13 September 2021: Human Study
Size of Acute Myocardial Infarction Correlates with Earlier Time of Initiation of Reperfusion Therapy with Cardiac Perfusion Scintigraphy: A National Single-Center Study
Hajdin Çitaku1ABCDF, Ramë Miftari23ACDEF*, David Stubljar4ACDF, Xhevdet Krasniqi56ADEDOI: 10.12659/MSMBR.933214
Med Sci Monit Basic Res 2021; 27:e933214
Abstract
BACKGROUND: BACKGROUND The aim of this study was to determine the correlation between the size of acute myocardial infarction (AMI) and the time of initiation of reperfusion therapy with cardiac perfusion scintigraphy. MATERIAL AND METHODS Overall, 80 patients with acute ST elevation myocardial infarction (STEMI) were examined. All patients were treated with primary percutaneous coronary intervention (pPCI). Data on patient and system delay expressed in minutes were recorded and compared with recommended timelines. Cardiac scintigraphy was performed with 99m Tc-sestamibi single-photon emission computed tomography (SPECT). The median time of cardiac scintigraphy was 20 days. The correlation between the size of infarction and the time of initiation of reperfusion therapy was evaluated. RESULTS The mean age of patients was 60.5±11.5 years, and 72.5% were male. The average system delay was 348 min, and the average patient delay was 173 min. The mean total ischemic time was 800 min. There was a correlation between time delays of reperfusion therapy and infarct size. Patients with a shorter time delay to patent artery after FMC showed smaller infarct size when compared to the patients with longer delay times. Multiple linear regression analysis showed that FMC, being male, and smokers had statistical significance when predicting infarct size. CONCLUSIONS There is a correlation between the size of myocardial infarction and the time of initiation of reperfusion therapy determined by perfusion myocardial scintigraphy. The study showed that there are time delays in starting the treatment of AMI with pPCI when compared to the recommended time, which requires an action plan in the near future to ensure earlier treatment for our patients.
MATERIAL AND METHODS:
RESULTS:
CONCLUSIONS:
Keywords: Angioplasty, Anterior Wall Myocardial Infarction, Technetium Tc 99m Sestamibi, Time Factors, Aged, Female, Heart, Humans, Male, Middle Aged, Myocardial Infarction, Myocardial Reperfusion, percutaneous coronary intervention, perfusion imaging, Tomography, Emission-Computed, Single-Photon
Background
Treatment of patients with ST elevation myocardial infarction (STEMI) consists of reperfusion therapy with the aim to restore blood circulation into the ischemic myocardium. The benefits of angioplasty are maximal when the procedure is performed within 2 h after the onset of symptoms, resulting in reduced mortality, heart failure, and rehospitalizations [1]. When primary percutaneous coronary intervention (pPCI) is performed between 3 and 6 h after the onset of symptoms the patient can still benefit, but to a lesser degree. A large number of observational studies have confirmed that any delay of at least 30 min in treatment resulted in a 7.5% per year increase of the risk of mortality in patients with myocardial infarction [2]. Thus, earlier time to reperfusion therapy is crucial. Additional risk factors leading to worse outcomes of AMI include comorbid diabetes, hypertension, peripheral artery disease, older age, reduced renal function, and history of stroke [3]. Infarct size and microvascular obstruction (MVO) are the main independent predictors of long-term mortality and heart failure in STEMI survivors [4,5]. MVO is defined as insufficient myocardial perfusion after successful mechanical opening of the infarct related artery (IRA), and is caused by various factors [6].
Use of single-photon emission computed tomography (SPECT) and cardiac magnetic resonance (CMR) for determination of myocardial infarct size is relatively new and may be useful for post-discharge risk stratification [7]. The purpose of this study was to assess delays and their impact on infarct size, as the data for our country are lacking, and thus assess a possible correlation between the size of AMI and the time of initiation of reperfusion therapy with cardiac perfusion scintigraphy. The Republic of Kosovo is part of the Western Balkan, South-East Europe region and has 1.78 million inhabitants [8]. Currently only 1 center, the University Clinical Center of Kosovo (UCCK), offers services for treatment of AMI with pPCI 24 h per day, 7 days per week. In early 2018, the start of 24-hour service at the Unit of Invasive Cardiology enabled treatment with pPCI for AMI. However, there is no functioning health insurance system or fully operational health information system, nor is there a database for tracking treatment delays, so this study is the first attempt at gathering national data.
