05 September 2020: Clinical Research
A Diagnostic Model to Improve the Predictability of Natural Pregnancy Potential in Patients with Oligoasthenospermia
Tiancheng Zhang1CE, Xin Wang2D, Zhikai Wang2F, Zhiming Xu2F, Liang Chen2F, Maohua Miao3F, Bin Wu1D, Xuemei Wang1D, Xiaorong Shen1D, Jun Wu1B, Ke Wang1B, Huijuan Shi1B, Jianhui Li2AE*, Jufen Zheng1AGDOI: 10.12659/MSM.922316
Med Sci Monit 2020; 26:e922316
Abstract
BACKGROUND: Oligoasthenospermia is one of the major reasons for male infertility in clinical practice. Nevertheless, some patients with oligoasthenospermia show normal fertility. Currently, there is a lack of an effective method to distinguish patients with oligoasthenospermia showing normal fertility from those who lack natural fertility and should participate in in vitro fertilization and assisted reproduction.
MATERIAL AND METHODS: In this study, we collected semen and blood samples from 153 males of Shui nationality at reproductive age in Guizhou Province, southwest China. We measured the routine parameters for semen and some serological indicators. A clinical diagnosis model was then constructed to evaluate the fertility potential of oligoasthenospermia patients using a logistic stepwise regression method, which was then visualized with a nomogram.
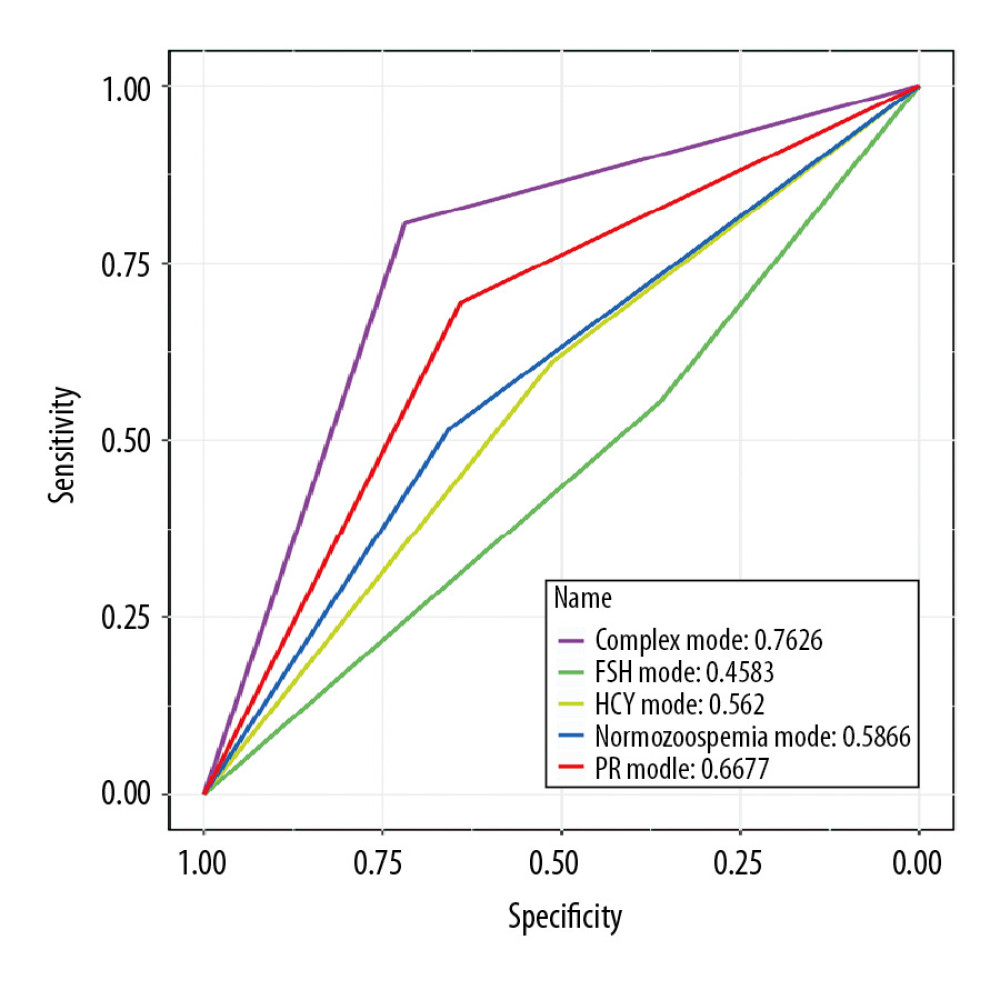
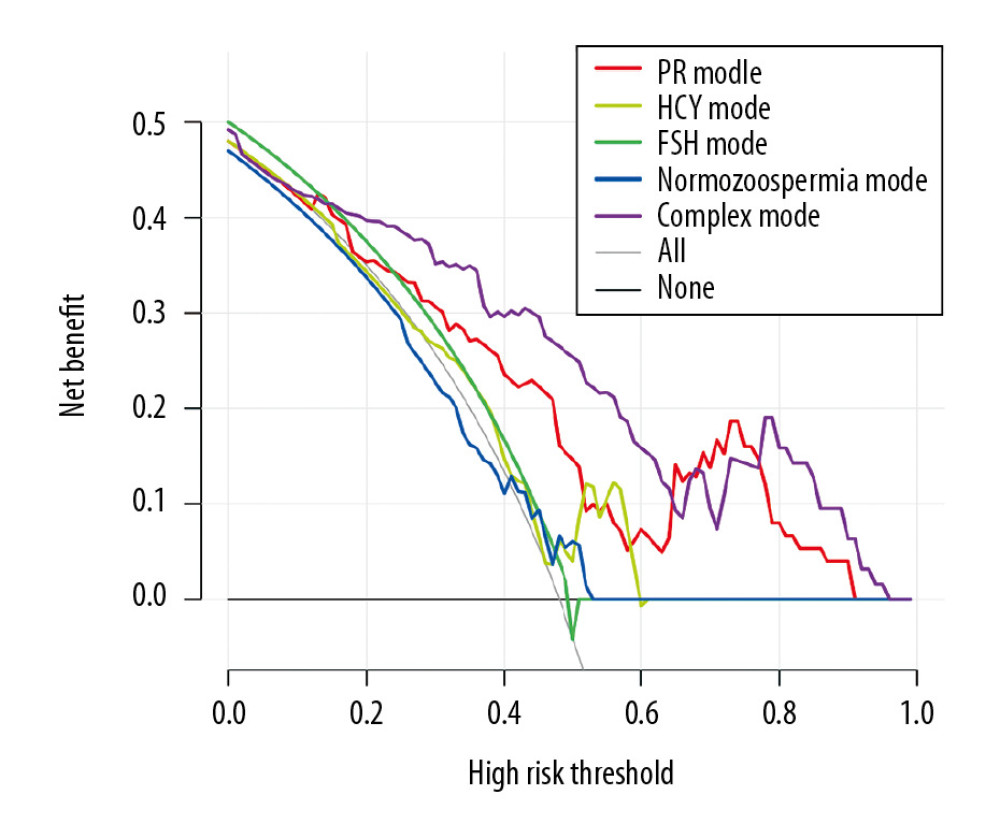
RESULTS: Our results showed that this model could effectively assess the natural pregnancy potential of patients with oligoasthenospermia, and its sensitivity and specificity were superior to those of a traditional model that used only sperm motility and count to assess male fertility potential (area under the curve=0.7626 vs. 0.6677). Additionally, we evaluated the clinical net benefit for patients with oligoasthenospermia at different risk scores in our model using decision curve analysis. The results showed that the net benefit was obtained at scores ranging from 0.1 to 0.6.
CONCLUSIONS: This comprehensive clinical prediction model can be used to determine whether infertile oligoasthenospermia patients lack natural fertility.
