23 August 2021: Human Study
Influence of Severe Thoracic Trauma on Choosing the Correct Surgical Strategy in Patients with Polytrauma from Kosovo
Shqiptar DemaçiDOI: 10.12659/MSMBR.932463
Med Sci Monit Basic Res 2021; 27:e932463
Abstract
BACKGROUND: BACKGROUND Severe thoracic trauma (TT) has a significant impact on the selection of treatment strategy in patients with polytrauma. Our aim was to assess the impact of severe TT on choosing the optimal surgical procedure to decrease mortality. MATERIAL AND METHODS Overall, 66 patients with polytrauma and significant TT were analyzed. Demographic data, trauma history, admittance imaging, injury details, injury severity scores, conservative treatment, surgical treatment, days of hospital stay, and mortality data were gathered. Frequencies of thoracic surgical procedures and other treatments were collected and compared with those in the literature. RESULTS All patients had Abbreviated Injury Scale (AIS) scores of thorax >3. Injuries to extremities and/or the osseous pelvis accounted for 50% of injuries; 47.0% included the head and/or neck; 45.5% were external injuries; and 27.3% were abdominal injuries or included pelvic organs and/or lumbar spine. Mean prehospital time was 40.3 min. Mean time from trauma occurrence to tertiary treatment was 125 min. Blunt TT (BTT) was recorded in 59 patients (89.4%), and penetrant TT (PTT) was recorded in 7 patients (10.6%). Thoracic drainage, urgent thoracotomy and laparotomy were recorded procedures. The mean Injury Severity Score (ISS) of all patients was 31.17. Nine patients died (13.6%) and had BTT with a mean ISS of 48.44. The Trauma Injury Severity Score for BTT injuries was 77.08% and for PTT, 85.6%. CONCLUSIONS Factors that decreased hospital stay and mortality and increased survival included arriving in time after injury, aggressive reanimation/intensive care, and mandatory thoracic surgical procedure combined with laparotomy.
MATERIAL AND METHODS:
RESULTS:
CONCLUSIONS:
Keywords: Injury Severity Score, Multiple Trauma, Thoracic Surgery, Thoracic Surgical Procedures, Thorax, Kosovo, Thoracic Injuries, Wounds, Nonpenetrating
Background
Severe thoracic trauma (TT) has a significant impact on the selection of treatment strategy for patients with polytrauma. Patients with severe TT have a higher probability of having complexities and mortality than do patients with the same severity score but without accompanying TT [1–4]. Patients with severe TT also need longer mechanical ventilation [2–4]. On average, TT occurs in 15% to 20% of injuries [2,3], with blunt TT (BTT) being the most frequent type of trauma. Frequent causes of TT are traffic accidents, falls, and other injuries [3,4].
The influence of TT on the entire clinical picture of polytrauma creates a dilemma of selecting the correct surgical and intensive care procedures [5]. For instance, TT hypoxemia is a major contributor to developing multiple organ failure, and patients with TT hypoxemia might need intubation and positive pressure ventilation [6]. Moreover, the intercostal tube is required in cases of fractured ribs and pulmonary contusions with chest wall fractures [7,8]. Reanimation is usually also done during advanced trauma life support as an important option to ensure the correct treatment in patients with polytrauma [4]. Meanwhile, thoracotomy is necessary as a definitive treatment in only 10% to 15% of thoracic injuries. Recently, chest computed tomography (CT) has been proposed as a diagnostic tool to exclude occult injuries; therefore, the use of thoracotomies might decrease over time [9,10]. There is still controversy over selecting the most appropriate treatment options and surgical procedures. Owing to the application of different procedures, the aim of this study was to identify the optimal surgical treatment procedure in patients with polytrauma and severe TT to decrease mortality.
Material and Methods
The study was conducted at the University Clinical Center of Kosovo (UCCK) in Pristina, which also serves as a tertiary center of trauma, admitting patients to the Emergency Department (ED), Intensive Care Unit (ICU), and Surgical Clinic, including the Orthopedy and Traumatology departments.
The data were collected retrospectively from the records of patients with polytrauma and significant TT who were admitted to the center during a period of 2 years, from January 2010 to December 2011. The records included demographic data, such as patient age and sex, analysis of time as a factor of clinical procedures (tertiary adequate aid), analysis of the Revised Trauma Score (RTS) at admission and the Injury Severity Score (ISS). The patients were scored according to the RTS physiologic score and Abbreviated Injury Scale (AIS-90) anatomic score. The AIS-90 score was used for calculating the ISS by summarizing the square of 3 most severe injuries on 3 different anatomic regions with the following formula: ISS=(AIS thorax1)2+(AIS2)2+(AIS3)2.
The patient records also included the probability of survival, which was analyzed using the Trauma and Injury Severity Score (TRISS) after calculating the ISS, RTS and age, according to the nature of the injury (blunt or penetrating trauma).
The inclusion criteria were as follows: mechanism of thoracic injury of patients with severity ISS ≥16; AIS thorax ≥3 and AIS head and neck ≤2; analysis of imaging (chest X-rays or computed tomography [CT]) within the “golden hour” (1 h from injury) or later and its impact on definitive results; analysis of mandatory treatment, including surgery, such as thoracostomy tube drainage/thoracotomy and laparotomy, or reanimation; relation of epicrisis/clinical decursus vs the ISS, RTS and TRISS. This study excluded patients with burn injuries from chemical substances, patients with polytrauma without significant TT (AIS thorax <3, AIS head/neck ≥2, and ISS <16), and patients with thoracic monotrauma.
