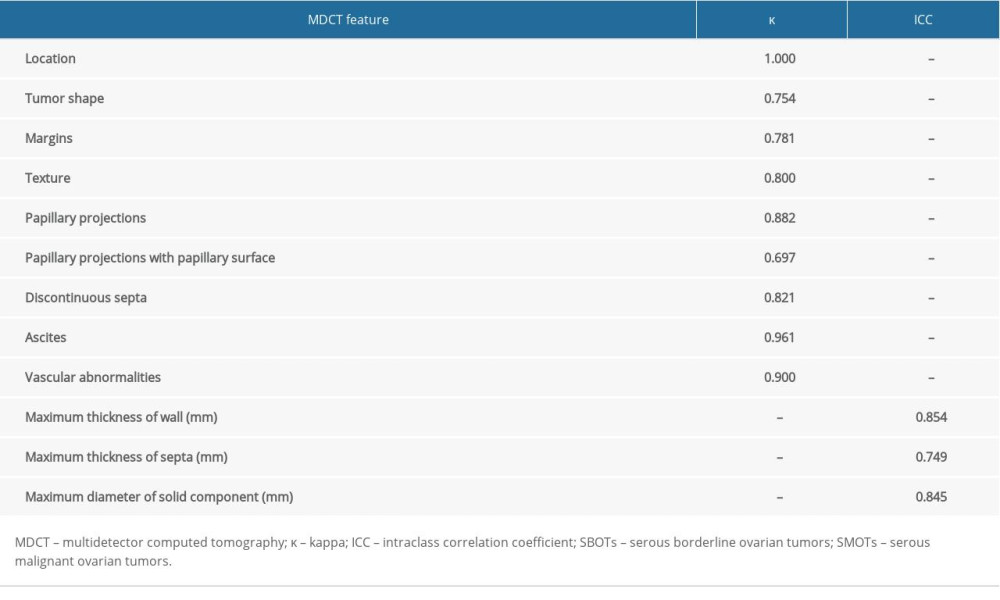 Table 6. The interobserver reproducibility of MDCT features.
Table 6. The interobserver reproducibility of MDCT features. In Press
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