Material and Methods
STATISTICAL ANALYSES:
All statistical analyses were performed using SPSS Statistics 21 (IBM, New York, USA). For categorical data, correlation between groups was assessed with the Pearson’s chi-square test or Fisher exact test; fore continuous data, the differences were assessed by analysis of variance or the Kruskal-Wallis test for data with non-normal distribution. Continuous variables were presented as mean or median values. Time delay was defined as the time from the onset of symptoms to the FMC; it was considered as a continuous variable and was expressed in minutes. Patient delays were log-transformed for further analysis. The effect of each potential predictor for infarct size was assessed by multiple linear regression analysis. All analyses were performed at a level of 5% significance.
Results
The study included a total of 80 patients with AMI who underwent primary percutaneous coronary intervention (pPCI). Data on basic patient characteristics are presented in Table 1. Coronary angiography findings showed involvement of the left anterior descending artery (LAD) in 42 (52.5%) patients, right coronary artery (RCA) in 23 (28.9%), and circumflex artery (LCX) in 15 (18.8%). Regarding the number of arteries, 40% of patients had single-vessel coronary heart disease, 31% had 2-vessel coronary artery disease, and 29% had 3-vessel coronary artery disease.
The average system delay was 348 min. The average patient delay was 173 min (range 45–180 min). The door-to-balloon inflation time was 114 min (0–65 min). The average distance to the regional hospital was 50 km, which resulted in an average delay of 950 min.
Patients were divided into 2 groups according to the timing of reperfusion therapy: the first group received reperfusion therapy within the first 180 min (3 h), and the second group after 180 min (more than 3 h). Patients with a different patent artery after FMC showed no significant differences between the 2 groups except for the FMC to patent artery (Table 2).
Our research did not differentiate the patients according to diabetes status, although this has been identified as a risk factor. We also did not compare mortality between the 2 PCI groups, as this was not the primary nor secondary endpoint of the study, but we rather focused on the size of infarction, which has been correlated in the past with higher mortality rates.