Statistical analyses of the data were performed using SPSS version 21 (IBM, Armonk, NY, USA). The
Results
Overall, 8563 patients with trauma were admitted to the UCCK in 2010 and 2011, with only 196 (2.29%) patients affected by polytrauma. Of them, 66 patients had severe thoracic injury, 59 (89%) patients had BTT, and 7 (11%) patients had penetrating TT (PTT). The mechanisms of injury in 63.6% of patients were traffic accidents (51.5% as drivers/passengers and 12.1% as pedestrians) and in 10.6% were weapon assaults (7.6% firearms and 3.0% cold weapons). Other cases included falls and accidents during work.
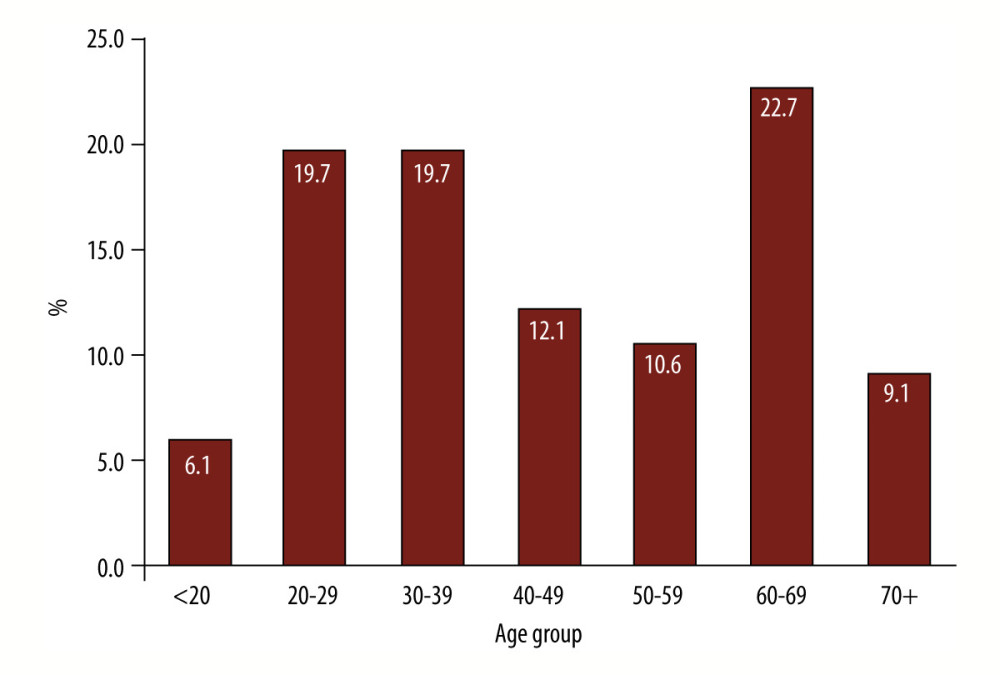
The mean age of patients was 46.1 years, with most patients in the age group of 60 to 69 years (Figure 1). The distribution of sex was 51 men (77.3%) and 15 women (22.7%). All patients had thoracic injury with an AIS thorax score >3, according to the severity of trauma. The anatomical regions of injuries are presented in Table 1.
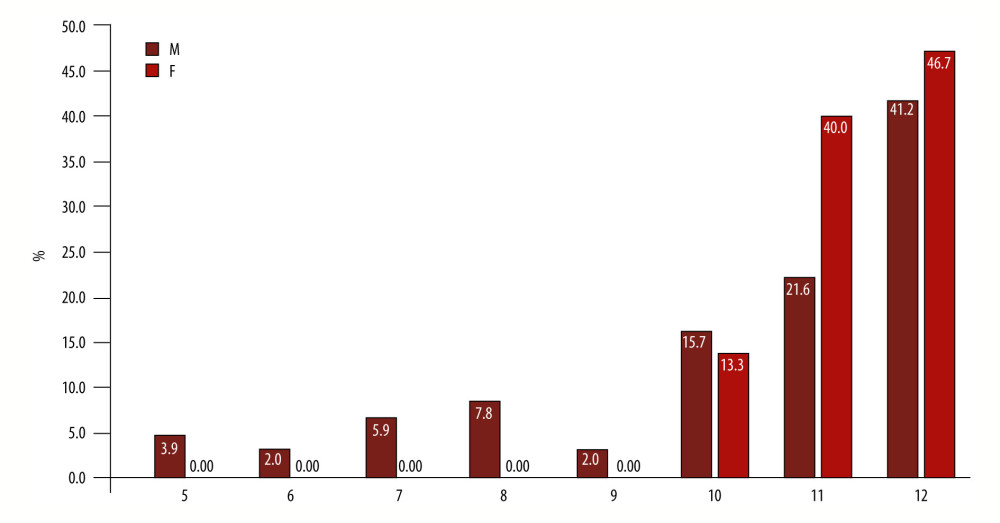
The average prehospital time, or golden hour, was 40.3±20.9 min. Prehospital times were divided into 4 groups, according to the RTS, ranging from a minimal recorded score of 5 to a maximal recorded score of 12: RTS of 5–6, 7–8, 9–10, and 11–12. There was a statistically significant difference in prehospital time (
Table 3 shows the surgical procedures that were undertaken as treatment options in our center. A thoracic drain was needed by most patients, followed in frequency by abdominal surgery. Early CT of the chest within 1 h after injury occurred in 1 patient with urgent thoracotomy, 15 patients with thoracic drainage, 4 patients with urgent laparotomy, 2 patients with orthopedic immobilization, and 2 patients with a counter indication for thoracic drainage (minimal hemothorax and minimal pneumothorax). BTT was registered in 59 (89.4%) patients with the following mechanisms: traffic accidents in 42 patients (63.3%), falls in 11 (16.7%) patients, injuries during work in 6 (9.1%) patients. PTT occurred in 7 patients (10.6%).