Keywords: Diagnosis, Oligospermia, Pregnancy, Adolescent, Cross-Sectional Studies, Fertility, Follicle Stimulating Hormone, homocysteine, Luteinizing Hormone, nomograms, young adult
Background
Idiopathic oligoasthenospermia is one of the main influencing factors of male infertility, but its mechanism is currently unclear [1]. At present, only sperm motility, count, and morphology are used clinically to diagnose male fertility [2]. Despite the difficulties, some oligoasthenospermia patients do have the opportunity to achieve natural pregnancy; thus, it is not necessary for these patients to participate in
Material and Methods
PATIENTS AND ETHICS:
During the period from November 2011 to July 2012, we adopted an overall random sampling method to conduct a cross-sectional survey of all 18–55-year-old, married, and reproductive-age men in the Shui nationality area of Guizhou Province. After excluding individuals who did not desire to have children, had azoospermia, or had organic diseases such as cryptorchidism, varicocele, vas deferens disorders, and small testicles, 157 subjects were included in the analysis. Among them, men with normal sperm and normal fertility were included in the control group, men with oligoasthenospermia but having had offspring were included in the fertile oligoasthenospermia group, and men with oligoasthenospermia and no pregnancy success for more than 5 years were included in the infertile oligoasthenospermia group.
The study was approved by the Ethics Committee and Institutional Review Board of Shanghai Institute of Planned Parenthood Research. Consent was obtained from each participant after receiving a full explanation of the purpose and nature of all procedures used. The standards for collecting semen were as follows: subjects were asked to abstain from sex as much as possible for a maximum of 3–5 days; subjects were required to abstain from alcohol 4 days before collection; semen collection from infertile patients and the control group should be done at the same time and in the same season as often as possible; subjects should urinate and wash their hands and penis before semen collection. For blood collection, room temperature was maintained at 22–25°C, and the blood was collected from the same batch of research subjects at the same time. It was then stored in an anticoagulant tube, first in a 4°C refrigerator, then stored at −20°C for 8 h followed by −80°C for 2 weeks. The age range for blood collection was 20–50 years old, with an average age of 33 years.
DETERMINATION OF SERUM REPRODUCTIVE HORMONE AND HCY:
Five milliliters of venous blood was collected, and then the serum was separated and stored at −20°C. Serum samples were measured by chemiluminescence. The indicators detected included follicle stimulating hormone (FSH), luteinizing hormone (LH), testosterone (T), and HCY.
DETERMINATION OF SPERM QUALITY:
Semen samples were obtained by masturbation. Semen volume, pH value, density, sperm motility, and forward movement rate were determined using a WLJY-9000 automated color-sperm quality detection system according to the standards of the World Health Organization
STATISTICAL ANALYSIS:
Comparisons of parameters between patients and controls were assessed using the Wilcoxon test and Kruskal-Wallis test for continuous variables. The chi-square test was used for categorical variables.
A multivariable logistic regression model was generated with variable selection by backward elimination. For each patient, a total score was calculated, and then the outcome probability of each patient was calculated with a conversion function between the score and the outcome probability. The receiver operating characteristic (ROC) curve is recognized as a standard evaluation index. The area under the curve (AUC), with false positive rate as the abscissa and true positive rate as the ordinate, indicates the accuracy of the diagnostic test. The decision curve is a curve with threshold probability as the abscissa and net benefit as the ordinate. When the different evaluation methods reach a certain value, the positive probability of patient i is recorded as Pi; when Pi reaches a certain threshold (recorded as Pt), it is defined as positive, and some intervention should be taken [4,5].
All statistical analyses were performed using the R programming language.
PATIENTS AND PUBLIC INVOLVEMENT:
Patients and the public were not involved in any aspect of this study.
Results
PATIENT CHARACTERISTICS:
The patient characteristics are summarized in Table 1. Samples from 157 subjects were analyzed, of whom 82 had normal fertility, 36 had fertile oligoasthenospermia, and 39 had infertile oligoasthenospermia. The variables studied included HCY, progressive motility (PR, %), PR + nonprogressive motility (%), density (106/mL), age, FSH, LH, T, percentage of normal sperm, percentage of malformed sperm, and percentage of round cells. Our results showed that there were no significant differences between the ages of patients with fertile and infertile oligoasthenospermia, and the levels of the three major hormones were FSH, 3.25–8.004; LH, 3.393–7.385; and T, 4.462–6.963.
MULTIVARIABLE REGRESSION ANALYSIS AND PROGNOSTIC MODEL CONSTRUCTION:
In this study, we established a predictive model to improve the accuracy for the current prognostic method using logistic regression. Then, we generated a predictive model to evaluate the fertility potential for patients with oligoasthenospermia by combining HCY, PR, and FSH with normozoospermia frequency, using a P value for the correlation coefficient <0.15 as the cutoff value (Table 2).
