08 June 2021: Clinical Research
Visceral-to-Subcutaneous Fat Ratio Is a Potential Predictor of Postoperative Complications in Colorectal Cancer
An-Qi He1BCDEF, Chun-Qiang Li1BCDEF, Qi Zhang1B, Tong Liu1D, Jian Liu1F, Gang Liu1A*DOI: 10.12659/MSM.930329
Med Sci Monit 2021; 27:e930329
Abstract
BACKGROUND: Colorectal cancer (CRC) is one of the most common malignant tumors. Surgery is the primary treatment for CRC. Recent studies have shown that visceral-to-subcutaneous fat ratio (VSR) may be a potential indicator of risk. The aim of the present study was to determine whether VSR is a suitable predictor of the impact of postoperative complications in CRC.
MATERIAL AND METHODS: Clinical data from 129 patients were analyzed retrospectively. All patients underwent laparoscopic surgery for CRC. Preoperative imaging was used to quantify VSR. The primary outcome was 30-day postoperative complications. Multivariate logistic regression was used to determine the association between obesity indexes and postoperative complications.
RESULTS: There were 129 patients who underwent primary resections of colorectal cancer. At 30 days after surgery, postoperative complications had occurred in 33 (25.6%) patients. VSR was significantly associated with postoperative complications in multivariate analysis (P=0.032, OR 6.103, 95% CI 1.173-31.748). In ROC analysis, VSR was a potential predictor of complications (AUC 0.650). A cutoff value of VSR ≥0.707 was associated with 60% sensitivity and 29% specificity for postoperative complications. Patients with VSR ≥0.707 had 41.7% risk of morbidity, whereas those with <0.707 had 16.0% risk (P=0.001).
CONCLUSIONS: Our study shows that VSR is superior to VFA for prediction of the risk of complications following CRC laparoscopic surgery. We have also identified the optimal cutoff values for the use of VSR for this purpose. Measurement of VSR and identifying patients with increased risk of postoperative complications facilitate making perioperative decisions.
Keywords: Colorectal Neoplasms, Colorectal Surgery, Postoperative Complications, Body Mass Index, Intra-Abdominal Fat, Laparoscopy, Obesity, Risk Factors, Sensitivity and Specificity, subcutaneous fat
Background
Colorectal cancer (CRC) is one of the most common malignant tumors worldwide and is increasing in prevalence. Surgery is the primary treatment for CRC. However, complications of surgery may adversely influence oncologic outcomes [1–3].
Epidemiologic studies have shown a relationship between the higher incidence of CRC and that of obesity, especially in men, who demonstrate a 30–70% higher risk [4]. Obesity, as defined by BMI ≥30 kg/m2 was reported to be associated with an increased risk of postoperative complications [5–7]. Abdominal obesity as defined by a high visceral fat area (VFA) has been shown to be a more reliable predictor factor of poor abdominal surgery outcome than is BMI [8]. In addition, recent studies conducted in several countries have suggested that visceral-to-subcutaneous fat ratio (VSR) is an independent predictor of cardiovascular disease events and metabolic syndrome, and that this might be a more sensitive predictor than VFA [9]. However, although the relationship with VFA is well characterized, that with VSR is not.
Other studies regard visceral obesity as a dichotomous variable based on a given VFA cutoff value. Application of a given cutoff values may introduce interpretation bias into previously reported studies. To avoid this bias, it may be prudent to treat VFA and related variables as continuous variables rather than categorical variables [8].
Abdominal obesity has become a substantial public health problem and its incidence is increasing at a significantly higher rate than that of non-specific overweight/obesity. Because of this trend, the effect of abdominal obesity on the outcomes of CRC surgery requires further study. Therefore, we aimed to identify the optimal anthropometric measure for the precise estimation of the impact of abdominal obesity on the outcomes of CRC surgery, using a retrospective study.
