16 January 2021: Clinical Research
Evaluation of 3-Dimensional Magnetic Resonance Imaging (3D MRI) in Diagnosing Anterior Talofibular Ligament Injury
Yan Xu1BCE, Lei He1BCE, Yu Han2CDF, Deyu Duan1AEG*, Liu Ouyang1AEGDOI: 10.12659/MSM.927920
Med Sci Monit 2021; 27:e927920
Abstract
BACKGROUND: It is challenging to entirely show the anterior talofibular ligament (ATFL) and accurately diagnose ATFL injury with traditional 2-dimensional (2D) magnetic resonance imaging (MRI). With the introduction of 3.0T MRI, a 3-dimensional (3D) MRI sequence can achieve images with high spatial resolution. This study aimed to evaluate the accuracy of 3D MRI and compare it with 2D MRI in diagnosing ATFL injury.
MATERIAL AND METHODS: This was a prospective study in which 45 patients with clinically suspected ATFL injury underwent 2D MRI, 3D MRI, and 3D model reconstruction followed by arthroscopic surgery between February 2018 and April 2019. Two radiologists who had over 11 and 13 years of musculoskeletal experience assessed the injury of ATFL in consensus without any clinical clues. Arthroscopic surgery results were the standard reference of MRI accuracy.
RESULTS: The 3D MRI results of ATFL injury showed the sensitivity of diagnosis of complete tears of 83% and specificity of 82%. The partial tears diagnosis sensitivity was 78%, and specificity was 100%. The sensitivity of diagnosis of sprains was 100%, and the specificity was 97%. The 3D MRI accuracy of diagnosis was 98% for no injury, 98% for sprain, 91% for partial tear, and 82% for complete tear. The difference in the diagnosis of sprain and partial tears by 3D MRI and 2D MRI was statistically significant (P<0.05). A 3D reconstruction model was successfully created for all patients.
CONCLUSIONS: 3D MRI may be a reliable and accurate method to detect ATFL injury. The 3D reconstruction model using 3D MRI sequences has excellent prospects in application.
Keywords: Dimensional Measurement Accuracy, Lateral Ligament, Ankle, Magnetic Resonance Angiography, Adolescent, Imaging, Three-Dimensional, Knee Injuries, Magnetic Resonance Imaging
Background
The ankle sprain that occurs during daily life and sport activities is mainly accompanied by a varus injury, which has a high risk of damaging the lateral ligament [1,2]. Injury to the anterior talofibular ligament (ATFL) alone accounts for 80% of total injuries to the ankle ligament [3]. Clinically, X-rays often show no fractures after ankle sprains. Consequently, doctors neglect to treat lateral ligament injury, which can then lead to traumatic severe osteoarthritis and osteonecrosis of the ankle joint, seriously inhibiting the quality of life of patients. Magnetic resonance imaging (MRI) is usually the diagnostic device chosen in cases with delayed healing and persistent symptoms of an ankle sprain and in elite athletes. The ATFL is oriented obliquely and is thinner than a normal ligament. Therefore, it cannot be detected in its entirety on the conventional 2-dimensional (2D) sequence, which uses relatively thick slices (3–4 mm) [4]. With the introduction of 3.0T MRI, images with high spatial resolution from using 3-dimensional (3D) MRI sequences can be obtained [5]. An optimized plane can be chosen to visualize the ATFL clearly and entirely; also, a 3D reconstruction model can be obtained through 3D sequences, thus helping to improve understanding of the injury by displaying the ligament damage visually. Diagnosing ATFL damage with 3D MRI provides an essential, timely, and accurate diagnosis that allows a surgeon to decide whether surgery is needed [6].
Our study aimed to assess the accuracy of 3D MRI, compared with 2D MRI, in diagnosing ATFL injury, using arthroscopic surgery findings as the standard reference of accuracy.
Material and Methods
PATIENTS:
The study included 45 patients who underwent arthroscopic surgery on 1 ankle in the Wuhan Union Hospital. This study was approved by the Ethics Committee of the hospital). All participants had signed informed consent before the study. All patients who underwent arthroscopy had symptoms of chronic ankle instability: lateral ankle pain and swelling for over 6 months and point tenderness over the lateral portion of the ankle on physical examination. The inclusion criteria were as follows: (1) lateral ankle pain and swelling after conservative treatment of at least 6 weeks; (2) positive clinical clues (anterior drawer test + or talar tilt test +); (3) point tenderness on the lateral ankle; (4) the sprain occurred at least 6 months prior to going to hospital; and (5) history of recurrent sprain and 2 or more sprains on the same ankle. Patients who had a history of previous ankle surgeries, ankle fracture, or rheumatoid disease were excluded from the study. From February 2018 to April 2019, 45 patients (27 men and 22 women; mean age, 32.1 years, range, 18–58 years) were included in the study.
All patients were examined using a 3.0-T MRI with a knee inspection coil. They were placed in a supine position, with the ankle in a neutral position. They were positioned and examined by the same scanning technician. The MRI conditions were as follows: 3D sequence, proton density-weighted turbo spin-echo, repetition time/echo time: 6.3/3.2); 30° flip angle; voxel, 0.6 mm isotropic; and acquisition, 8–9 min. Two radiologists who had over 11 and 13 years of musculoskeletal experience assessed the injury of ATFL in consensus without any clinical clues. The MRI images were stored in the DICOM 3.0 standard format and in Mimics 16.0 software. Then, a 3D reconstruction model of the ATFL was built. All patients also underwent 2D MRI scan sequences.
The arthroscopic assessment was performed before surgery by a senior ankle surgeon who had more than 17 years of related surgical experience. The surgeon examined the condition of the ligaments of the ankle. All patients undergoing arthroscopy had over 6 months from injury to surgery. The damage criteria were as follows: (1) sprain: the ligament was intact but thinner or looser; (2) complete tear: the ligament had definite discontinuity; and (3) partial tear: the ligament fiber had partial adhesion, intact continuity was observed, and the fiber surface was coarsely cut. The findings of arthroscopy were the standard reference of MRI accuracy. Patients needing ankle arthroscopy were selected for this study based on our inclusion criteria: all enrolled patients had chronic ankle instability symptoms and point tenderness. Other associated ligament injuries are not discussed in detail because they are outside the scope of this article. The study flow chart (Figure 1).