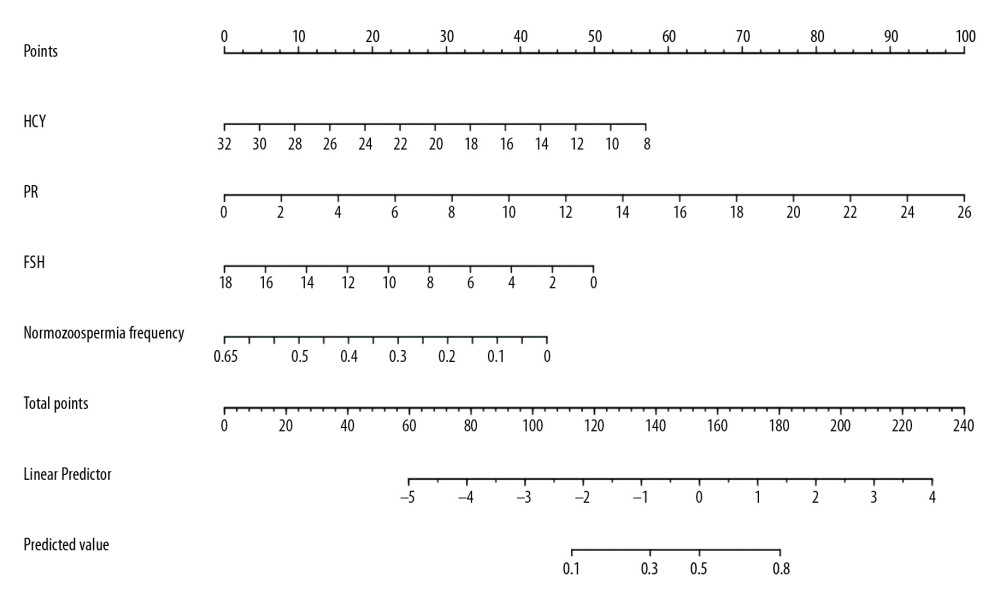
The point assignment of the nomogram for the probability of natural pregnancy for patients with oligoasthenospermia is shown in Figure 1. By adding up all points and locating them on the bottom scales, we can easily calculate the estimated probability of natural pregnancy for patients with oligoasthenospermia. When the corresponding variables for the diagnosed patients are substituted into the model, scores greater than 50% are recorded as infertile oligoasthenospermia, whereas those less than 50% are recorded as fertile oligoasthenospermia.
EFFICACY OF THE DIAGNOSTIC MODEL:
The nomogram showed valuable predictive power, with an AUC of 0.7626, sensitivity of 0.7188, and specificity of 0.8065 (Table 3). The area under the ROC curve was not affected by the prevalence and diagnostic critical value and thus can be used to comprehensively compare the accuracy of two diagnostic tests. In this study, we compared the accuracy of our multifactor model with that of one-factor predictive models. The individual PR predictive indicator showed an AUC of 0.6677, whereas the individual sperm motility assessment model only showed an AUC of 0.5866 (Figure 2), which indicated that the comprehensive evaluation model was more accurate than the single-indicator evaluation models.
By inspecting the decision curve analysis plot shown in Figure 3, it is possible to find a clear net benefit gain over the entire range of thresholds when using the updated prognostic model compared with the baseline model or considering all patients (or no patients) at risk of infertile oligoasthenospermia.
Discussion
Oligoasthenospermia refers to the situation where the total number (or density) of spermatozoa and the percentage of forward-moving spermatozoa found during routine sperm testing are lower than the reference minimum values. Studies have shown that patients with this symptom generally show low fertility. A study by Li et al. collected 16 835 semen samples and revealed that oligoasthenospermia is related to infertility [6]. Liu et al. analysed the semen quality of 2810 infertile men in the Huzhou area of China and showed that oligoasthenospermia is one of the main factors of male infertility in this area [7].
At present, the treatment options for oligoasthenospermia mainly include drug treatment and assisted reproductive technology. The main purpose of drug treatment is to improve the quality of sperm and help patients conceive naturally. For instance, tamoxifen, coenzyme Q10, and traditional Chinese medicine qilin have all shown good clinical effects [8–10], improving the sperm quality of patients with oligoasthenospermia and helping them conceive naturally. However, it is difficult to determine which type of patient’s sperm has the potential for improved quality by testing only sperm density and movement.