Thoracic drainage was used in 43 (65.1%) patients, urgent thoracotomy in 5 patients (7.6%), bundling together in 48 (72.7%) patients with thoracic surgical treatment. Drainage lasted an average of 7.4±3.5 days. Laparotomy was conducted in 9 patients (13.6%).
The mean amount of blood after initial drainage was 411±442.3 mL. Four hours after drainage, the mean amount of blood was 275±170.8 mL. Six patients were given blood from 1 to 8 doses of fresh plasma (mean amount was 4 doses). Six patients were given 1 to 3 doses of fresh plasma (mean amount was 1.8 doses).
The outcome of surgical procedures resulted in 9 (13.6%) deaths. One (1.5%) patient was in coma vigile (permanent vegetative state), 1 (1.5%) patient was still on mechanic ventilation at the time of analysis, 9 (13.6%) patients were transferred from the thoracic surgery ward to other departments, and 46 (69.7%) patients were released from the hospital (Table 4). The RTS at admission was associated with different outcomes (F=14.1,
Discussion
Severe TT is a frequent cause of death in patients with polytrauma; however, studies have had contradictory results in morbidity and mortality rates in such patients [11–13]. Severe TT in patients with polytrauma has a significant influence on choosing the right surgical strategy or treatment in EDs and ICUs. Thus, the aim of this study was to observe the influence of severe TT on the management of patients with polytrauma. In our analysis, 66 patients with polytrauma and severe thoracic injuries with AIS thorax >3 were evaluated. Of the total, 51 patients (77.3%) were men and 15 (22.7%) were women, indicating male sex is more prone to severe injuries.
The mean age of patients in our study was 46.1 years (±17.9). By comparison, Vécsei et al investigated 501 patients with polytrauma, and a majority with BTT, who had a mean age of 37.7 years [14]. In a study by Chrysou et al [15], injuries were more common among older adults, compared with the group of patients below 50 years of age. Moreover, in our study, 22.7% of patients were between 60 and 69 years of age. The patients in this age group needed special evaluation and treatment owing to the high mortality rate which follows such trauma. An age of more than 50 years has been identified as an independent predicting factor of mortality and morbidity in patients with TT [16]. For instance, the probability of death increases by 132% with every decade of age. Older adults with rib fractures are also more prone to develop complications than are younger patients [15]. Therefore, early surgical management might prevent such conditions (eg, pneumonia) and consequently also death in these individuals [17].
More than half of our patients (n=39, 59.1%) needed treatment in the ICU, which expressed the gravity or seriousness of thoracic injury in our study. Patients with polytrauma with TT had a significant extension of days on mechanical ventilation (2 days vs 8 days) and stayed longer in the ICU (4 days vs 11 days), compared with the patients with polytrauma without TT [18]. More than half of the patients in the study by Chrysou et al [15] had chest tube thoracostomy (54.5%) and most were admitted to the ED. However, only 10% of patients with polytrauma had surgical procedures for their chest injuries. Most frequently this followed unsuccessful nonoperative treatment, for instance unresolving pneumothorax, despite thoracic drainage. Furthermore, they had contradictory findings that the severity of BTT, based on the AIS, did not correlate with the hospital and ICU length of stay, the time of mechanical ventilation, complications, and mortality rates [15]. The observations of Veysi et al were similar [19]. In contrast, Beshay et al [20] showed that the severity of TT correlated with the hospital and ICU lengths of stay, the time of mechanical ventilation, complications, and mortality rates. The findings of Beshay et al agree with our results.
The RTS is ideal for immediate triage of the injured person and is scored after admission. The TRISS indicates the probability of survival, which is calculated with the ISS, RTS, and age of the patient. In the present study, the mean ISS of 66 patients was 31.17, and the mean ISS of 9 patients resulting with exitus at admission or during clinical decursus was 48.44. A high TTS >9, high AIS >3, and severe lung contusion have been recorded as predictors of mortality and morbidity in patients with TT [16]. The present results confirmed the ISS as an accurate score for death prediction. ISS is also a consistent factor of risk for prediction of multiple organ failure after injury [21]. Veysi et al [19] showed that patients with higher scores had a higher risk of developing multiple organ failure, higher morbidity, and mortality.
The mortality rate of our cohort was 13.6% (9 of 66 patients), which is a much higher percentage than that of the cohort of Chrysou et al [15], which had a mortality rate of only 5.5%. According to their report, no fatalities were correlated with TT, which might have been owing to well-developed prehospital trauma management, short traveling distances to the hospital centers, and the readiness of healthcare teams. In the present study, the mean prehospital time (golden hour) of our patients was 40.3 min. Transportation of patients in such a short time was possible because the maximal distance from all regional hospitals to the Tertiary Center of Trauma in Kosovo is only 80 km. The time from injuries to definitive tertiary care was on average 125 min, with 99.4 min in male patients and 236 min in female patients. Sex discrimination was observed toward female patients, who were processed in a slower time. This could be explained as a coincidence or a consequence of the level of alarm and setting up for the respective injury. As observed, a higher proportion of patients were men; therefore, the severity of injuries was more serious when patient sex was male. Time management is crucial in patients with high ISS and AIS. Thoracic vascular and neurologic trauma are the most common causes of death during the first hour after hospital admission. The presence of an experienced interdisciplinary trauma team is mandatory to ensure high-quality management with low morbidity and mortality rates in these patients [20]. This was confirmed in a study by Bary et al [16], where morbidity and mortality rates in patients with TT showed direct correlation with the severity of TT and the presence of a thoracic surgeon as a part of the trauma team.