Material and Methods
STUDY DESIGN AND PATIENTS:
This study was reviewed and approved by the Ethics Committee of Tianjin Medical University General Hospital with waiver of informed consent. Consecutive patients with CRC who were admitted to the Department of General Surgery at Tianjin Medical University General Hospital between July 2015 and September 2017 were considered for inclusion in the study. The inclusion criteria were: (1) a definitive diagnosis of CRC made before surgery and planned radical laparoscopic resection; (2) no hepatic, pulmonary, peritoneal, or other distant metastases had been identified in preoperative examinations; (3) a postoperative pathologic diagnosis had been made after an R0 resection; and (4) the patient did not receive neoadjuvant therapy and ostomy. The exclusion criteria were: (1) the patient’s physical condition was too poor to tolerate general anesthesia, defined as American Society of Anesthesiologists (ASA) physical fitness grade >III; (2) a planned laparotomy; and (3) a requirement for palliative surgery, because of intraoperative findings of peritoneal dissemination, distant metastasis, and/or extensive adhesion.
The data collected included preoperative demographic characteristics, intraoperative parameters, and postoperative conditions. The preoperative demographic characteristics were sex, age, height, body mass, and the presence of concomitant diseases (hypertension, diabetes mellitus, and/or coronary heart disease). In addition, hemoglobin and albumin concentrations were recorded. Height and body mass were measured just before surgery, and samples were collected for hemoglobin and albumin measurement on the morning of surgery. The intraoperative parameters were surgical time, volume of blood loss, and the number of lymph nodes that were dissected. The postoperative conditions were pathology and pathologic stage, as well as complications that developed within 1 month of surgery (wound infection, pneumonia, intra-abdominal infection, anastomotic leakage, and/or ileus).
ANTHROPOMETRIC MEASUREMENT:
Recently, there has been a great deal of interest in using computed tomography (CT) to measure abdominal adipose tissue [10,11]. Preoperative CT and specific scanning software were used to quantify the VFA and subcutaneous fat area (SFA) of each patient. During CT examination, the patients were supine and a sequential scan was performed from the right superior border of the diaphragm to the symphysis pubis. A single cross-sectional image was acquired at the level of the L4–L5 intervertebral space, and this was analyzed at a workstation using GE AW VolumeShare 5 software. The CT attenuation value was set as −30~−190 HU for the identification of the total fat area. A region of interest (ROI) was outlined from the medial border of the rectus abdominis to the lateral margin of the psoas maximus and the medial border of the obliquus internus abdominis. The area within the ROI was calculated as the VFA, and the area of fat beyond the ROI was calculated as the subcutaneous fat area (SFA) (Figure 1). The VSR was calculated by dividing the VFA by the SFA. An experienced radiologist reviewed all of the images and calculated the VFA and SFA values in blinded fashion. According to the Chinese Overweight/Obesity Medical Nutrition Treatment Expert Consensus, BMI, which is the most useful population-level measure of overweight and obesity, was set at 28 kg/m2 for obesity in all adults.
STATISTICAL ANALYSIS:
Statistical Product and Service Solutions (SPSS) software v.22.0 (IBM Inc., Armonk, NY, USA) was used for data processing. Anthropometric variables were evaluated as continuous variables. Continuous variables are expressed as the median (interquartile range IQR) and evaluated by Mann-Whitney U test or ANOVA; Spearman’s rank or Kendall’s tau-b correlation coefficient were used to evaluate ordinal variables. As appropriate, Pearson’s chi-squared, or Fisher’s exact test were used to evaluate categorical variables.
Results
DEMOGRAPHICS AND CLINICAL FEATURES:
The records of a total of 191 consecutive patients were considered, and 129 of them fulfilled the inclusion and exclusion criteria for the study (Figure 2). The characteristics of the enrolled patients are given in Table 1. The median age of patients was 66 years old (IQR, 60–73.5 years), and 59 (45.7%) patients were female. The median BMI was 23.8 kg/m2 (IQR, 21.7–26.0kg/m2). 60 (46.5%) and 64 (49.6%) patients were diagnosed with anemia (Hb <120g/L) and hypoalbuminemia (Alb <30 g/L), respectively. The cancers AJCC staging was: stage I n=18 (14.0%); stage II n=53 (41.1%); stage III n=58 (44.9%). There were 81 (62.8%) patients diagnosed with colon cancer and who underwent laparoscopic elective colon resection. There were 48 (37.2%) patients diagnosed with rectal cancer and all of these underwent laparoscopic rectal anterior resection.