In this study, we found that, combined with sperm count, sperm motility, and other indicators, some routine items for clinical prognosis such as HCY and FSH could be used to construct a more accurate and effective predictive model that could effectively distinguish oligoasthenospermia patients who were able to conceive spontaneously from those who were unable to achieve natural pregnancy. Interestingly, when recruiting patients, we did not strictly limit the age of the respondents. Therefore, we considered age as one of the potential elements in fertility when modeling. A correlation was found between age and reproductive capacity of oligoasthenospermia patients; however, this correlation was lost in the process of constructing the model by regression analysis.
The model may help clinicians discriminate patients who should continue trying to conceive naturally from those who need assisted reproductive intervention. The strengths of our study include its randomized design and reasonable statistical methods. The study also has weaknesses that should be acknowledged. One of the weaknesses is the relatively small sample size, which may be due to our restrictive selection conditions. Another notable issue is that the study participants were limited to the Chinese Shui population, which restricted the generalizability of our findings. Therefore, further large-scale longitudinal cohort studies in multiracial and multiethnic populations are still needed. Furthermore, we attempted to control for confounding factors as much as possible but were unable to do so completely. For example, although we excluded the possible effects of alcohol and sample handling when recruiting patients, we did not consider environmental exposure factors such as potential infections, occupational factors, and heavy-metal pollution. These omissions could bias our results.
Conclusions
