27 October 2020: Clinical Research
Left-Behind Status Worsens Prognosis of ST-Elevation Myocardial Infarction in Elderly Patients from Southwest China
Maolin Cao1BCDE, Zhe Zhang2BCDE, Shichuan Li3B, Yan Chen1B, Shunkang Rong4B, Bo Li5B, Zijun Chen1AG*DOI: 10.12659/MSM.927300
Med Sci Monit 2020; 26:e927300
Abstract
BACKGROUND: This study aimed to assess the association between left-behind status and the prognosis of ST-elevation myocardial infarction (STEMI).
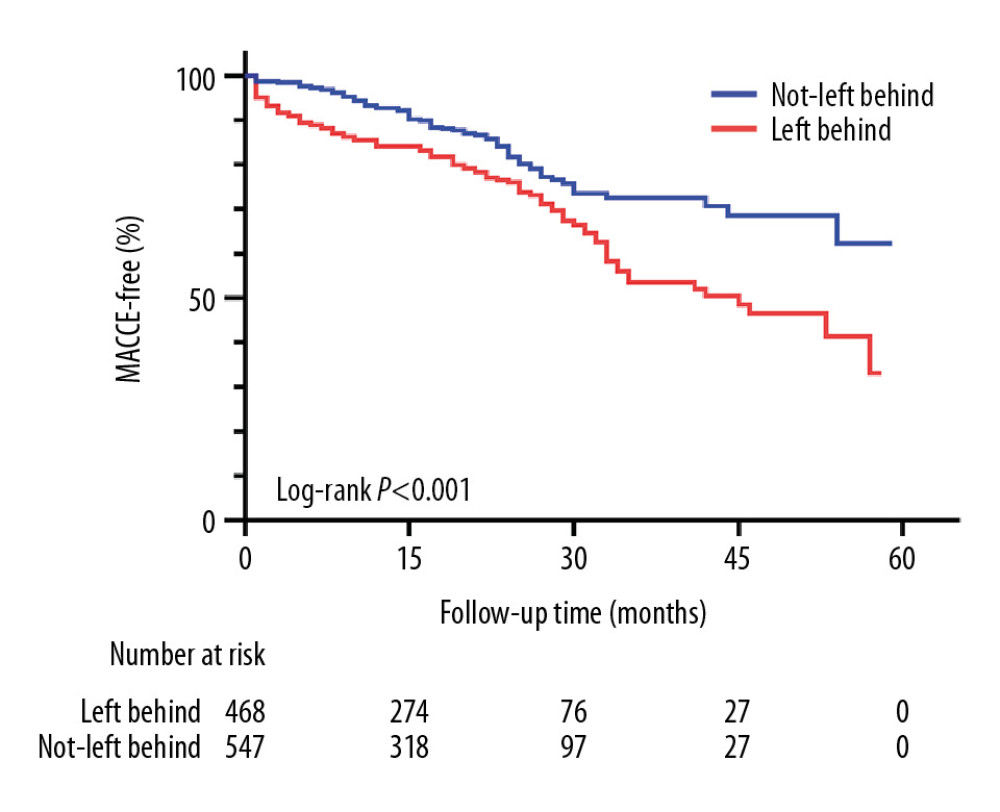
MATERIAL AND METHODS: A total of 1 015 patients with STEMI patients from 4 tertiary medical centers in southwest China were enrolled and categorized into left-behind and not-left-behind groups. The primary endpoints were major adverse cardiovascular and cerebrovascular events (MACCEs), which were assessed with Kaplan-Meier curves. Multivariate Cox regression analyses were used to explore the predictive value of left-behind status for MACCEs.