STATISTICAL ANALYSIS:
The statistical data were analyzed using SPSS software version 22 (SPSS Inc, Chicago, IL, USA). The confidence interval was 95%. The chi-square test was used to compare the accuracy, sensitivity, specificity, and positive and negative predictive values of the ATFL between 2D MRI and 3D MRI. Sensitivity=(true positive/(false negative+false positive)); specificity=(true negative/(true negative+false positive)); and accuracy=((true positive+true negative)/(true positive+true negative+false negative+false positive)). A
Results
A total of 45 patients underwent a 2D MRI scan, 3D MRI scan, and arthroscopy. All 3D MRI sequences were reconstructed into a 3D ATFL model. According to the classification of ankle damage, 8 normal ATFL, 7 sprains, 14 partial tears, and 16 complete tears of ATFL were detected by arthroscopy. However, differences were found between the findings of 2D MRI and 3D MRI (Table 1). MRI and arthroscopic surgery findings in the diagnosis of ATFL were inconsistent (Table 2). According to the 3D MRI findings, the sensitivity of diagnosis of normal ATFL was 89%, specificity was 100%, and accuracy was 98%. The sensitivity of the diagnosis of sprains was 100%, the specificity was 97%, and the accuracy was 93%. The sensitivity of the diagnosis was 78% for partial tears, with specificity and accuracy of 100% and 91%, respectively. The positive predictive value of 3D MRI findings ranged from 86% to 100%, the negative predictive value ranged from 87% to 100%, and the findings of 3D MRI were more accurate than those of 2D MRI (Table 3). The difference in the diagnosis of sprain and partial tears by 3D MRI and 2D MRI was statistically significant (
Discussion
Our study was performed to assess the significance of 3D MRI in the diagnosis of ATFL injury. We found that 3D MRI was more reliable in diagnosing minor injuries, especially sprains and partial tears, while there was no significant difference between 2D MRI and 3D MRI in the diagnosis of normal and complete rupture. 3D MRI is important for the diagnosis of ligament injury in chronic ankle sprain of patients, including elite athletes. A timely and clear diagnosis is conducive to making timely choices of surgical or other treatment and to helping patients recover the function of the ankle quickly. Chronic ankle instability can affect the knee, hip, and even the spine. 3D MRI is a very promising device for ankle sprain.
Commonly used imaging methods for the clinical diagnosis of a ligament injury include stress X-ray, arthrography, MRI, and arthroscopy. MRI has the ability to display soft tissues and the advantages of noninvasiveness, rapid evaluation, multiplanar display, and no radiation damage. Numerous studies have reported that MRI examination has a high diagnostic value [7–9]. Kumar et al. reported a sensitivity of ATFL tears of 60%, accuracy of 72%, and specificity of 87% [10]. Park et al. reported lower ATFL tear sensitivity (44–75%), but higher specificity (78–88%) [11]. Kumar et al. and Park et al. used the 2D MRI sequence, and their findings were consistent with the results of the present study in which MRI showed more injury than did surgery, probably because MRI is more sensitive to damage, and some damage was invisible under arthroscopy. In the present study, 3D MRI showed ATFL tear sensitivity of 78% to 100%, specificity of 97% to 100%, and accuracy of 82% to 100%. These values were higher than those of 2D MRI, as the 3D MRI sequences had thinner sections compared with normal sequences. The ATFL could be observed only on several sections using a normal 2D MRI sequence owing to its anatomy. However, the 3D MRI sequence had more sections to show the ATFL tear. As shown in Figure 2, the 2D MRI sequence showed complete ATFL tear with poor tension, but on the same section, the 3D MRI sequence showed that 1 of the ATFLs was intact with poor tension (Figure 3), and the results were consistent with those of surgery (Figure 4). The 3D reconstruction model visually presented the information of the ATFL quickly and clearly (Figure 5). The 3D MRI showed advantages in diagnosing ATFL injury, as it significantly improved the diagnostic rate of ATFL injury. However, it had some limitations, including increased time to scan the selected area, requirement of relatively scarce radiology medical resources, and a high financial cost. Therefore, it could not be applied in all regions.
The 3D MRI sequence was input into the Mimics software, and the 3D reconstruction model was obtained to visualize the ATFL injuries. The section thickness of the 3D MRI scan was 0.3 mm, which was less than that of a 2D section (3–4 mm) [12]. The ATFL emanates from the anterior edge of the lateral malleolus and is attached to the talus neck. It is about 2 cm long and 6 mm to 8 mm wide [13]. The 3D MRI has more sections to show ATFL injury [14], and hence can display the injury more accurately. In this study, 3D MRI showed the potential for an improvement in accuracy and specificity in the diagnosis of ATFL injury. The 3D reconstruction model also showed encouraging results and had clinical significance in visualizing the injury. As shown in Figure 4, the condition of the ATFL could be directly observed using the 3D reconstruction model. In general, an experienced foot and ankle doctor can accurately diagnose ATFL damage using 3D MRI, but it is a challenge for young doctors or doctors in other fields, and patients can understand their condition only through the doctor’s explanation. The 3D models can shorten the learning curve of doctors and help patients understand the condition by themselves. The 3D reconstruction of bones is very common, but the reconstruction of ligaments needs further exploration [15]. The 3D reconstruction can be used in anatomical visualization, formulation of personalized diagnosis and treatment plans, simulation of surgical procedures, educational tools for medical research, medical training and teaching, communication among clinical staff, and patient education [16–19].
The 3D reconstruction model is a very promising technology. It can intuitively display the damage to ligaments, which is conducive to doctor-patient communication before surgery and improves the patient’s understanding of the condition. A personalized anatomical model helps doctors simulate an operation before surgery. The 3D reconstruction model has been widely used in the field of orthopedics [20,21]. It can be reconstructed from many kinds of data [10], and the 3D MRI sequence data are a good choice. Our next study will explore how to better perform 3D model reconstruction and simulate an operation before surgery.
This study had limitations. First, the sample size was small, and very few patients had complete ligament rupture, which affected the results. Second, all patients included in the study were selected by an experienced surgeon, and thus our results might not truly reflect the evaluation of the use of 3D MRI in diagnosing ATFL.