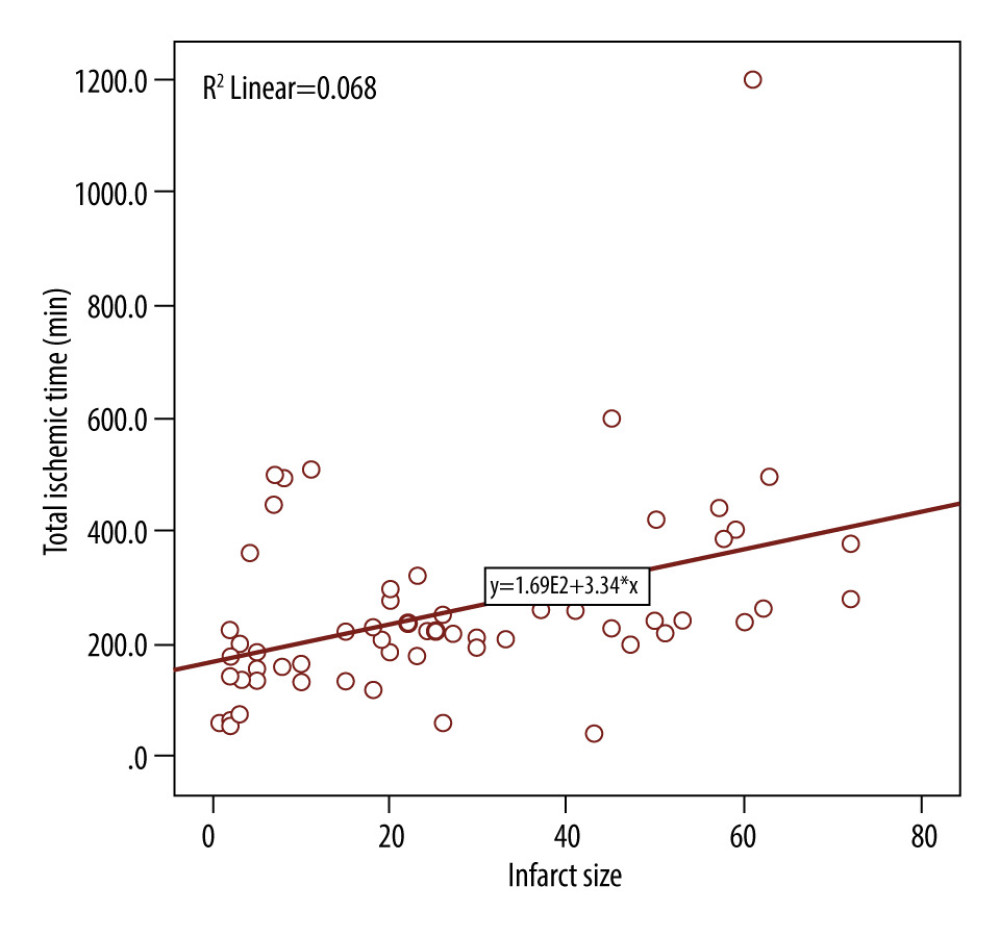
There was a good correlation between time delays of reperfusion therapy and infarct size, as shown in the Figure 1, with r=0.36. Patients with a shorter time of patent artery after FMC had smaller infarct size compared to patients with longer delay times. Moreover, multiple linear regression analysis showed that FMC, being male, and being a smoker were statistically significant (
Discussion
STUDY LIMITATIONS:
Our analysis has some limitations. The data were analyzed retrospectively, impacting the quality of the dataset. Measurements of time delays could be biased and thus result in errors. Only patients who had full records were included, resulting in a relatively small sample size. A larger-scale study might have found a stronger correlation between time delays and infarct size. Lastly, this was a single-center study with a small number of patients for the multiple timepoint measurements.
Conclusions
We found a significant relationship between the size of myocardial infarction and the time of initiation of reperfusion therapy as determined by perfusion myocardial scintigraphy. The study showed that there are long delays in starting the treatment of AMI with pPCI compared to the recommended timelines. Evidence-based studies show that infarct size will improve with earlier management of STEMI patients, by better identification of those with large infarcts. Our results suggest the need for an action plan to reduce time delays, as well as the need for improved management systems to significantly reduce delays in treatment of STEMI patients.
References
1. Ibanez B, James S, Agewall S, 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST segment elevation of the European Society of Cardiology (ESC): Eur Heart J, 2018; 39; 119-77
2. De Luca G, Suryapranata H, Ottervanger JP, Antman EM, Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts: Circulation, 2004; 109; 1223-25
3. Johansson S, Rosengren A, Young K, Jennings E, Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: A systematic review: BMC Cardiovasc Disord, 2017; 17; 53
4. Stone GW, Selker HP, Thiele H, Relationship between infarct size and outcomes following primary PCI: Patient-level analysis from 10 randomized trials: J Am Coll Cardiol, 2016; 67; 1674-83
5. Ibáñez B, Heusch G, Ovize M, Van de Werf F, Evolving therapies for myocardial ischemia/reperfusion injury: J Am Coll Cardiol, 2015; 65; 1454-71