ANTHROPOMETRIC RESULTS:
The median VFA was 121.7 cm2 (IQR, 83.7–159.6 cm2), median SFA 194.8 cm2 (IQR, 149.8–254.8 cm2), median VSR 0.63 (IQR, 0.48–0.78 cm2). There was a significant correlation between BMI and VFA, SFA (P<0.001). Surgical time was significantly correlated with VFA and VSR (p=0.004; p=0.025). Collinearity of patient characteristics and obesity indexes are shown in Table 2.
POSTOPERATIVE COMPLICATIONS:
Thirty-three patients (25.6%) developed 30-day postoperative complications. Complications included wound infection (n=18), intra-abdominal infection (n=8), pulmonary infection (n=5), intestinal obstruction (n=5), and anastomotic leakage (n=8). Regression analysis (Table 3) showed that higher VFA and VSR and longer surgical time were associated with an increased risk of postoperative complications (P=0.016, P=0.006, P=0.002, respectively). In multivariable analysis, VSR remained associated with increased risk of postoperative complications (P=0.032, OR 6.103, 95% CI 1.173–31.748). ROC analysis was used to evaluate the accuracy of VSR in predicting postoperative complications. The area under the curve (AUC) was 0.650. The cutoff value is VSR ≥0.707, which was associated with 60% sensitivity and 29% specificity for 30-day postoperative complications (Figure 3). In an unadjusted analysis, patients with VSR ≥0.707 had 41.7% risk of incidence, whereas those with VSR <0.707 had 16.0% risk (P=0.001) (Figure 4).
Discussion
The usefulness of a number of anthropometric parameters for the prediction of the surgical outcomes of laparoscopic CRC surgery has been assessed in several countries. It is reasonable to suppose that obesity influences the success of abdominal surgery, and indeed almost all of the previous reports have concluded that VFA is a more sensitive index than BMI and other parameters. At present, the mean annual increase in the incidence of central obesity in China is 1.1%, which is significantly higher than that of non-specific overweight/obesity. Furthermore, the incidence of and mortality associated with CRC also shows clear upward trends. However, previous studies that have evaluated the usefulness of VFA or VSR for the prediction of the success of abdominal surgery in China have almost always used the Western cutoff values, despite the differences between East and West with regard to physical fitness, and the consequent mis-grouping of participants may have led to inappropriate findings.
Identifying patients with increased risk of postoperative complications facilitates making perioperative decisions. In contrast to ASA class, comorbidity, and other factors, obesity may influence the outcomes through its impact on the difficulty of surgery and the physiological system effect [6,7]. Numerous studies have shown that it does not reflect the extent of adipose tissue deposition around the viscera or the risk of postoperative complications, although BMI is widely used for the clinical assessment of obesity. Currently, VFA seems to be the most useful index for the assessment of surgical risk associated with obesity. Kuritzkes et al [8] concluded that VFA, rather than BMI, predicts the incidence of postoperative complications of colon cancer elective surgery. Furthermore, a single-center study conducted in Japan demonstrated that high VFA is an independent risk factor for incisional hernia [12]. However, visceral obesity can also be assessed using other anthropometric measures. Chen et al [13] quantified VFA and the total abdominal muscle area, alongside muscle strength and physical performance, and showed that a combination of visceral obesity and sarcopenia is associated with a higher incidence of postoperative complications, longer hospital stays, and higher hospitalization costs after surgery for CRC.
Some researchers have suggested that perirenal fat area is a risk factor for perioperative and short-term postoperative complications in elective colon cancer surgery [14]. Other anthropometric measures, such as body surface area, mesorectal fat ratio, pelvic fat area, pelvic fat ratio, and VFA-to-muscle index, have also been discussed. However, which is the most useful anthropometric measure remains a matter of controversy. Recent studies have shown that VSR may be a more accurate predictor of cardiovascular and metabolic disease incidence than VFA, but to date there have been few assessments of the use of VSR for the prediction of complications associated with radical laparoscopic colorectal surgery. In the present study, we have compared BMI, VFA, and VSR, and found that VSR is superior to the other indexes, including VFA, for the prediction of postoperative complications. The explanation for this may be that VSR most closely reflects adipose tissue distribution, and VSR increases the difficulty of surgery and thus leads to an increased incidence of complications. Many previous studies have shown that visceral fat mass is strongly associated with the risks of metabolic and cardiovascular disease, whereas subcutaneous fat is relatively benign [15]. High VSR may imply both greater visceral adiposity and less subcutaneous adiposity; therefore, the risk of postoperative complications is higher than with high VFA alone.