Conclusions
In conclusion, 3D MRI may be a reliable and accurate method to detect ATFL injury. The 3D reconstruction model using 3D MRI sequences has very good application prospects.
Figures
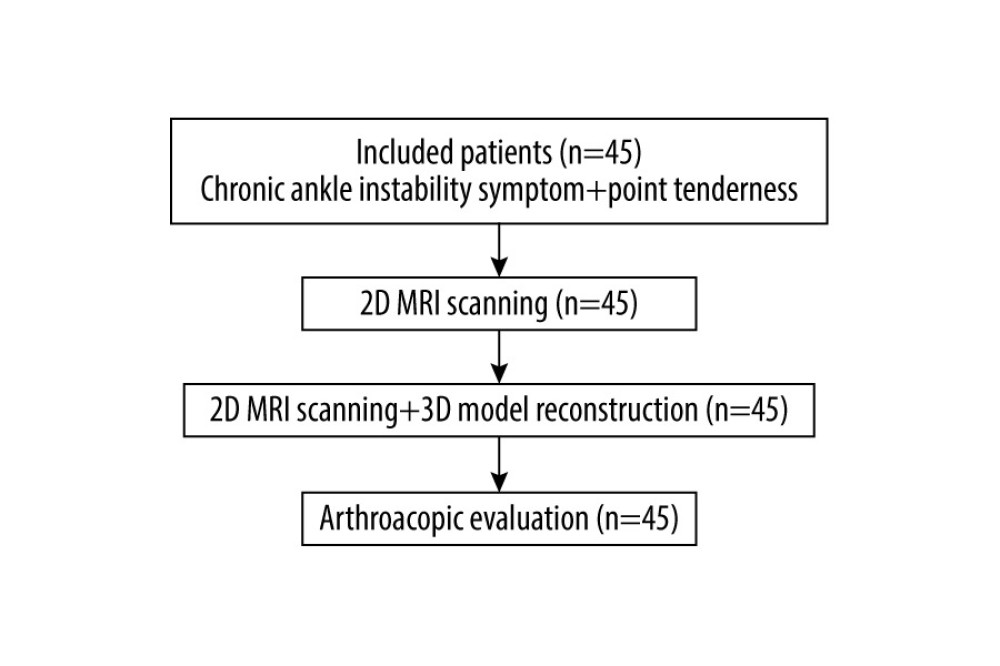 Figure 1. study flow chart.
Figure 1. study flow chart. 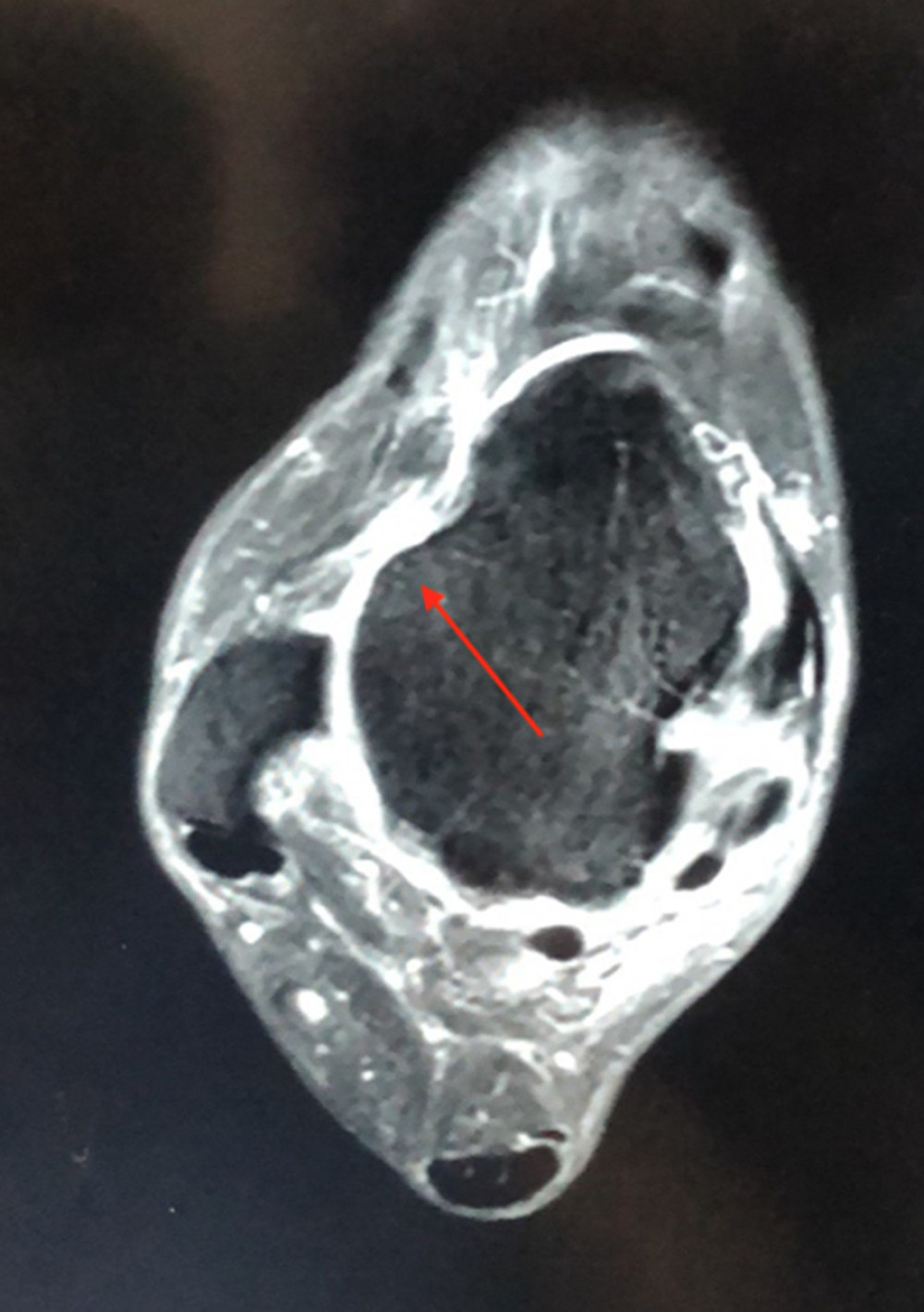 Figure 2. A 2-dimensional MRI image of a 45-year-old patient with anterior talofibular ligament (ATFL) injury, revealing a complete ATFL tear (arrow).