6. Niccoli G, Scalone G, Lerman A, Crea F, Coronary microvascular obstruction in acute myocardial infarction: Eur Heart J, 2016; 37; 1024-33
7. Gibbons RJ, Araoz P, Does infarct size matter?: J Am Coll Cardiol, 2016; 67; 1684-86
8. Statistical Agency of Kosovo: Health System, Social Statistics, Health Statistics, Series 5, 2014, Prishtina, Kosovo
9. : The independent commission for mines and minerals Infrastructure Available from: www.kosovo-mining.org/kosovo/infrastructure/?lang=en
10. Reindl M, Holzknecht M, Tiller C, Impact of infarct location and size on clinical outcome after ST-elevation myocardial infarction treated by primary percutaneous coronary intervention: Int J Cardiol, 2020; 301; 14-20
11. Dohi T, Maehara A, Brener SJ, Utility of peak creatine kinase-MB measurements in predicting myocardial infarct size, left ventricular dysfunction, and outcome after first anterior wall acute myocardial infarction (from the INFUSE-AMI trial): Am J Cardiol, 2015; 115; 563-70
12. De Luca G, Suryapranata H, Zijlstra F, Symptom-onset-to-balloon time and mortality in patients with acute myocardial infarction treated by primary angioplasty: J Am Coll Cardiol, 2003; 42; 991-97
13. Rathore SS, Curtis JP, Chen J, Association of door-to-balloon time and mortality in patients admitted to hospital with ST elevation myocardial infarction: National cohort study: BMJ, 2009; 338; b1807
14. Brodie BR, Stuckey TD, Wall TC, Importance of time to reperfusion for 30-day and late survival and recovery of left ventricular function after primary angioplasty for acute myocardial infarction: J Am Coll Cardiol, 1998; 32; 1312-19
15. Tödt T, Maret E, Alfredsson J, Janzon M, Relationship between treatment delay and final infarct size in STEMI patients treated with abciximab and primary PCI: BMC Cardiovasc Disord, 2012; 12; 9
16. Kosmidou I, Redfors B, Selker HP, Infarct size, left ventricular function, and prognosis in women compared to men after primary percutaneous coronary intervention in ST-segment elevation myocardial infarction: Results from an individual patient-level pooled analysis of 10 randomized trials: Eur Heart J, 2017; 38; 1656-63
17. Sager HB, Husser O, Steffens S, Time-of-day at symptom onset was not associated with infarct size and long-term prognosis in patients with ST-segment elevation myocardial infarction: J Transl Med, 2019; 17; 180