In the present study, we aimed to demonstrate that VSR is a suitable measurement for the prediction of the risk of postoperative complications following laparoscopic colorectal cancer, and to identify the most appropriate cutoff value for VSR. We found that as VSR increased, the incidence of postoperative complications also increased. The VSR values were associated with larger AUC areas than were VFA and BMI values. In addition, we have shown, using the ROC curves, that the appropriate cutoff value of VSR for the prediction of the risk of postoperative complications is 0.707.
There were some limitations to the present study. First, there were few participants, and the number of patients with colon cancer and rectal cancer was significantly different. Second, this was a retrospective case study and single-center study. Patients with missing medical records were excluded and the difficulty of surgery varies with the location of the tumor, which may have affected the results to a certain extent. For example, the complication rate of colon cancer (23/81) was higher than that of rectal cancer (10/48). However, we believe that the outcomes are meaningful. In recent years, a study [16] concluded that VSR is the optimal obesity index for predicting stage I–III middle and low rectal cancer recurrence. At present, there is still a lack of sufficient data to prove the relationship. Therefore, multicenter studies with long-term follow-up are needed.
Conclusions
VSR is a potential predictor of postoperative complications in laparoscopic surgery of CRC. Measurement of VSR and identifying patients with increased risk of postoperative complications facilitate making perioperative decisions.
Figures
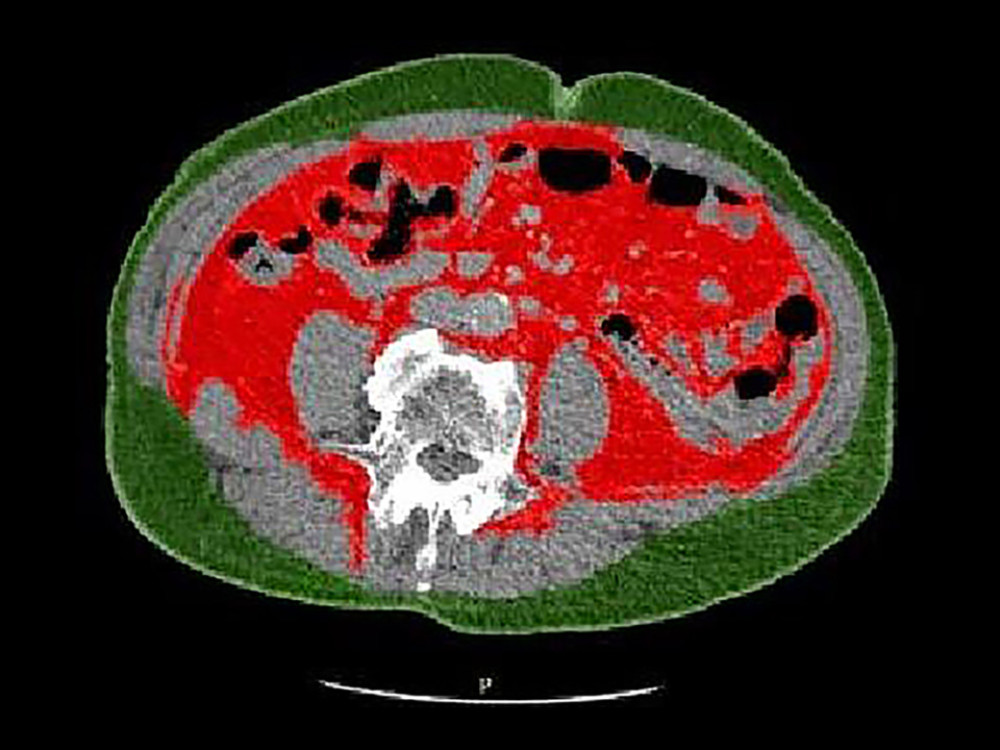 Figure 1. A representative image taken at the level of the L4/L5 intervertebral space, showing computer-derived SFA (green) and VFA (red).