Figure 2. A 2-dimensional MRI image of a 45-year-old patient with anterior talofibular ligament (ATFL) injury, revealing a complete ATFL tear (arrow).  Figure 3. A 3-dimensional (3D) MRI image of a 45-year-old patient with an anterior talofibular ligament (ATFL) partial tear (arrow); this image was on the same section of 2D MRI. A break in 1 of the ATFL bundles was observed, but the ATFL was still consistent.
Figure 3. A 3-dimensional (3D) MRI image of a 45-year-old patient with an anterior talofibular ligament (ATFL) partial tear (arrow); this image was on the same section of 2D MRI. A break in 1 of the ATFL bundles was observed, but the ATFL was still consistent.  Figure 4. An arthroscopic image of a 45-year-old patient with an anterior talofibular ligament (ATFL) partial tear. The an ATFL had weakened tension and was partially broken. The results were consistent with those of MRI.
Figure 4. An arthroscopic image of a 45-year-old patient with an anterior talofibular ligament (ATFL) partial tear. The an ATFL had weakened tension and was partially broken. The results were consistent with those of MRI. 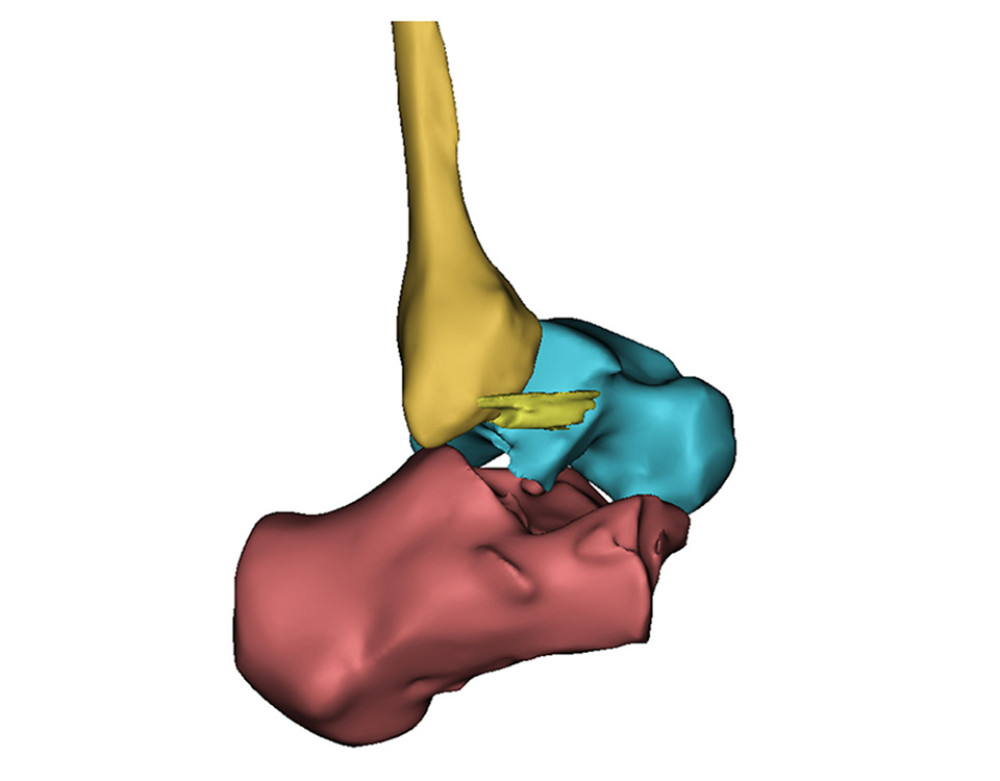 Figure 5. A 3-dimensional reconstruction model showing an anterior talofibular ligament partial tear. The results were consistent with arthroscopic surgery findings.
Figure 5. A 3-dimensional reconstruction model showing an anterior talofibular ligament partial tear. The results were consistent with arthroscopic surgery findings. References
1. Waterman BR, Owens BD, Davey S, The epidemiology of ankle sprains in the United States: J Bone Joint Surg Am, 2010; 92(13); 2279-84
2. Gerber JP, Williams GN, Scoville CR, Persistent disability associated with ankle sprains: A prospective examination of an athletic population: Foot Ankle Int, 1998; 19(10); 653-60
3. Malliaropoulos N, Papacostas E, Papalada A, Acute lateral ankle sprains in track and field athletes: An expanded classification: Foot Ankle Clin, 2006; 11(3); 497-507
4. Kim YS, Kim YB, Kim TG, Reliability and validity of magnetic resonance imaging for the evaluation of the anterior talofibular ligament in patients undergoing ankle arthroscopy: Arthroscopy, 2015; 31(8); 1540-47