18. Żurowska-Wolak M, Piekos P, Jąkała J, Mikos M, The effects of prehospital system delays on the treatment efficacy of STEMI patients: Scand J Trauma Resusc Emerg Med, 2019; 27; 39
19. Stone GW, Dixon SR, Grines CL, Predictors of infarct size after primary coronary angioplasty in acute myocardial infarction from pooled analysis from four contemporary trials: Am J Cardiol, 2007; 100; 1370-75
20. Hedström E, Engblom H, Frogner F, Infarct evolution in man studied in patients with first-time coronary occlusion in comparison to different species – implications for assessment of myocardial salvage: J Cardiovasc Magn Reson, 2009; 11; 38
21. Shahim B, Redfors B, Chen S, BMI, infarct size, and clinical outcomes following primary PCI: Patient-level analysis from 6 randomized trials: JACC Cardiovasc Interv, 2020; 13; 965-72
22. Patel MR, Worthley SG, Stebbins A, Pexelizumab and infarct size in patients with acute myocardial infarction undergoing primary percutaneous coronary intervention: A delayed enhancement cardiac magnetic resonance substudy from the APEX-AMI trial: JACC Cardiovasc Imaging, 2010; 3; 52-60
23. Wu E, Ortiz JT, Tejedor P, Infarct size by contrast enhanced cardiac magnetic resonance is a stronger predictor of outcomes than left ventricular ejection fraction or end-systolic volume index: Prospective cohort study: Heart, 2008; 94; 730-36
24. Chen S, Redfors B, Crowley A, Relationship between primary percutaneous coronary intervention time of day, infarct size, microvascular obstruction and prognosis in ST-segment elevation myocardial infarction: Coron Artery Dis, 2021; 32; 267-74
25. Bradley EH, Curry LA, Webster TR, Achieving rapid door-to-balloon times: How top hospitals improve complex clinical systems: Circulation, 2006; 113; 1079-85
26. Ward MR, Lo ST, Herity NA, Effect of audit on door-to-inflation times in primary angioplasty/stenting for acute myocardial infarction: Am J Cardiol, 2001; 87; 336-38
27. Shry EA, Eckart RE, Winslow JB, Effect of monitoring of physician performance on door-to-balloon time for primary angioplasty in acute myocardial infarction: Am J Cardiol, 2003; 91; 867-69
Tables
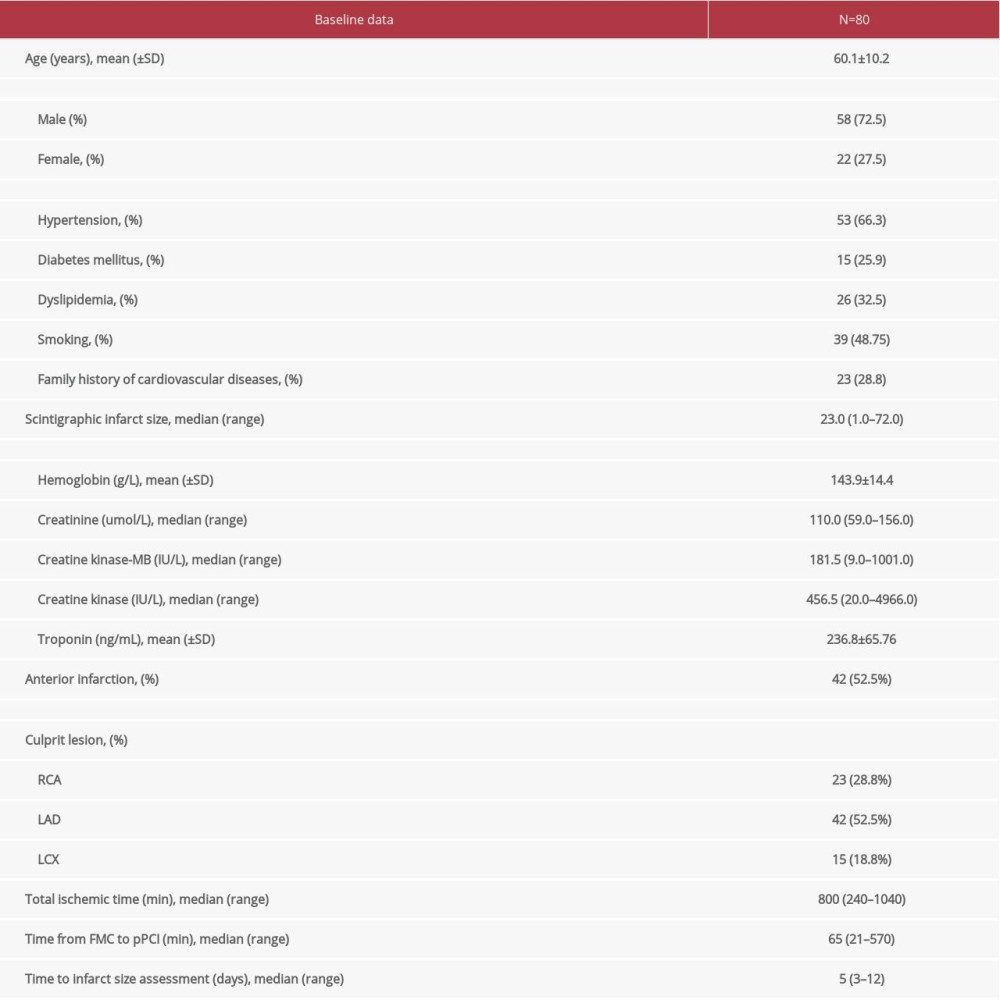 Table 1. Basic characteristics of patients at admission.
Table 1. Basic characteristics of patients at admission. Table 2. Characteristics related to reperfusion time.