Figure 1. A representative image taken at the level of the L4/L5 intervertebral space, showing computer-derived SFA (green) and VFA (red). 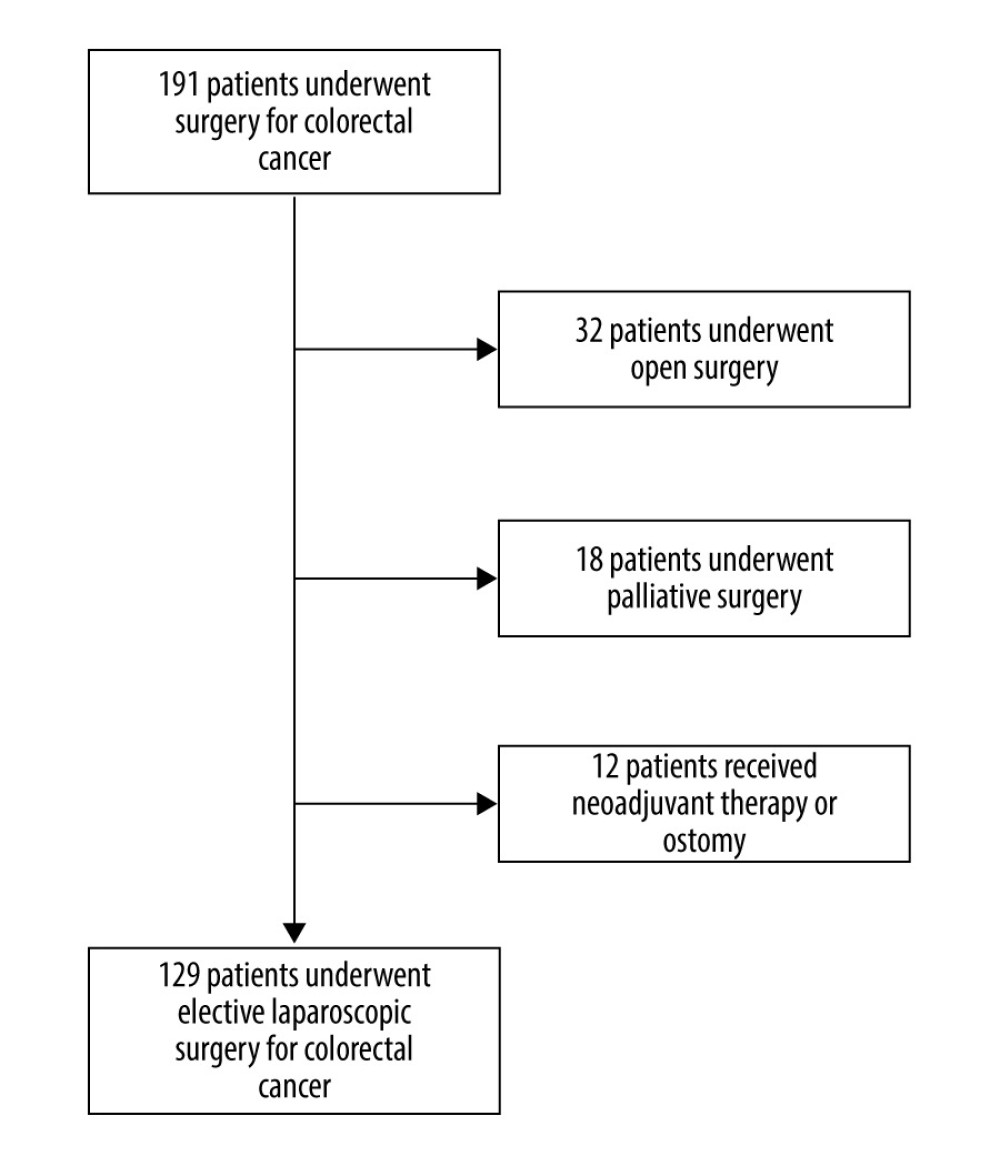 Figure 2. Flowchart of exclusion criteria to arrive at final cohort.