A CT scan of the thorax is recommended in the primary diagnostic evaluation of multiple injuries with suspicion of TT. The aim of a CT scan is to reduce complications and increase improvement of results of polytraumatic patients with BTT. In the present study, an early CT scan of the thorax within the golden hour was performed as an early intervention in 1 patient with urgent thoracotomy, 15 patients with thoracic drainage, 4 patients with urgent laparotomies, 2 patients requiring orthopedic immobilization, and 2 patients who were contraindicated to thoracic drainage (minimal hemothorax and minimal pneumothorax). Two patients had a clear indication for surgery: the first had an open traumatic pneumothorax and the second had a median laparotomy. Sampson et al, who investigated 97 cases of pneumothorax detected with CT, found 12 were bilateral, 52 had a chest tube in situ, and 36 were not detected on supine position of chest X-ray [22]. In the present study, pneumothorax was detected in 30.3% of patients with TT, hemothorax was detected in 34.9%, and hemopneumothorax was detected in 34.8%. Hemopericardia was diagnosed in 2 patients (3%), pneumomediastinum in 2 (3%), widened mediastinum in 2 (3%), massive pleural fistula in 1 (1.5%), subcutaneous emphysema in 10 (15.2%), and intrapulmonary hematoma in 25 (37.9%). Fractured ribs were recorded in 44 (66.7%) patients, of which 8 patients (12.1%) had bilateral fractures. These significant injuries confirmed the severity and seriousness of the thoracic injuries in our patients.
Thoracic drainage was performed in 36 (54.5%) patients, whereas bilateral thoracic drain was performed in 7 (10.6%), with a mean duration of 7.4 days. Adegboye et al reported thoracic drainage in 346 (58.8%) of 597 patients with PTT [23]. Furthermore, in the present study, 6 patients were treated with an average of 4 doses of fresh plasma and 6 were given, on average, 1.8 doses of fresh plasma. Recent studies have shown an improvement of results with the early use of plasma and platelets. However, many clinicians have concluded that the optimal time and quantity of blood for treatment of patients with hypothermia, coagulopathy, and acidosis is still uncertain [24].
In the present study, mandatory surgical intervention was used in 43 (65.1%) patients (thoracic drainage in 36 [54.5%] and bilateral thoracic drainage in 7 [10.6%]), urgent thoracotomy in 5 (7.6%), abdominal surgery in 9 (13.6%), and thoracic surgery in 5 patients, combined particularly with abdominal surgery. Frequencies of surgeries identified in the literature were 15.0% (181/1206) and 79.9% (612/766) in patients with thoracic and abdominal trauma (
In the present study, there was no registered emergent thoracotomy noted in the patient records. Nishiumi et al [26] emphasized that emergency thoracotomy with pulmonary lobectomy should be performed before a hemorrhage reaches an amount of 1200 mL to decrease mortality [26]. In our study, a high percentage of mortality and morbidity was determined according to epicrisis, cumulatively 13.6%+13.6%=27.2%. There was no measurement of invalidity for patients who were transferred to other wards or discharged from the hospital. Hildebrand et al [18] reported that mortality of young patients was 0% to 5% with isolated TT, whereas in older adult patients mortality reached 10% to 15%, comparable to our results. Mortality with multitrauma reached 40%, whereas thoracic monotrauma was responsible for 20% to 25% of deaths correlated with trauma, and approximately 50% to 75% of patients who died from trauma had TT [18].
Although the present study is one of the largest studies of TT in our region, it has some limitations. The analysis was done retrospectively from the records of patients, which could have resulted in missing data. The sample size was relatively small owing to the stringent inclusion criteria. This was also designed as a single-center study. Further studies are needed to evaluate the influence of different treatment methods on the outcome of patients with polytrauma and severe TT, or a comparison study of trauma centers should be conducted.
Conclusions
Severe thoracic trauma in patients with polytrauma has a significant influence on surgical strategy. Men are much more prone than are women to severe injuries that require different surgical strategies and treatment procedures. The RTS at admission was associated with different outcomes and was lower in patients who died than in patients who were transferred to other departments or released from the hospital. The mean ISS of patients who died was higher and indicated an accurate score for death prediction. Factors that decreased hospital stay and mortality and increased survival included arriving in time after injury, aggressive reanimation/intensive care, and mandatory thoracic surgical procedure combined with laparotomy.