5. Teramoto A, Akatsuka Y, Takashima H, 3D MRI evaluation of morphological characteristics of lateral ankle ligaments in injured patients and uninjured controls: J Orthop Sci, 2020; 25(1); 183-87
6. Tan DW, Teh DJW, Chee YH, Accuracy of magnetic resonance imaging in diagnosing lateral ankle ligament injuries: A comparative study with surgical findings and timings of scans: Asia Pac J Sports Med Arthrosc Rehabil Technol, 2016; 7; 15-20
7. Shengxuan C, Chen W, Xin M, Reliability and validity of different ankle MRI scanning planes for the anterior talofibular ligament injury diagnosis: A cadaveric study: J Orthop Surg Res, 2019; 14(1); 69
8. Jisook Y, Gyu CJ, Koo LY, MRI of the anterior talofibular ligament, talar cartilage and os subfibulare: Comparison of isotropic resolution 3D and conventional 2D T2-weighted fast spin-echo sequences at 3.0 T: Skeletal Radiol, 2016; 45(7); 899-908
9. Kanamoto T, Shiozaki Y, Tanaka Y, The use of MRI in pre-operative evaluation of anterior talofibular ligament in chronic ankle instability: Bone Joint Res, 2014; 3(8); 241-45
10. Kumar V, Triantafyllopoulos I, Panagopoulos A, Deficiencies of MRI in the diagnosis of chronic symptomatic lateral ankle ligament injuries: J Foot Ankle Surg, 2007; 13(4); 171-76
11. Park HJ, Cha SD, Kim SS, Accuracy of MRI findings in chronic lateral ankle ligament injury: Comparison with surgical findings: Clin Radiol, 2012; 67(4); 313-18
12. Kim TH, Moon SG, Jung HG, Subtalar instability: Imaging features of subtalar ligaments on 3D isotropic ankle MRI: BMC Musculoskelet Disord, 2017; 18(1); 475
13. Khawaji B, Soames R, The anterior talofibular ligament: A detailed morphological study: Foot (Edinb), 2015; 25(3); 141-47
14. Atsushi T, Yoshihiro A, Hiroyuki T, 3D MRI evaluation of morphological characteristics of lateral ankle ligaments in injured patients and uninjured controls: J Orthop Sci, 2020; 25(1); 183-87
15. Ripley B, Levin D, Kelil T, 3D printing from MRI data: Harnessing strengths and minimizing weaknesses: J Magn Reson Imaging, 2017; 45(3); 635-45
16. Mamoru S, Yasuo O, Atsushi K, Rapid prototyping of temporal bone for surgical training and medical education: Acta Otolaryngol, 2004; 124(4); 400-2
17. Zheng YX, Yu DF, Zhao JG: J Surg Educ, 2016; 73(3); 518-23