We used clinically routinely tested HCY, PR, FSH, and normal sperm count indicators to construct a comprehensive predictive model for infertile oligoasthenospermia. This model is superior to those built from single predictors, including sperm motility, the most commonly used clinical method of judging male fertility for distinguishing patients with fertility and infertility. However, because of the small sample size of this study, further large-scale multicenter studies are needed to obtain a more accurate evaluation model for clinical practice that would be of benefit for oligoasthenospermia patients.
References
1. Nordhoff V, Fricke RK, Schuring AN, Treatment strategies for severe oligoasthenoteratozoospermia (OAT) (<0.1 million/mL) patients: Andrology, 2015; 3(5); 856-63
2. Colpi GM, Francavilla S, Haidl G, European Academy of Andrology guideline: Management of oligo-astheno-teratozoospermia: Andrology, 2018; 6(4); 513-24
3. Ortega C, Verheyen G, Raick D, Absolute asthenozoospermia and ICSI: What are the options?: Hum Reprod Update, 2011; 17(5); 684-92
4. Vickers AJ, Elkin EB, Decision curve analysis: A novel method for evaluating prediction models: Med Decis Making, 2006; 26(6); 565-74
5. Vickers AJ, van Calster B, Steyerberg EW, A simple, step-by-step guide to interpreting decision curve analysis: Diagn Progn Res, 2019; 3; 1
6. Li W, Zhu W, Tang Z, Liu GSemen quality of 16 835 infertile men in China: Zhong Nan Da Xue Xue Bao Yi Xue Ban, 2014; 39(2); 157-60 [in Chinese]
7. Liu C, Qiu H, Wu X, Investigation on sperm quality of 2810 males: Infertility in Huzhou City in 2010: Chin J Health Lab Technol, 2011; 21(8); 1998-2002
8. Tang KF, Xing Y, Wu CYTamoxifen combined with coenzyme Q10 for idiopathic oligoasthenospermia: Zhong Nan Ke Xue, 2011; 17(7); 615-18 [in Chinese]
9. Guo L, Jing J, Feng YM, Yao B, Tamoxifen is a potent antioxidant modulator for sperm quality in patients with idiopathic oligoasthenospermia: Int Urol Nephrol, 2015; 47(9); 1463-69
10. Jin X, Man C, Gong D, Fan Y, Adjuvant treatment with oilin pill for men with oligoasthenospermia: A meta-Analysis of randomized controlled trials: Phytother Res, 2017; 31(9); 1291-97
Figures
Tables
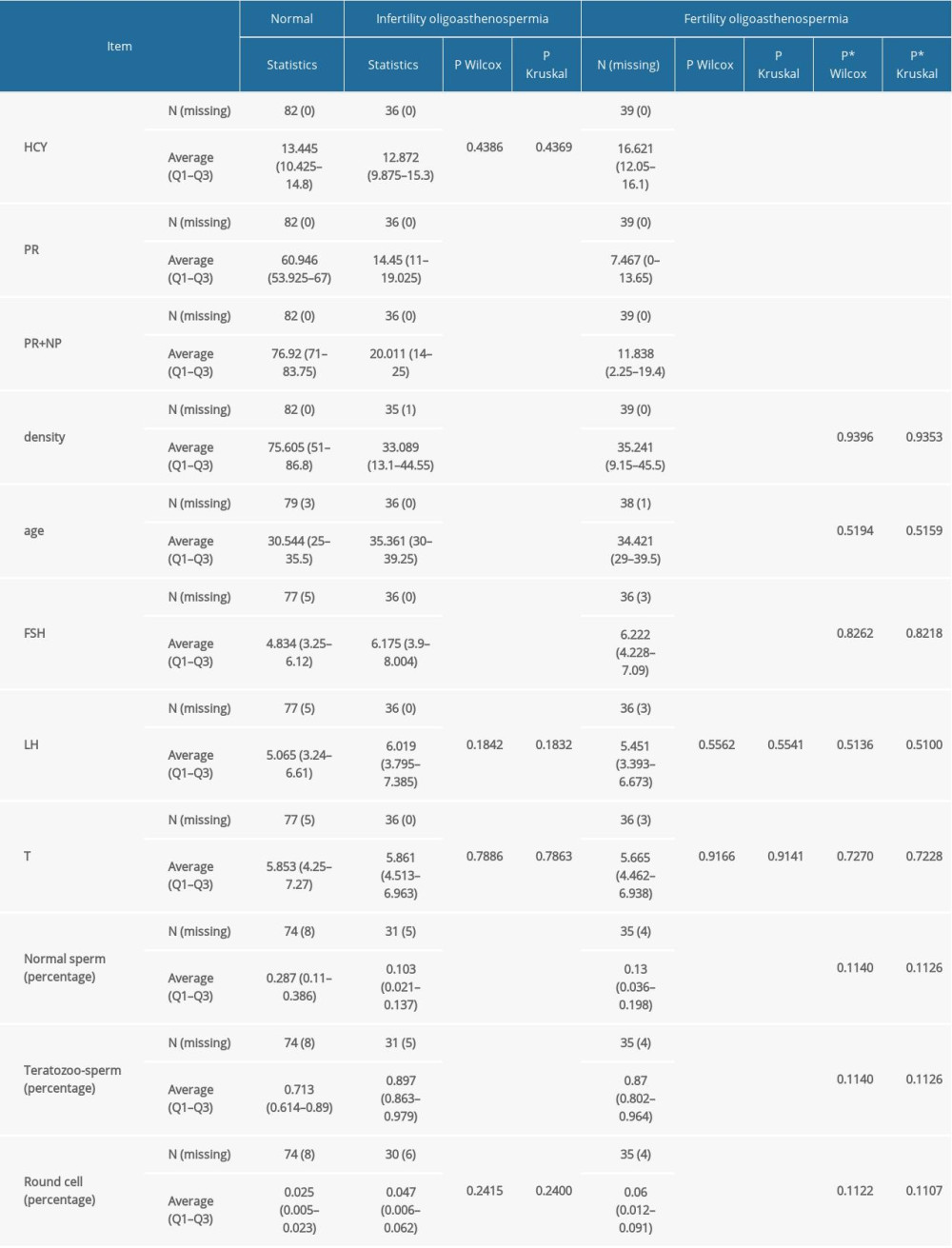 Table 1. Characteristics of normal fertility men and oligoasthenospermia.