Tables
Table 1. Basic characteristics of patients at admission with anatomical regions of injuries.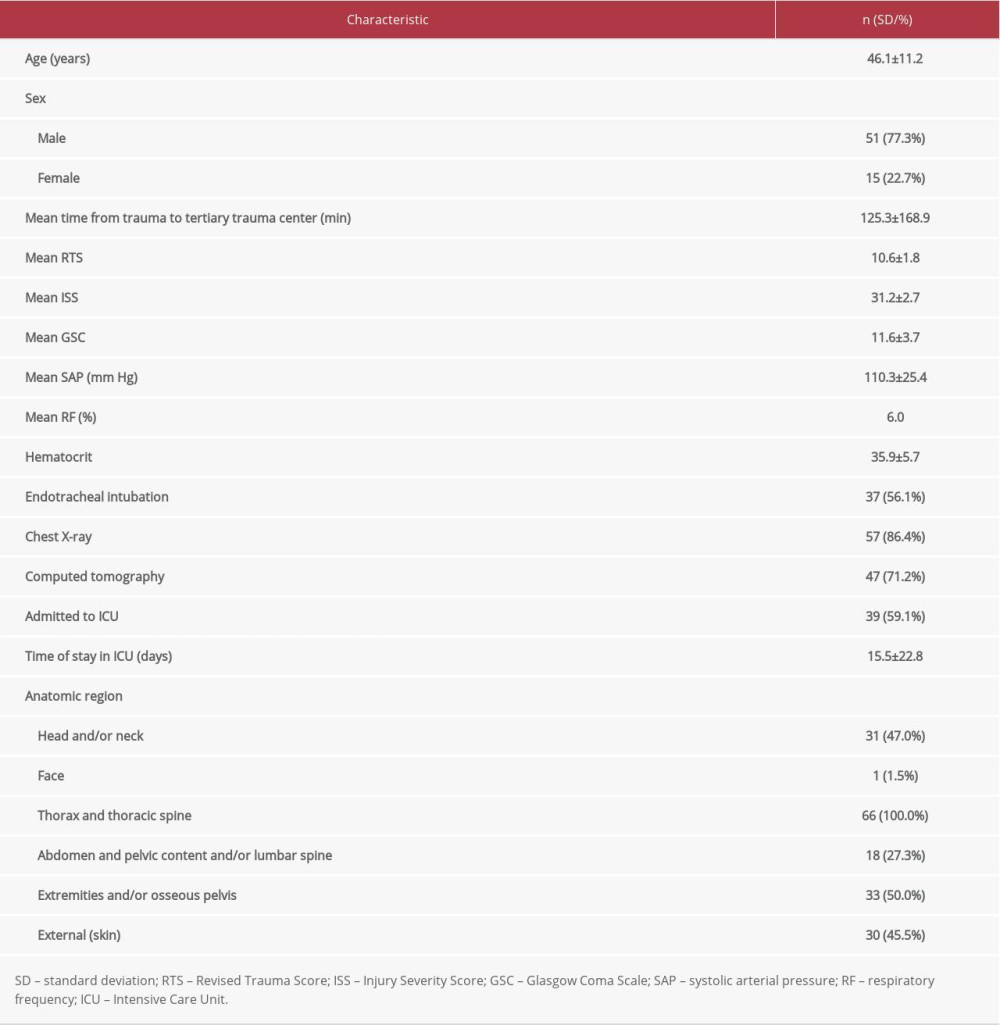 Table 2. Prehospital time by 4 Revised Trauma Score groups.
Table 2. Prehospital time by 4 Revised Trauma Score groups. Table 3. Surgical procedures conducted in patients with polytrauma.
Table 3. Surgical procedures conducted in patients with polytrauma.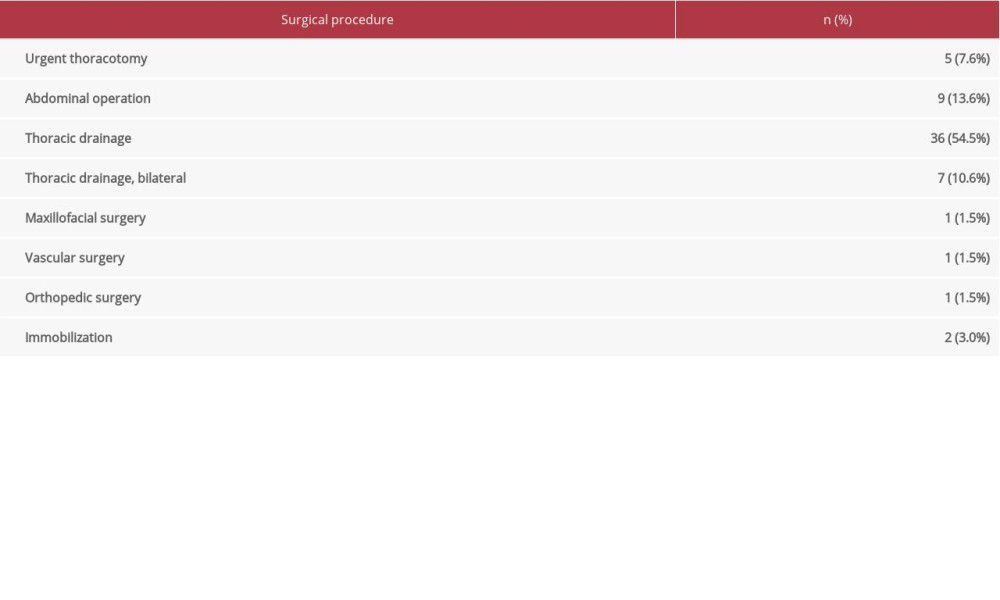 Table 4. Relationship between Revised Trauma Score at admission and epicrisis.
Table 4. Relationship between Revised Trauma Score at admission and epicrisis.