18. Silberstein JL, Maddox MM, Dorsey P, Physical models of renal malignancies using standard cross-sectional imaging and 3-dimensional printers: A pilot study: Urology, 2014; 849(2); 268-72
19. Bernhard JC, Isotani S, Matsugasumi T, Personalized 3D printed model of kidney and tumor anatomy: A useful tool for patient education: World J Urol, 2016; 34(3); 337-45
20. Ma L, Fan Z, Ning G, 3D Visualization and augmented reality for orthopedics: Adv Exp Med Biol, 2018; 1093; 193-205
21. Bagaria V, Bhansali R, Pawar P, 3D printing-creating a blueprint for the future of orthopedics: Current concept review and the road ahead!: J Clin Orthop Trauma, 2018; 9(3); 207-12
Figures
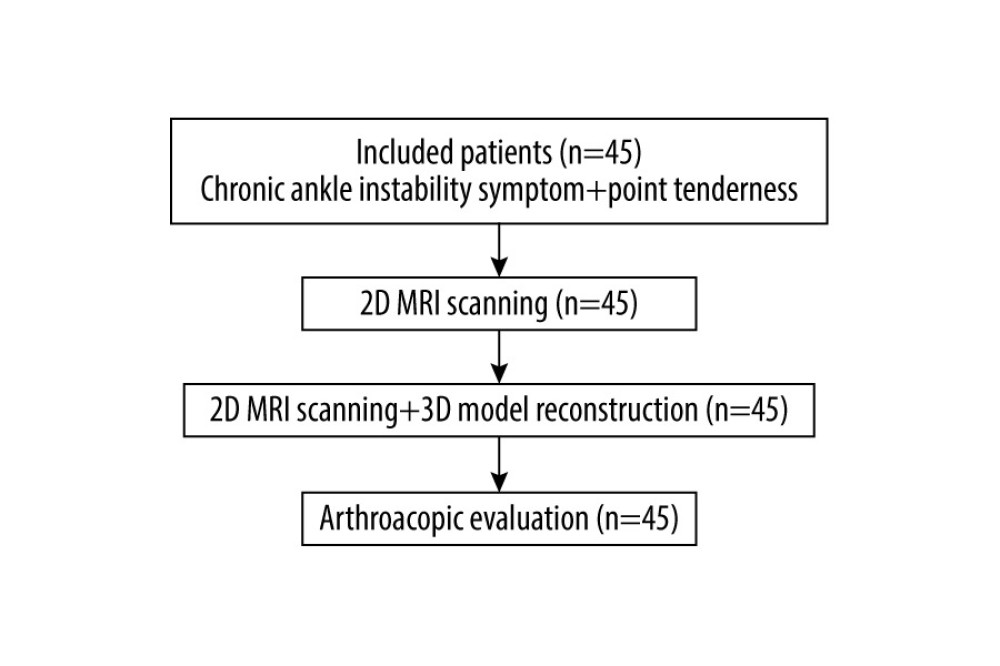 Figure 1. study flow chart.
Figure 1. study flow chart.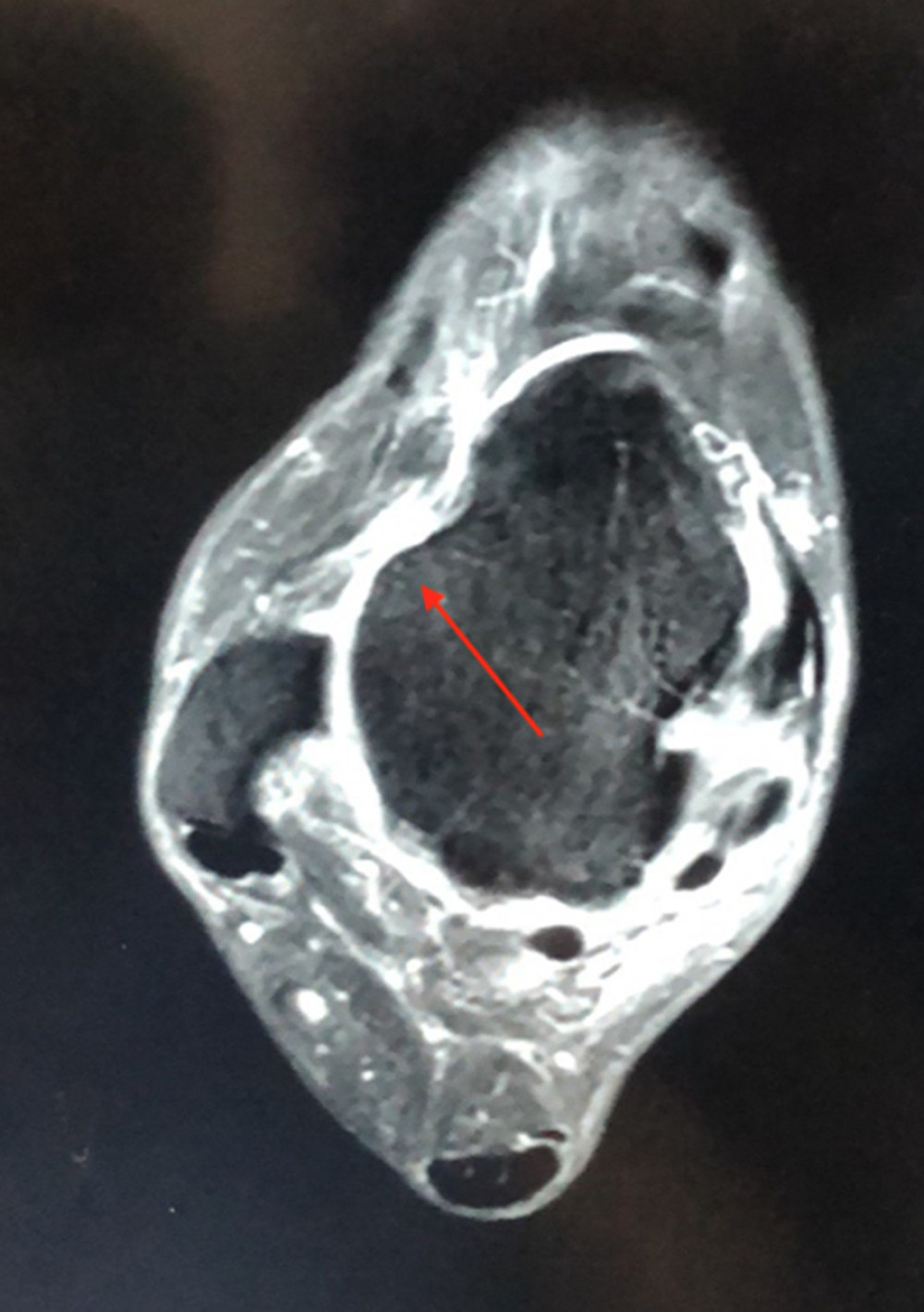 Figure 2. A 2-dimensional MRI image of a 45-year-old patient with anterior talofibular ligament (ATFL) injury, revealing a complete ATFL tear (arrow).
Figure 2. A 2-dimensional MRI image of a 45-year-old patient with anterior talofibular ligament (ATFL) injury, revealing a complete ATFL tear (arrow). Figure 3. A 3-dimensional (3D) MRI image of a 45-year-old patient with an anterior talofibular ligament (ATFL) partial tear (arrow); this image was on the same section of 2D MRI. A break in 1 of the ATFL bundles was observed, but the ATFL was still consistent.
Figure 3. A 3-dimensional (3D) MRI image of a 45-year-old patient with an anterior talofibular ligament (ATFL) partial tear (arrow); this image was on the same section of 2D MRI. A break in 1 of the ATFL bundles was observed, but the ATFL was still consistent. Figure 4. An arthroscopic image of a 45-year-old patient with an anterior talofibular ligament (ATFL) partial tear. The an ATFL had weakened tension and was partially broken. The results were consistent with those of MRI.
Figure 4. An arthroscopic image of a 45-year-old patient with an anterior talofibular ligament (ATFL) partial tear. The an ATFL had weakened tension and was partially broken. The results were consistent with those of MRI.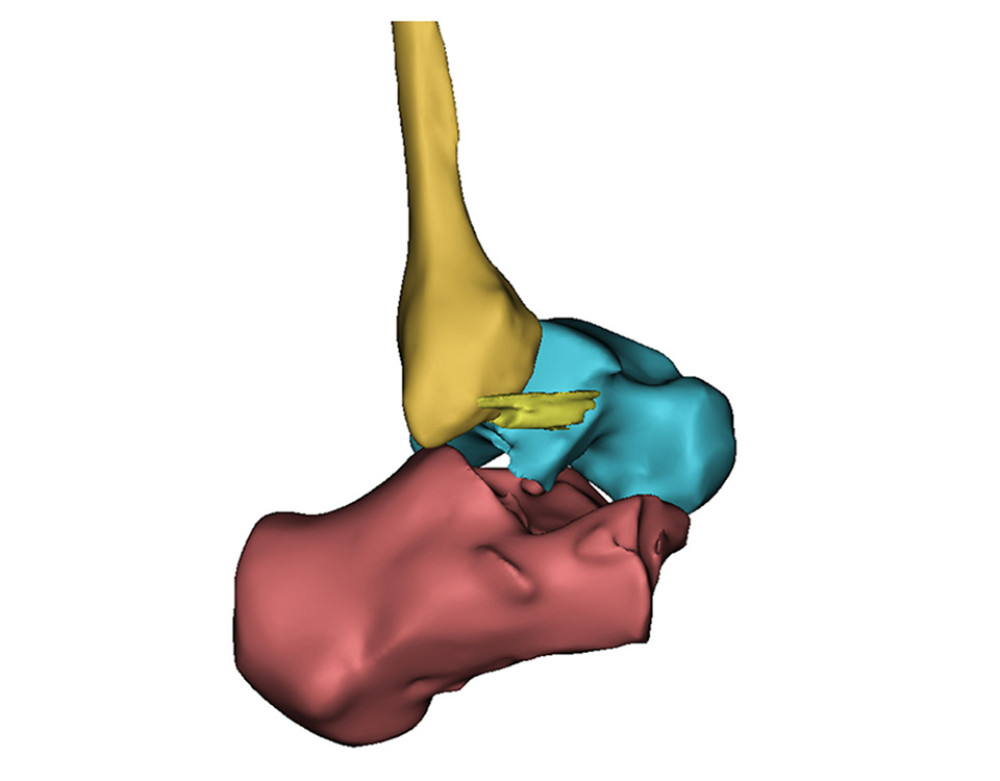 Figure 5. A 3-dimensional reconstruction model showing an anterior talofibular ligament partial tear. The results were consistent with arthroscopic surgery findings.