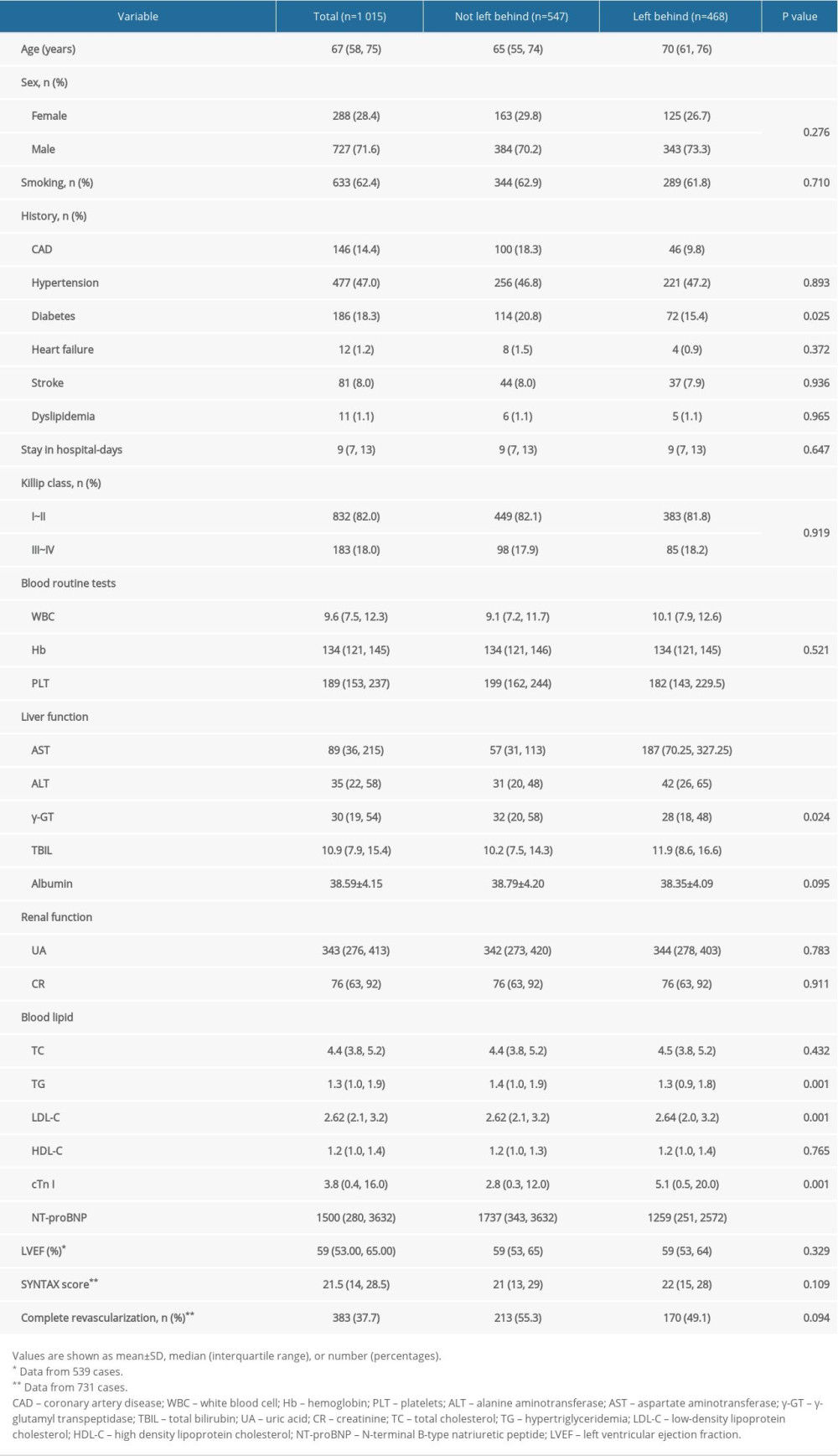
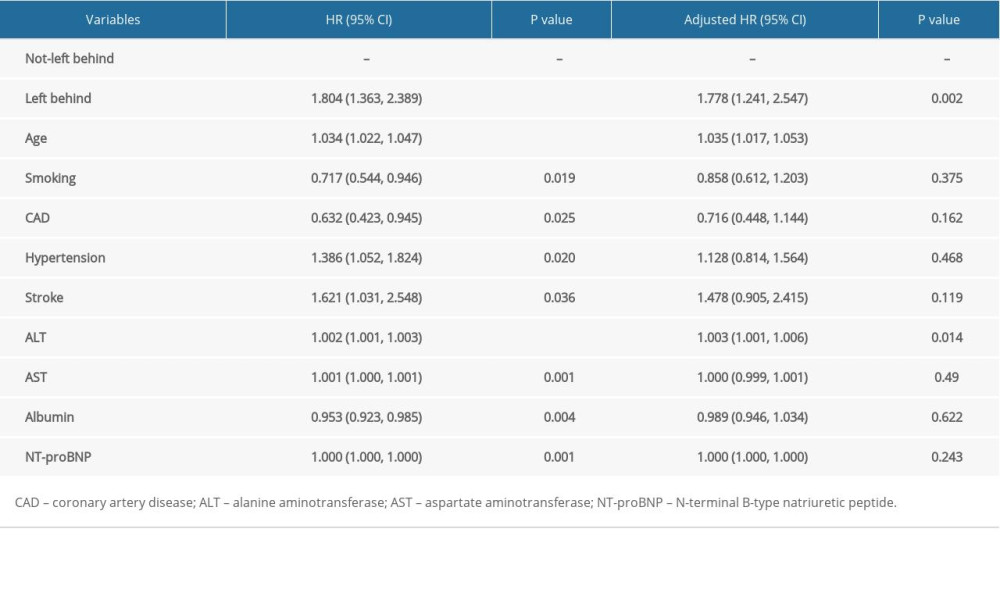
RESULTS: Patients in the left-behind group were older than those in the not-left-behind group (70 vs. 65 years, P<0.001). The patients in the left-behind group had a lower incidence of history of coronary heart disease and diabetes mellitus than those in the not-left-behind group. Meanwhile, the left-behind group had higher levels of alanine aminotransferase (42 vs. 31, P<0.001), low-density lipoprotein cholesterol concentration (2.64 vs. 2.62, P=0.001) and cardiac troponin I (5.11 vs. 2.84, P=0.001) than the not-left-behind group. During the 18-month follow-up, the left-behind group experienced a higher rate of adverse events than the not-left-behind group (123/26.2% vs. 81/14.8%, P<0.001). After multivariate adjustment, the left-behind group also had a 1.778-fold (95% CI: 1.241–2.547, P=0.002) higher risk of experiencing MACCEs than the not-left-behind group.
CONCLUSIONS: Left-behind status is an independent predictor of STEMI prognosis.
Keywords: Frail Elderly, Social Conditions, Alanine Transaminase, Cholesterol, LDL, Risk Factors, ST elevation myocardial infarction, Social factors, Tertiary Care Centers, troponin I
Background
With an increasing elderly population in China, ST-elevation myocardial infarction (STEMI) has become a major public health issue due to its high morbidity and mortality rates. Post-hospitalization care, including physical and psychological care, is important for STEMI patients. In East and Southeast Asia, elderly patients are mostly cared for by their children [1] because of a fundamental and traditional belief that family is the major source of financial support, love, and care for its elderly members. This belief emphasizes a son’s duty to respect and support his parents [2]. However, with recent industrialization and urbanization in China, the younger generation has migrated to the country’s cities and eastern regions in search of better employment opportunities and salaries, leaving their aging parents behind. By the end of 2016 in China, the total population of elderly individuals was 230 million, of which 51.1% had been left behind [3].
Because of the increasing popularity of leaving the elderly behind, more researchers are now focusing on this special population [4,5]. It is clear that those left behind suffer from poorer mental and physical health outcomes, such as depression, anxiety, and cognitive impairment [6]. Almost all of the existing research is focused on describing the mental health of these individuals [4–6]. Very little evidence is available on the relationship between left-behind status and the prognosis of special chronic diseases [7], especially that of myocardial infarction, which has increasingly gained importance as a serious health condition. Heart disease is a leading cause of death in China, with 700 000 new cases of acute myocardial infarction reported each year [8]. Therefore, in this study, we explored the relationship between the left-behind status of patients with STEMI and the prognosis of acute myocardial infarction.