References
1. Abdel Bary M, Branscheid D, Mertzlufft F, Beshay M, Long term management of thoracic trauma in a high frequency trauma center; What have we learned?: J Egypt Soc Cardiothorac Surg, 2018; 26; 73-81
2. Abdelghany A, Abu Arab W, Allam A, Karara K, Emergency thoracotomy: Experience of one year in a large tertiary trauma center: J Egypt Soc Cardiothorac Surg, 2016; 24; 188-93
3. Paniker J, Graham SM, Harrison JW, Global trauma: The great divide: SICOT J, 2015; 1; 19
4. Haagsma JA, Graetz N, Bolliger I, The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013: Inj Prev, 2016; 22(1); 3-18
5. Marsden NJ, Tuma F, Polytraumatized patient: StatPearls [Internet] Jan, 2021, Treasure Island (FL), StatPearls Publishing
6. Smith N, Weyman D, Findlay G, The management of trauma victims in England and Wales: A study by the National Confidential Enquiry into Patient Outcome and Death: Eur J Cardiothorac Surg, 2009; 36(2); 340-43
7. Huber S, Biberthaler P, Haeberle STrauma Register DGU: Scand J Trauma Resusc Emerg Med, 2014; 3(22); 52
8. Ludwig C, Koryllos A, Management of chest trauma: J Thorac Dis, 2017; 9(Suppl.3); S172-77
9. Huber-Wagner S, Biberthaler P, Haeberle S, Whole-body CT in haemodynamically unstable severely injured patients – a retrospective, multicentre study: PLoS One, 2013; 8; e68880
10. Lotfipour S, Kaku SK, Vaca FE, Factors associated with complications in older adults with isolated blunt chest trauma: West J Emerg Med, 2009; 10; 79-84
11. Lecky FE, Bouamra O, Woodford M, Epidemiology of Polytrauma: Damage control management in the polytrauma patient, 2010; 13-24, New York, Springer
12. Hildebrand F, Giannoudis PV, Griensven M, Management of patients with polytrauma with associated blunt chest trauma: A comparison of two European countries: Injury, 2005; 36; 293-302
13. Grubmüller M, Kerschbaum M, Diepold E, Severe thoracic trauma – still an independent predictor for death in multiple injured patients?: Scand J Trauma Resusc Emerg Med, 2018; 26(1); 6
14. Vécsei V, Arbes S, Aldrian S, Nau Th, Chest injuries in polytrauma: Eur J Trauma, 2005; 31(3); 239-43
15. Chrysou K, Halat G, Hoksch B, Lessons from a large trauma center: Impact of blunt chest trauma in polytrauma patients-still a relevant problem?: Scand J Trauma Resusc Emerg Med, 2017; 25(1); 42