Figure 5. A 3-dimensional reconstruction model showing an anterior talofibular ligament partial tear. The results were consistent with arthroscopic surgery findings. Tables
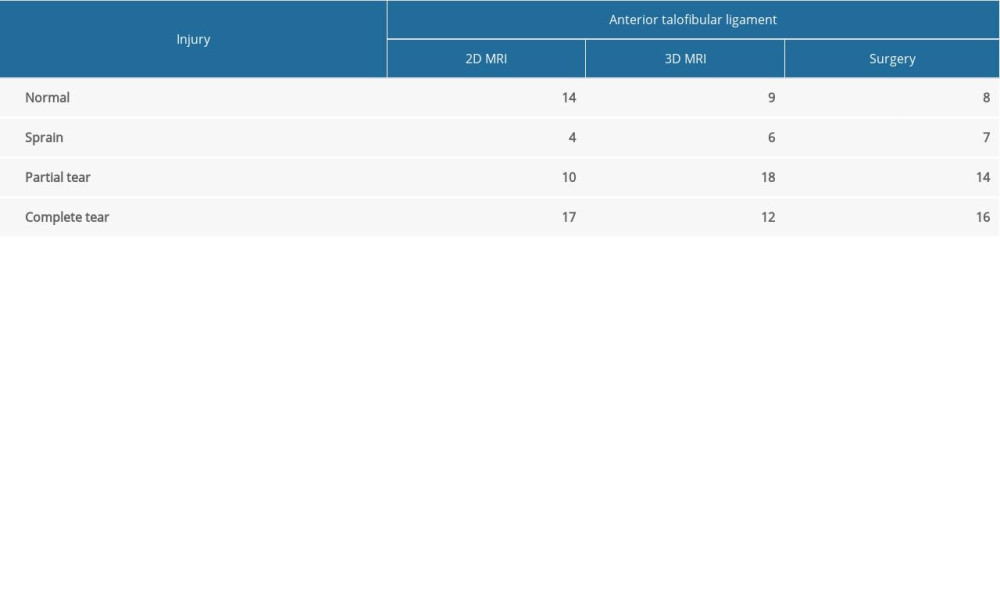 Table 1. General information of anterior talofibular ligament injuries.
Table 1. General information of anterior talofibular ligament injuries.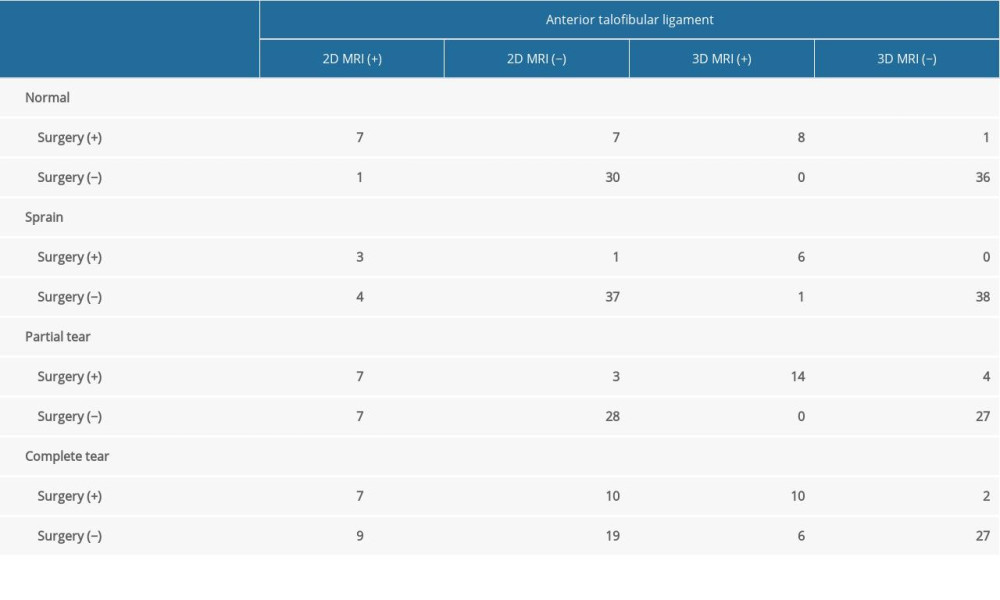 Table 2. Comparison of MRI and arthroscopic results.
Table 2. Comparison of MRI and arthroscopic results.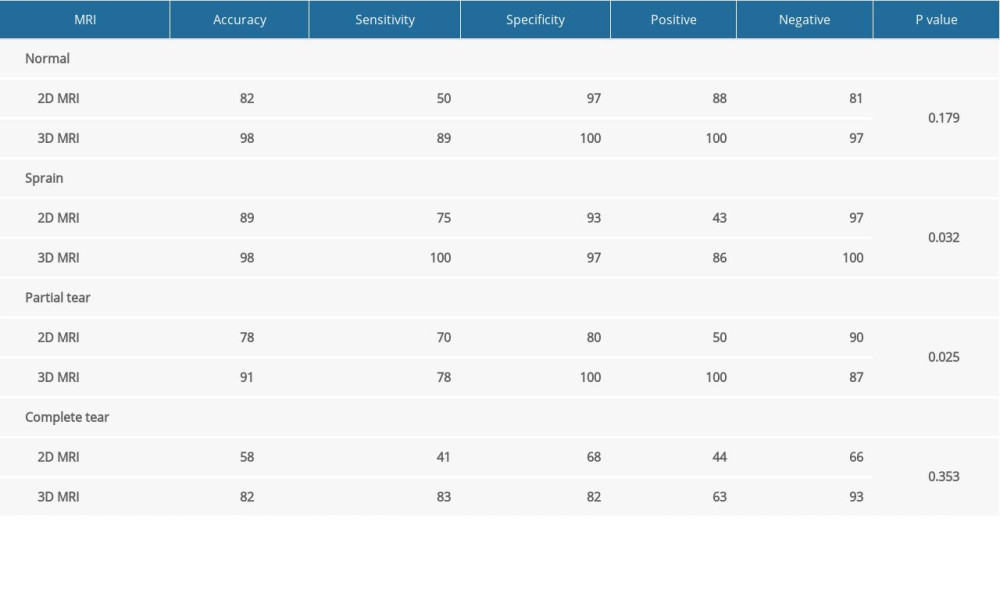 Table 3. Comparison of 2D and 3D MRI in diagnosing anterior talofibular ligament.