Table 2. Characteristics related to reperfusion time.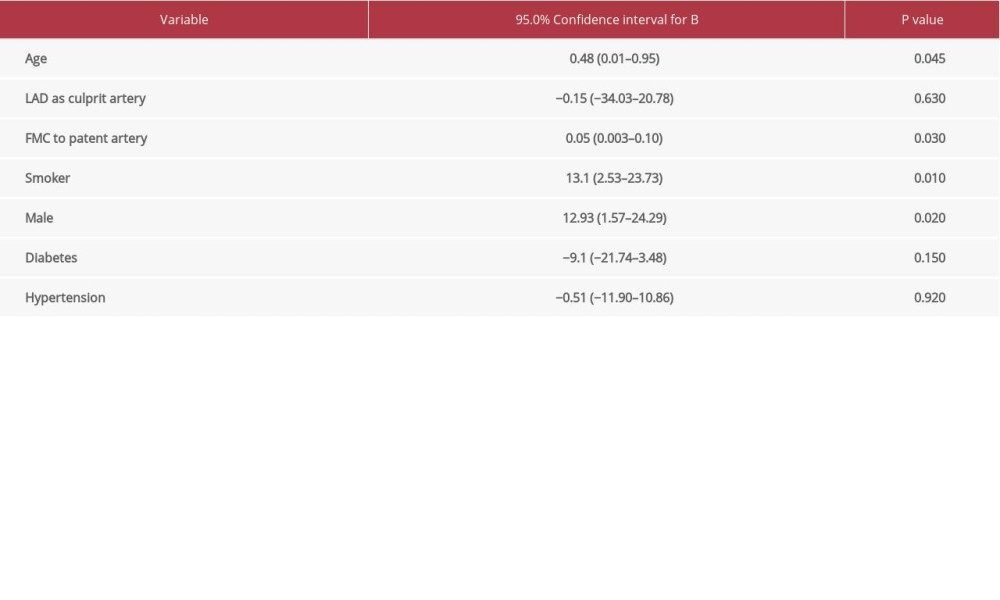 Table 3. Prediction of infarct size (dependent variable) based on multiple linear regression.
Table 3. Prediction of infarct size (dependent variable) based on multiple linear regression.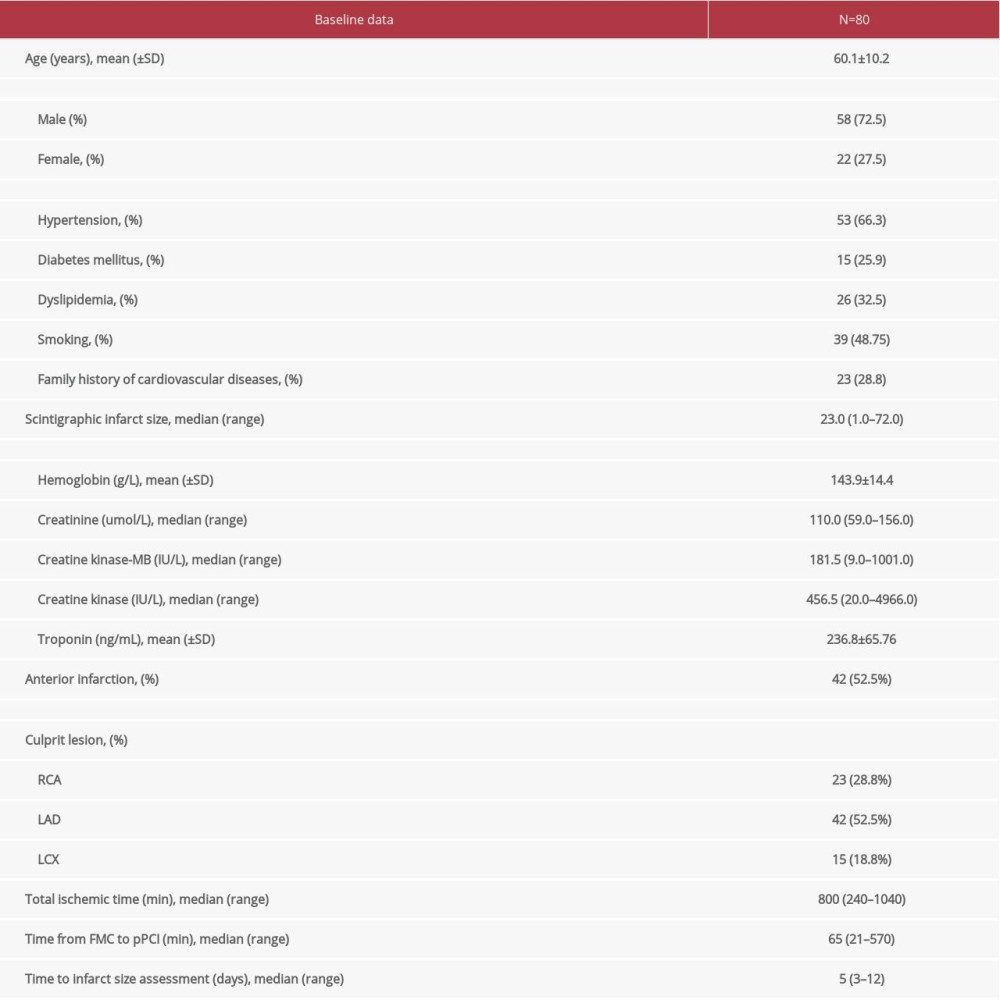 Table 1. Basic characteristics of patients at admission.