16. Bary MA, Brandscheid D, Mertzlufft F, Beshay M, Long term management of thoracic trauma in a high frequency trauma center; What have we learned?: J Egypt Cardiothorac Surg, 2018; 26; 73-81
17. Kocher GJ, Sharafi S, Azenha LF, Schmid RA, Chest wall stabilization in ventilator-dependent traumatic flail chest patients: Who benefits?: Eur J Cardiothorac Surg, 2017; 51(4); 696-701
18. Hildebrand F, van Griensven M, Garapati R, Diagnostic and scoring in blunt chest trauma: Eur J Trauma Emerg Surg, 2002; 28; 157-67
19. Veysi VT, Nikolaou VS, Paliobeis C, Prevalence of chest trauma, associated injuries and mortality: A level I trauma centre experience: Int Orthop, 2009; 33(5); 1425-33
20. Beshay M, Mertzlufft F, Kottkamp HW, Analysis of risk factors in thoracic trauma patients with a comparison of a modern trauma centre: A mono-centre study: World J Emerg Surg, 2020; 15(1); 45
21. Lecky F, Woodford M, Edwards A, Trauma scoring systems and databases: Br J Anaesth, 2014; 113(2); 286-94
22. Sampson MA, Colquhoun KBM, Hennessy NLM, Computed tomography whole body imaging in multi-trauma: 7 years experience: Clin Radiol, 2006; 61(4); 365-69
23. Adegboye VO, Ladipo JK, Brimmo IA, Adebo AO, Penetrating chest injuries in civilian practice: Afr J Med Sci, 2001; 30(4); 327-31
24. Holcomb JB, Optimal use of blood products in severely injured trauma patients: Hematology Am Soc Hematol Educ Program, 2010; 2010; 465-69
25. Gao JM, Gao YH, Zeng JB, Polytrauma with thoracic and/or abdominal injuries: Experience in 1540 cases: Chin J Traumatol, 2006; 9(2); 108-14
26. Nishiumi N, Inokuchi S, Oiwa K, Diagnosis and treatment of pulmonary laceration with intrathoracic hemorrhage from blunt trauma: Ann Thorac Surg, 2010; 89(1); 232-38
Figures
Tables
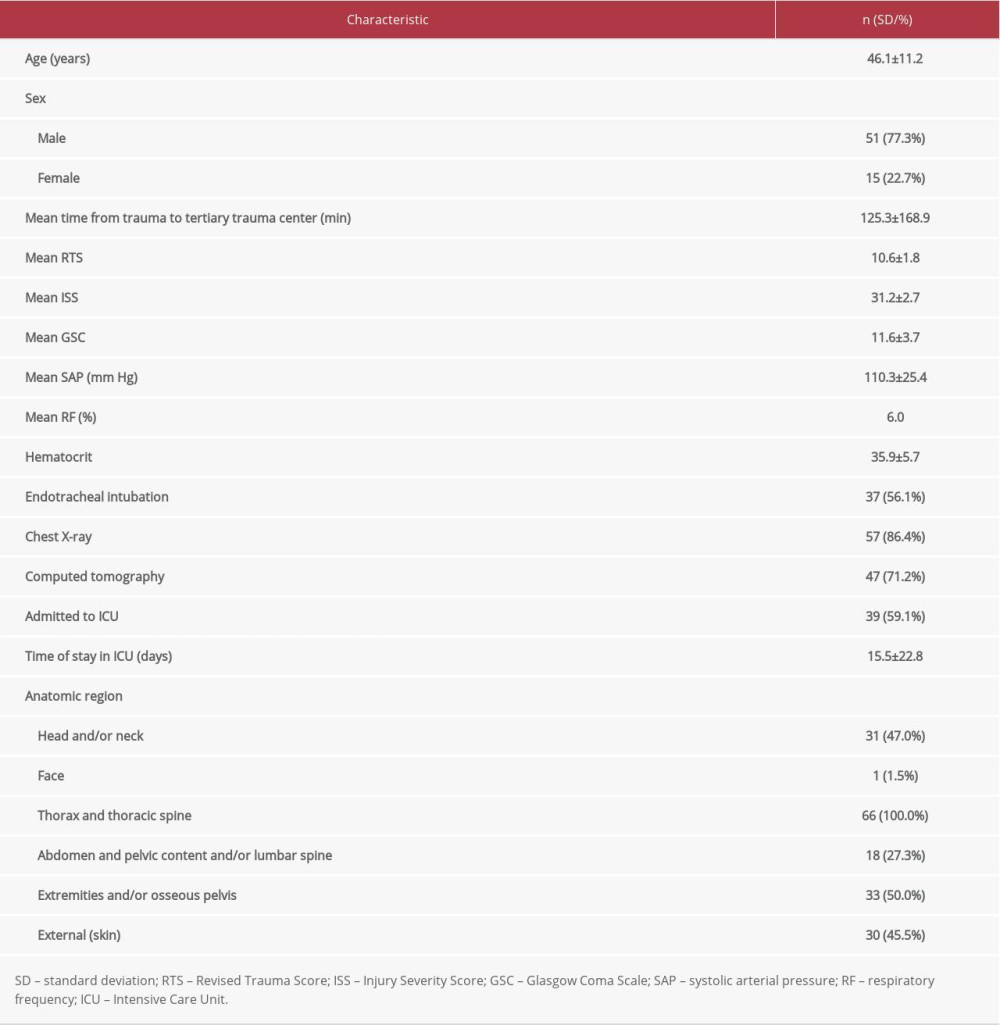 Table 1. Basic characteristics of patients at admission with anatomical regions of injuries.
Table 1. Basic characteristics of patients at admission with anatomical regions of injuries. Table 2. Prehospital time by 4 Revised Trauma Score groups.
Table 2. Prehospital time by 4 Revised Trauma Score groups.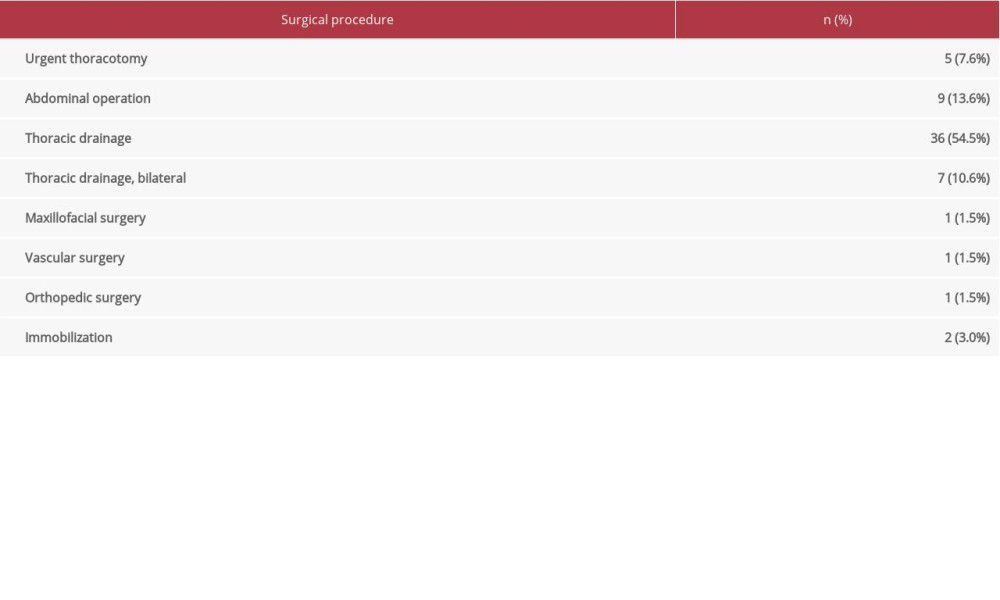 Table 3. Surgical procedures conducted in patients with polytrauma.
Table 3. Surgical procedures conducted in patients with polytrauma. Table 4. Relationship between Revised Trauma Score at admission and epicrisis.