Table 3. Comparison of 2D and 3D MRI in diagnosing anterior talofibular ligament.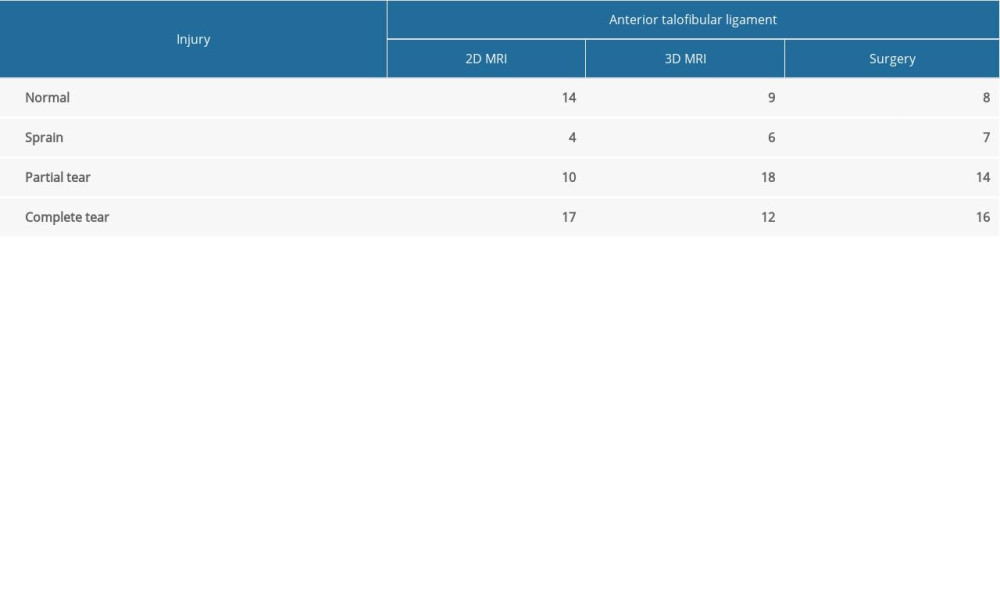 Table 1. General information of anterior talofibular ligament injuries.
Table 1. General information of anterior talofibular ligament injuries.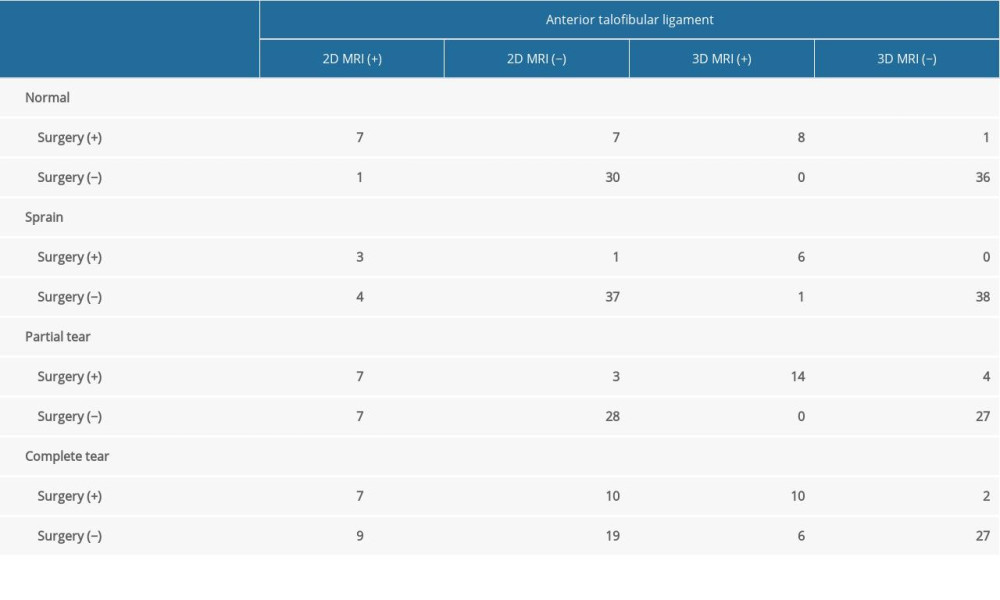 Table 2. Comparison of MRI and arthroscopic results.
Table 2. Comparison of MRI and arthroscopic results.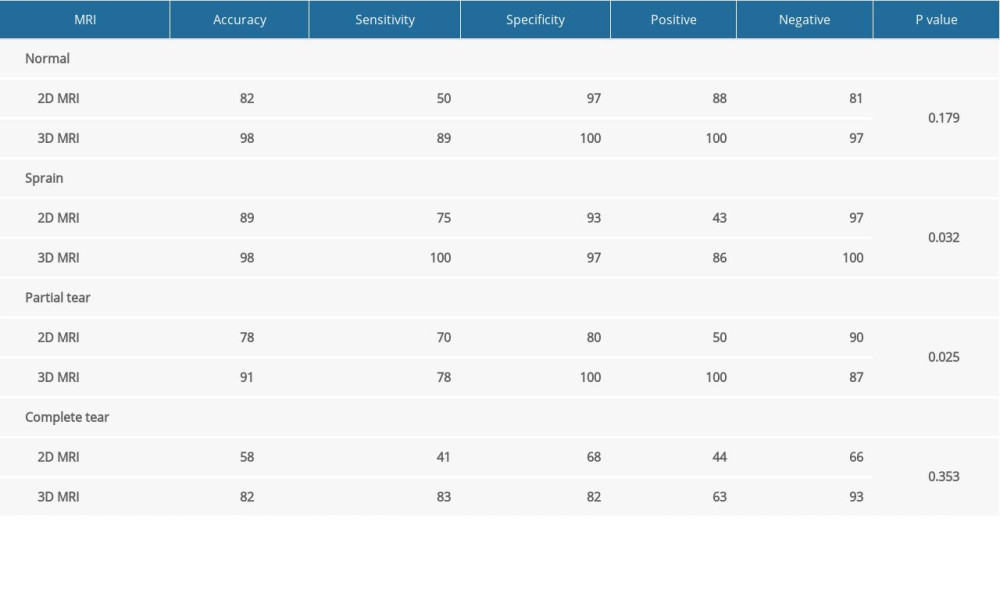 Table 3. Comparison of 2D and 3D MRI in diagnosing anterior talofibular ligament.
Table 3. Comparison of 2D and 3D MRI in diagnosing anterior talofibular ligament. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