Table 1. Basic characteristics of patients at admission. Table 2. Characteristics related to reperfusion time.
Table 2. Characteristics related to reperfusion time.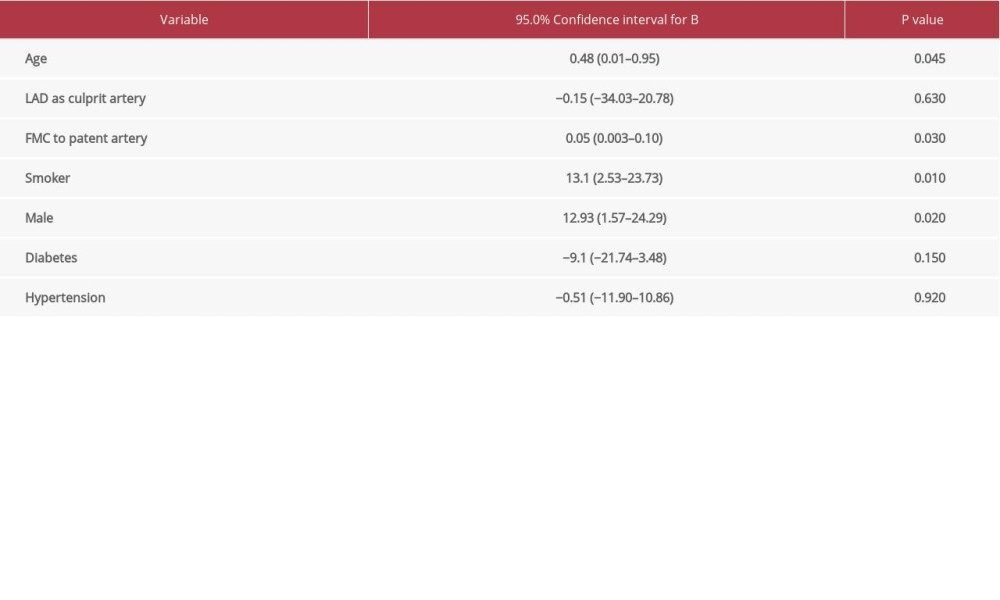 Table 3. Prediction of infarct size (dependent variable) based on multiple linear regression.
Table 3. Prediction of infarct size (dependent variable) based on multiple linear regression. Most Viewed Current Articles
15 Jun 2022 : Clinical Research
Evaluation of Apical Leakage After Root Canal Obturation with Glass Ionomer, Resin, and Zinc Oxide Eugenol ...DOI :10.12659/MSMBR.936675
Med Sci Monit Basic Res 2022; 28:e936675
07 Jul 2022 : Laboratory Research
Cytotoxicity, Apoptosis, Migration Inhibition, and Autophagy-Induced by Crude Ricin from Ricinus communis S...DOI :10.12659/MSMBR.936683
Med Sci Monit Basic Res 2022; 28:e936683
01 Jun 2022 : Laboratory Research
Comparison of Sealing Abilities Among Zinc Oxide Eugenol Root-Canal Filling Cement, Antibacterial Biocerami...DOI :10.12659/MSMBR.936319
Med Sci Monit Basic Res 2022; 28:e936319
08 Dec 2022 : Original article
Use of Estimated Glomerular Filtration Rate and Urine Albumin-to-Creatinine Ratio Based on KDIGO 2012 Guide...DOI :10.12659/MSMBR.938176
Med Sci Monit Basic Res 2022; 28:e938176