Material and Methods
Approximately 1 628 STEMI patients who received percutaneous coronary intervention at 4 tertiary medical centers in southwest China from January 2013 to January 2015 were retrospectively enrolled. Of these, 389 patients were ineligible and were excluded from the study; the ineligibility criteria included death in the hospital, absence of accurate contact information, childlessness, and solitary living. An additional 224 patients were lost to follow-up. Therefore, 1 015 patients were available for further screening. These patients were divided into 2 groups: the left-behind group (n=468) and the not-left-behind group (n=547). Left-behind status was defined as having adult children who remained absent for more than 6 months per year [7].
We collected information on clinical events through telephone follow-up every 12 months and from in-hospital and outpatient medical records. The last follow-up was conducted in January 2019. If a patient was unable or unwilling to attend the scheduled interview, information was gathered through a phone conversation between the study physicians and the patients’ relatives. Baseline data including sex, age, medical history, smoking status, blood glucose level, HbA1c level, echocardiography and coronary angiography findings, and cardiac function classification were collected.
The primary endpoints were major adverse cardiovascular and cerebrovascular events (MACCE), including all-cause and cardiovascular mortality, nonfatal myocardial infarction, urgent revascularization, and ischemic stroke.
This study was performed in accordance with institutional ethical standards and was approved by the ethical committee of the Yongchuan Hospital of Chongqing Medical University. The need to obtain informed consent was waived owing to the retrospective design of the study. The investigations were carried out following the principles of the Declaration of Helsinki.
All statistical analyses were conducted using SPSS software version 20.0 (SPSS Inc, Chicago, IL, USA). Continuous, normally distributed variables were presented as means and standard deviations and were compared between the 2 groups using
Results
Of the 1 015 patients included, 46.1% were left-behind, constituting the left-behind group. These individuals were older than those in the not-left-behind group (70
Conversely, patients in the left-behind group had lower platelet counts and NT-proBNP levels than those in the not-left-behind group (82
During the median follow-up at 18 months, 204 MACCEs were observed: 123 (26.2%) in the left-behind group and 81 (14.8%) in the not-left-behind group. Kaplan-Meier curves for primary outcomes are shown in the Figure 1 (log-rank test
After adjusting for age, smoking, history of coronary artery disease, hypertension, stroke, and ALT and AST levels, the left-behind group was at a higher risk of experiencing primary outcomes than the not-left-behind group (hazard ratio (HR): 1.778, 95% confidence interval: 1.241–2.547,
Discussion
In this study, we demonstrated that left-behind status was associated with adverse cardiovascular outcomes in STEMI patients. This is a new indicator, independent of the traditional risk factors such as age, left ventricular ejection fraction, cTn I level, and physical inactivity. To the best of our knowledge, this is the first study to identify the connection between the prognosis of STEMI and left-behind status.
With unbalanced economic development and accelerated urbanization in China over the past 3 decades, the number of left-behind elderly is rapidly rising. In our study, 46.1% of the study subjects were left-behind individuals, a Figure1 that is in line with the statistics (51.1%) reported in the literature [3]. Although leaving elderly parents behind is a common phenomenon, most of the research on left-behind parents is conducted in emerging Asian countries, where multiple generations of a family often live in the same household [9–11]. In these countries, child migration creates the “left-behind” phenomenon; in contrast, in the American and European cultures, children are expected to leave their parents after reaching adulthood.
Being left-behind means older parents receive better financial support from their children [12] and engage in increased physical activity [13], such as agricultural and domestic work, which may in turn benefit their health [13]. Improved financial support is crucial for elderly left-behind individuals in the absence of a mature social protection system comprised of pensions and accessible and affordable health care, especially in rural areas [14]. This theory is consistent with our present study in which we found that the prevalence of diabetes mellitus and cardiovascular diseases was lower in the left-behind group than in the not-left-behind group. However, researchers have found that left-behind status is significantly associated with mental and physical diseases [9–11]. In rural China, the migration of sons increases the risk of stomach and other digestive diseases by a factor of 1.29 [7]. Furthermore, the left-behind elderly parents experience higher degrees of loneliness, depressive symptoms, and cognitive impairment. Magnetic resonance imaging showed that the left-behind elderly parents have a higher progression of structural brain changes (white matter lesions) than the not-left-behind elderly parents [15]. Approximately 10.9% to 43.6% of the left-behind elderly parents in the rural areas of China suffer from moderate to serious loneliness [16], while in Europe, the prevalence of depression in community-dwelling populations above 65 years of age is approximately 12.3% [17]. These mental health problems may lead to a higher risk of endocrine disorders and immune dysfunction in the left-behind group, which could further cause various diseases, such as cancer [18].