Figure 2. Flowchart of exclusion criteria to arrive at final cohort. 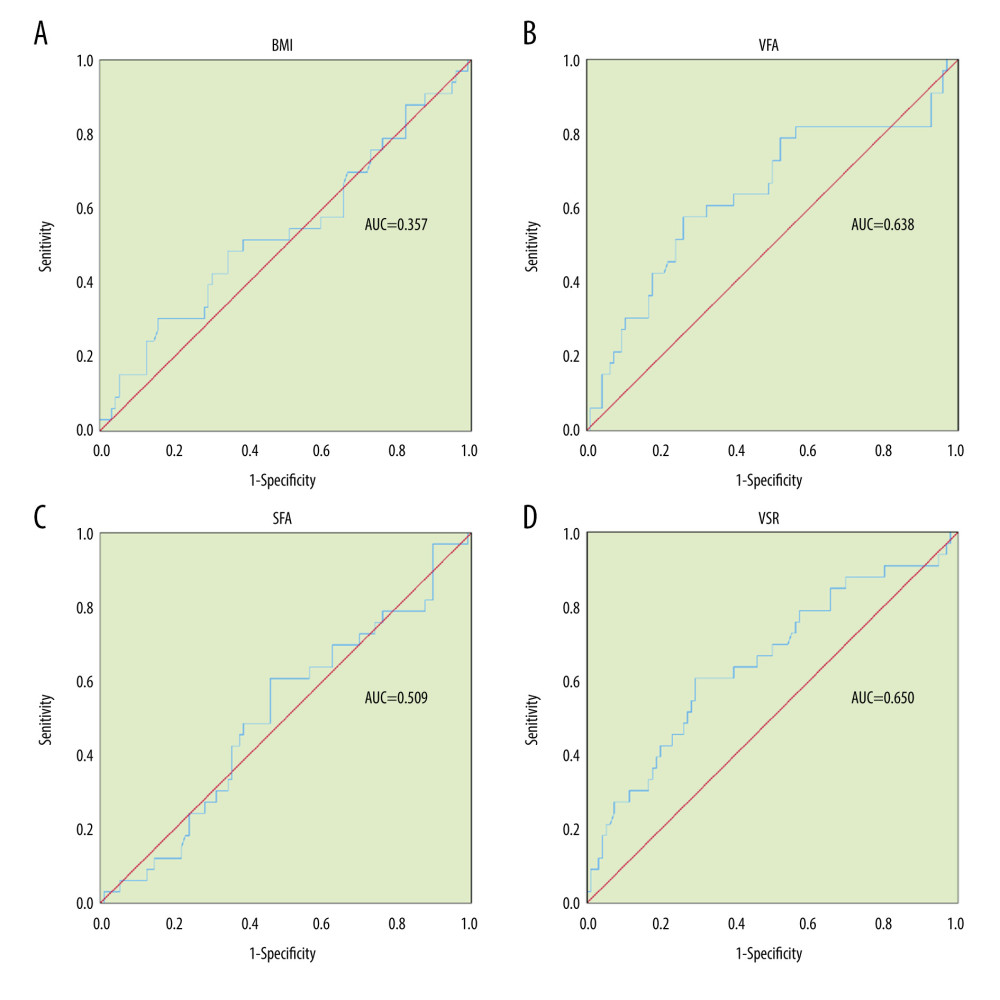 Figure 3. (A–D) ROC curves showing the accuracy of anthropometric measurement in predicting postoperative complications.