Table 1. Characteristics of normal fertility men and oligoasthenospermia.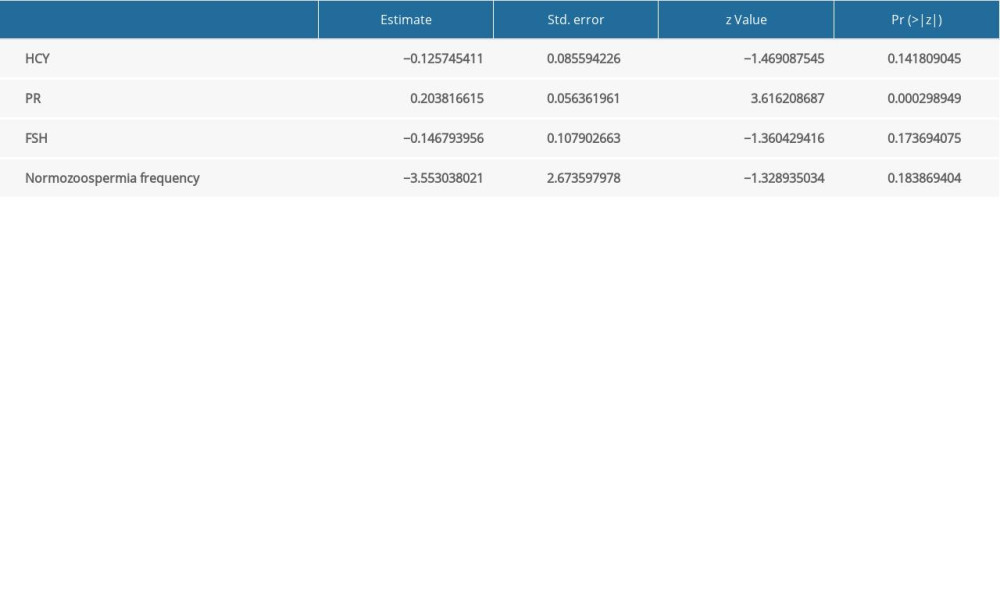 Table 2. Multivariable logistic regression model for successful natural conception.
Table 2. Multivariable logistic regression model for successful natural conception. Table 3. Prediction properties of based on internal validation.
Table 3. Prediction properties of based on internal validation.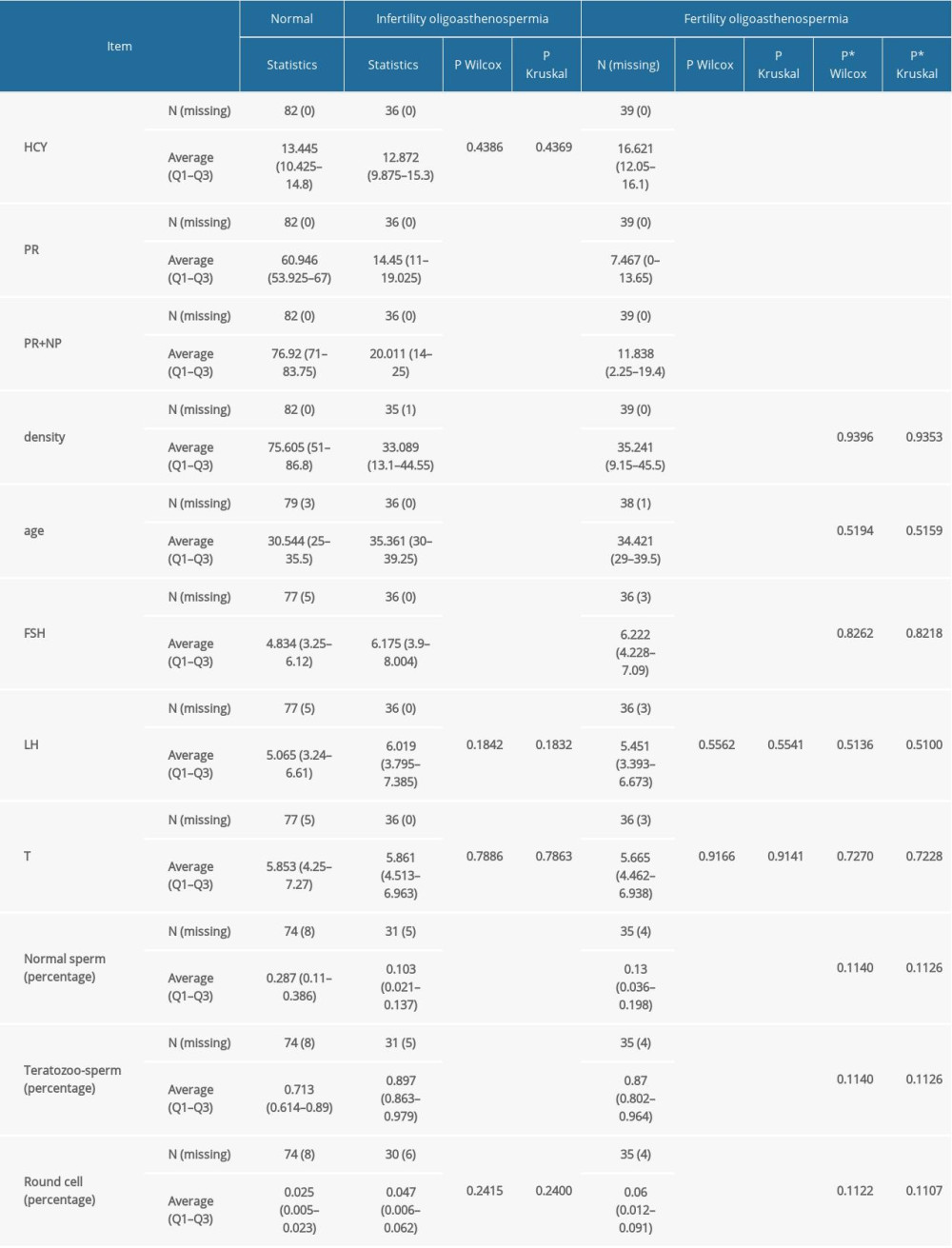 Table 1. Characteristics of normal fertility men and oligoasthenospermia.
Table 1. Characteristics of normal fertility men and oligoasthenospermia.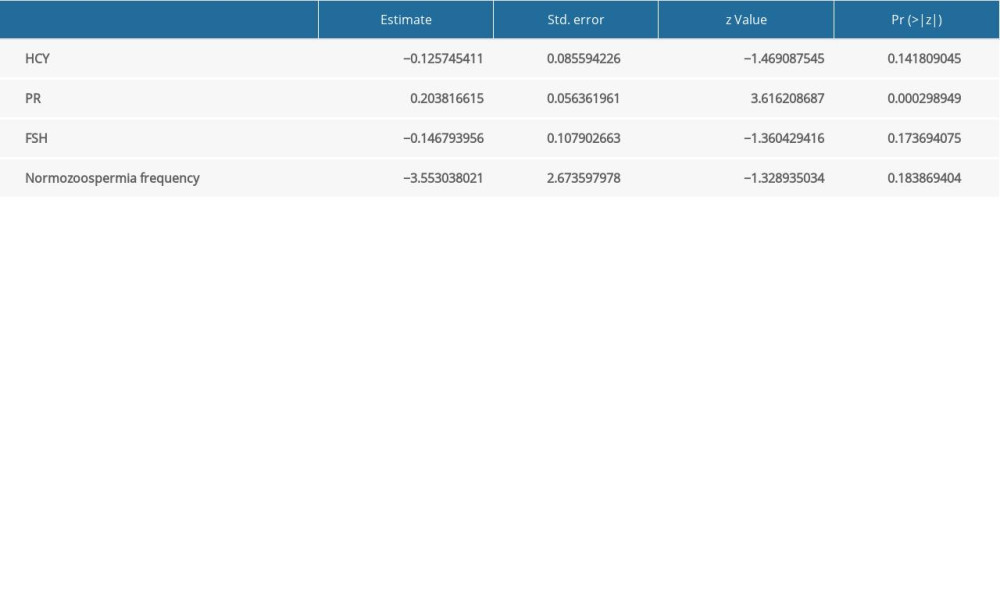 Table 2. Multivariable logistic regression model for successful natural conception.
Table 2. Multivariable logistic regression model for successful natural conception. Table 3. Prediction properties of based on internal validation.
Table 3. Prediction properties of based on internal validation. In Press
05 Mar 2024 : Clinical Research
Muscular Function Recovery from General Anesthesia in 132 Patients Undergoing Surgery with Acceleromyograph...Med Sci Monit In Press; DOI: 10.12659/MSM.942780
05 Mar 2024 : Clinical Research
Effects of Thermal Insulation on Recovery and Comfort of Patients Undergoing Holmium Laser LithotripsyMed Sci Monit In Press; DOI: 10.12659/MSM.942836
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952