In the present study, we found that left-behind patients with STEMI experienced worse clinical events than patients with STEMI who were not left behind. There are several explanations for this. First, the left-behind group had more severe cardiac conditions, which may be attributed to their older age and higher cTn I and LDL-C levels. Previous studies revealed that left-behind elderly parents with migrant children are less likely to receive health care and be taken to the hospital than those who live with their children [3,19]. This may lead to an increase in the perfusion time when myocardial infarction occurs [20]. Patients with more severe cardiac conditions and higher ages are more likely to have poor medication compliance, which is an important secondary preventive measure to reduce the risk of recurrent events for cardiovascular disease [21].
Second, left-behind individuals have poorer mental health, which is the most important factor influencing their quality of life [5, 22]. Though our research excluded patients who lived alone, the included patients may have experienced loneliness even while living with their spouses. It was found that 33% of married women and 45% of married men feel lonely while living with their spouse or others [23]. Furthermore, left-behind elderly women who experienced loneliness have a 2.9 times greater risk of all-cause mortality in STEMI than those who did not feel lonely, while the left-behind men have 2.1 times greater risk [24].
Third, the left-behind group has an unhealthier lifestyle than the not-left-behind group. An increase in household incomes (contributed by the migrant children) leads to unhealthy diets that are high in fat and sugar [25]. Furthermore, to alleviate mental illnesses and stress, the left-behind elderly parents consume more tobacco and alcohol than the not-left-behind elderly parents [26,27]. These habits are negatively associated with their health outcomes.
Future targets for intervention in the poor prognosis of left-behind patients with STEMI should focus on encouraging adult children to pay more attention to their parents and find a job as near to their parents’ residence as possible. Such initiatives are being undertaken by the Chinese government [28]. At the same time, improving the mental health condition and providing more convenient access to health care is beneficial for such left-behind elderly individuals.
This study should be interpreted in the context of its limitations. First, as this is a retrospective study, we could not investigate the effect of communication between the left-behind parents and their children; this communication is helpful in alleviating the parents’ loneliness, dispelling their negative emotions, and possibly improving their mental health [29]. Second, we did not evaluate the patients’ psychological states, which can affect the prognosis of STEMI [24].
Conclusions
In conclusion, we found that left-behind status was an independent risk factor for the prognosis of STEMI. The left-behind group with STEMI had a 1.778-fold higher risk of experiencing MACCEs. More effort is needed to improve the prognosis of the left-behind elderly population with STEMI.
References
1. Chou RJA, Filial piety by contract? The emergence, implementation, and implications of the “family support agreement” in China: Gerontologist, 2010; 51(1); 3-16
2. Biao X, How far are the left-behind left behind? A preliminary study in rural China: Popul Space Place, 2007; 13; 179-91
3. China National Committee on Ageing (CNCA): Survey of Home-Based Care of 10,000 Elderly People in Ten Cities http://www.cncaprc.gov.cn/contents/7/4898.html
4. Zhong Y, Schön P, Burström B, Burström K, Association between social capital and health-related quality of life among left behind and not left behind older people in rural China: BMC Geriatr, 2017; 17; 287
5. Xie JF, Ding SQ, Zhong ZQ, Mental health is the most important factor influencing quality of life in elderly left behind when families migrate out of rural China: Rev Lat Am Enfermagem, 2014; 22; 364-70