Table 4. Relationship between Revised Trauma Score at admission and epicrisis.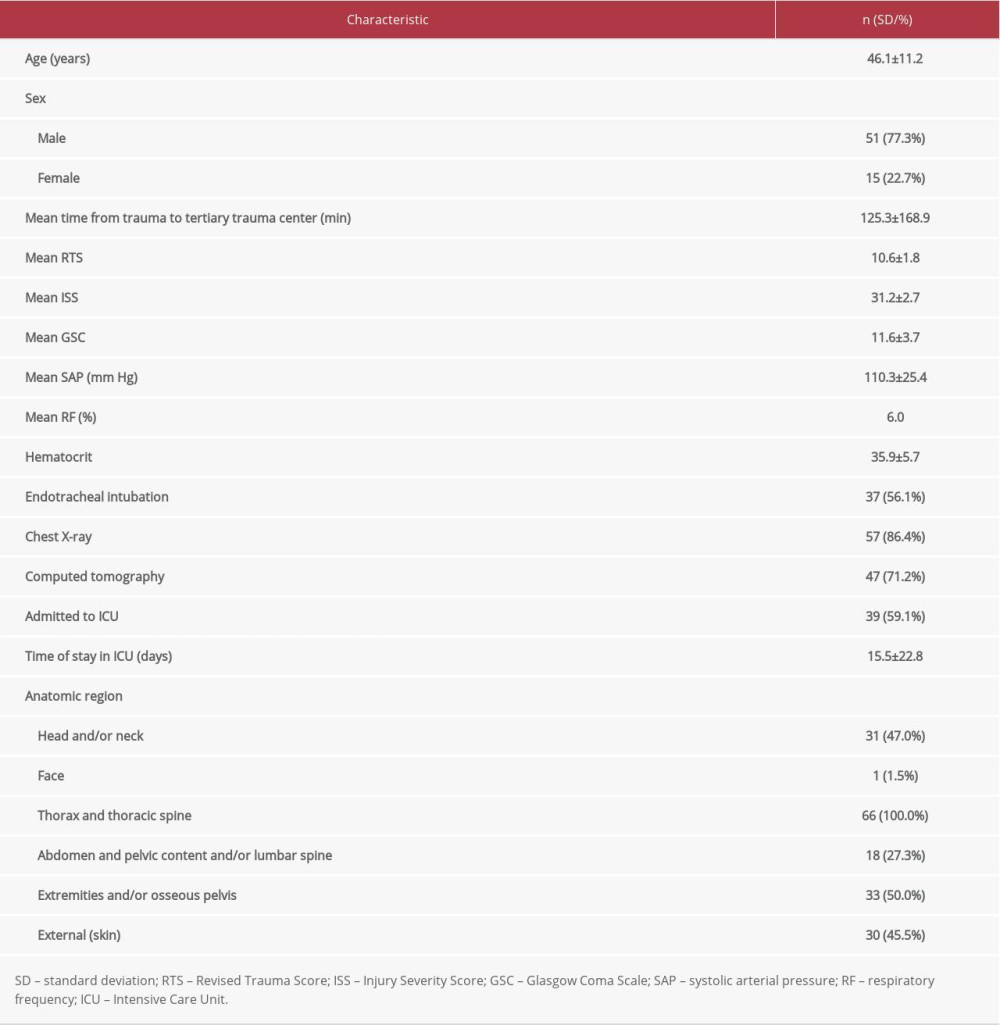 Table 1. Basic characteristics of patients at admission with anatomical regions of injuries.
Table 1. Basic characteristics of patients at admission with anatomical regions of injuries. Table 2. Prehospital time by 4 Revised Trauma Score groups.
Table 2. Prehospital time by 4 Revised Trauma Score groups.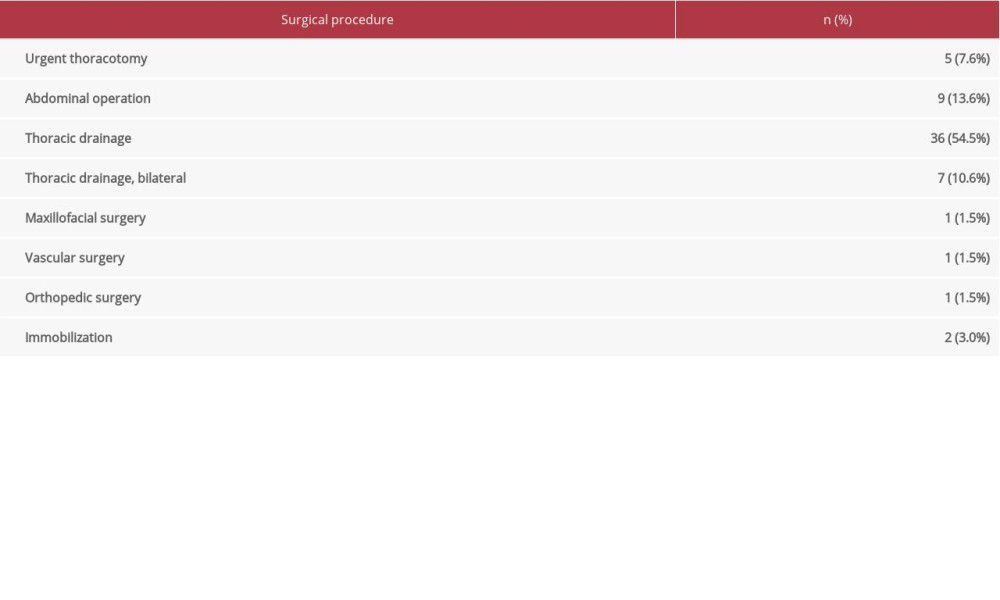 Table 3. Surgical procedures conducted in patients with polytrauma.
Table 3. Surgical procedures conducted in patients with polytrauma. Table 4. Relationship between Revised Trauma Score at admission and epicrisis.
Table 4. Relationship between Revised Trauma Score at admission and epicrisis. Most Viewed Current Articles
15 Jun 2022 : Clinical Research
Evaluation of Apical Leakage After Root Canal Obturation with Glass Ionomer, Resin, and Zinc Oxide Eugenol ...DOI :10.12659/MSMBR.936675
Med Sci Monit Basic Res 2022; 28:e936675
07 Jul 2022 : Laboratory Research
Cytotoxicity, Apoptosis, Migration Inhibition, and Autophagy-Induced by Crude Ricin from Ricinus communis S...DOI :10.12659/MSMBR.936683
Med Sci Monit Basic Res 2022; 28:e936683
01 Jun 2022 : Laboratory Research
Comparison of Sealing Abilities Among Zinc Oxide Eugenol Root-Canal Filling Cement, Antibacterial Biocerami...DOI :10.12659/MSMBR.936319
Med Sci Monit Basic Res 2022; 28:e936319
08 Dec 2022 : Original article
Use of Estimated Glomerular Filtration Rate and Urine Albumin-to-Creatinine Ratio Based on KDIGO 2012 Guide...DOI :10.12659/MSMBR.938176
Med Sci Monit Basic Res 2022; 28:e938176