6. Thapa DK, Visentin D, Kornhaber R, Cleary M, Migration of adult children and mental health of older parents ‘left behind’: An integrative review: PLoS One, 2018; 13; e0205665
7. Evandrou M, Falkingham J, Qin M, Vlachantoni A, Children’s migration and chronic illness among older parents ‘left behind’ in China: SSM Popul Health, 2017; 3; 803-7
8. Du X, Pi Y, Dreyer RP, The china patient-centered evaluative assessment of cardiac events (PEACE) prospective study of percutaneous coronary intervention: study design: Catheter Cardiovasc Interv, 2016; 88; E212-21
9. Sekhon H, Minhas S, An insight into mental health of elderly family members of emigrants from Punjab, India: Int J Res Health Sci, 2014; 2; 30-35
10. Ashfaq A, Abbasi SU, Ali R, Habiba U, Elderly parents and international migration of sons: Evidence from Pakistan and Azad Jammu & Kashmir: J Identity Migr Stud, 2016; 10; 53-65
11. Kuhn R, Everett B, Silvey R, The effects of children’s migration on elderly kin’s health: A counterfactual approach: Demography, 2011; 48; 183-209
12. Xiang AO, Jiang D, Zhao Z, The impact of rural–urban migration on the health of the left-behind parents: China Econ Rev, 2015; 37; 126-39
13. Weuve J, Kang JH, Manson JE, Physical activity, including walking, and cognitive function in older women: JAMA, 2004; 292; 1454-61
14. He C, Ye JZ, Impact study on the rural labor force migrant working to the life care of left-behind elders: Issues in Agricultural Economy, 2010; 3; 46-53
15. Duan D, Dong Y, Zhang H, Empty-nest-related psychological distress is associated with progression of brain white matter lesions and cognitive impairment in the elderly: Sci Rep, 2017; 7; 43816
16. Liu LJ, Guo Q, Loneliness and health-related quality of life for the empty nest elderly in the rural area of a mountainous county in China: Qual Life Res, 2007; 16; 1275-80
17. Copeland JR, Beekman AT, Braam AW, Depression among older people in Europe: The EURODEP studies: World Psychiatry, 2004; 3; 45-49
18. Zhou C, Ji C, Chu J, Non-use of health care service among empty-nest elderly in Shandong, China: a cross-sectional study: BMC Health Serv Res, 2015; 15; 294
19. Falkingham J, Qin M, Vlachantoni A, Evandrou M, Children’s migration and lifestyle-related chronic disease among older parents ‘left behind’ in india: SSM Popul Health, 2017; 3; 352-57
20. Ohama A, Mizuguchi Y, Hashimoto S, Impact of living alone on the care and outcomes of patients with ST-elevation myocardial infarction: J Cardiol, 2020; 75; 628-34
21. Shang P, Liu GG, Zheng X, Association between medication adherence and 1-year major cardiovascular adverse events after acute myocardial infarction in China: J Am Heart Assoc, 2019; 8; e011793
22. Liu LJ, Sun X, Zhang CL, Guo Q, Health-care utilization among empty-nesters in the rural area of a mountainous county in China: Public Health Rep, 2007; 122; 407-13
23. He G, Xie JF, Zhou JD, Depression in left-behind elderly in rural China: Prevalence and associated factors: Geriatr Gerontol Int, 2016; 16; 638-43
24. Christensen AV, Juel K, Ekholm O, Significantly increased risk of all-cause mortality among cardiac patients feeling lonely: Heart, 2020; 106; 140-46
25. Yoshida M, McKeown NM, Rogers G, Surrogate markers of insulin resistance are associated with consumption of sugar-sweetened drinks and fruit juice in middle and older-aged adults: J Nutr, 2007; 137; 2121-27
26. Epel E, Lapidus R, McEwen B, Brownell K, Stress may add bite to appetite in women: A laboratory study of stress-induced cortisol and eating behavior: Psychoneuroendocrinology, 2001; 26; 37-49
27. Jiang S, Chu J, Li C, Alcohol consumption is higher among left-behind Chinese children whose parents leave rural areas to work: Acta Paediatr, 2015; 104; 1298-304
28. Ministry of Human Resources and Social Security of the People’s Republic of China: Eliminate poverty [in Chinese]http://www.mohrss.gov.cn/SYrlzyhshbzb/dongtaixinwen/buneiyaowen/201807/t20180723_297851.html
29. Knodel J, Saengtienchai C, Rural parents with urban children: Social and economic implications of migration for the rural elderly in Thailand: Popul Space Place, 2007; 13; 193-210
In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952