Figure 3. (A–D) ROC curves showing the accuracy of anthropometric measurement in predicting postoperative complications. 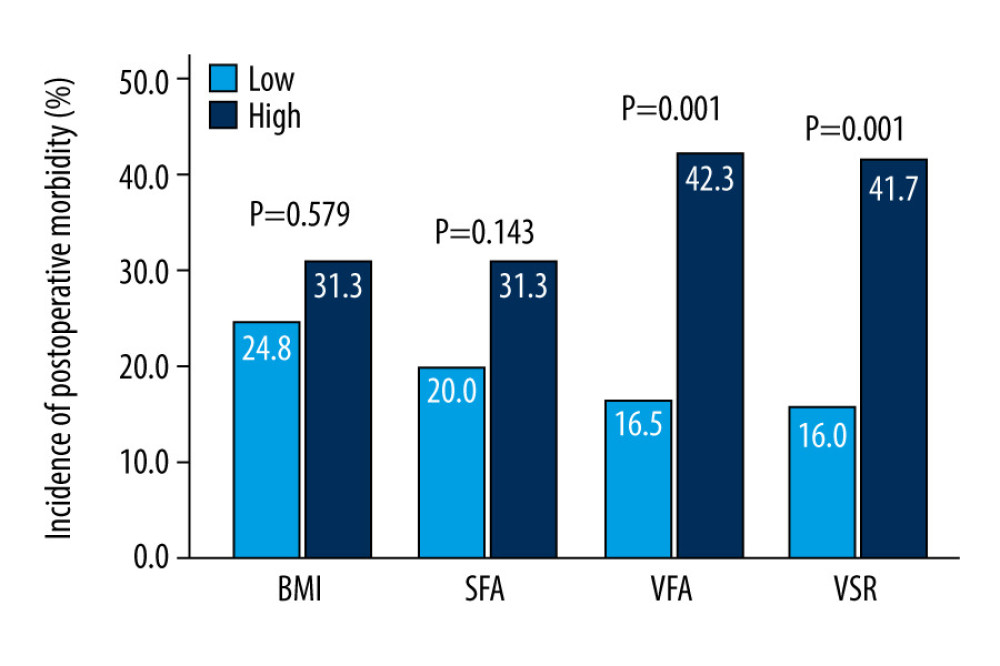 Figure 4. Comparison of anthropometric measurement in predicting postoperative complication. * Unadjusted P values, Pearson chi-squared test.
Figure 4. Comparison of anthropometric measurement in predicting postoperative complication. * Unadjusted P values, Pearson chi-squared test. References
1. Hendren S, Birkmeyer JD, Yin H, Surgical complications are associated with omission of chemotherapy for stage III colorectal cancer: Dis Colon Rectum, 2010; 53; 1587-93
2. Merkow RP, Bentrem DJ, Mulcahy MF, Effect of postoperative complications on adjuvant chemotherapy use for stage III colon cancer: Ann Surg, 2013; 258(6); 847-53
3. Eberhardt JM, Kiran RP, Lavery IC, The impact of anastomotic leak and intra-abdominal abscess on cancer-related outcomes after resection for colorectal cancer: A case control study: Dis Colon Rectum, 2009; 52(3); 380-86
4. Bardou M, Barkun AN, Martel M, Obesity and colorectal cancer: Gut, 2013; 62(6); 933-47
5. Bickenbach KA, Denton B, Gonen M, Impact of obesity on perioperative complications and long-term survival of patients with gastric cancer: Ann Surg Oncol, 2013; 20(3); 780-87
6. Aytac E, Lavery IC, Kalady MF, Impact of obesity on operation performed, complications, and long-term outcomes in terms of restoration of intestinal continuity for patients with mid and low rectal cancer: Dis Colon Rectum, 2013; 56(6); 689-97
7. Gendall KA, Raniga S, Kennedy R, The impact of obesity on outcome after major colorectal surgery: Dis Colon Rectum, 2007; 50(12); 2223-37
8. Kuritzkes BA, Pappou EP, Kiran RP, Visceral fat area, not body mass index, predicts postoperative 30-day morbidity in patients undergoing colon resection for cancer: Int J Colorectal Dis, 2018; 33(8); 1019-28
9. Kwon S, Han AL, The correlation between the ratio of visceral fat area to subcutaneous fat area on computed tomography and lipid accumulation product as indexes of cardiovascular risk: J Obes Metab Syndr, 2019; 28(3); 186-93
10. Graffy PM, Pickhardt PJ, Quantification of hepatic and visceral fat by CT and MR imaging: Relevance to the obesity epidemic, metabolic syndrome and NAFLD: Br J Radiol, 2016; 89(1062); 20151024
11. Shuster A, Patlas M, Pinthus JH, The clinical importance of visceral adiposity: A critical review of methods for visceral adipose tissue analysis: Br J Radiol, 2012; 85(1009); 1-10
12. Yamamoto M, Takakura Y, Ikeda S, Visceral obesity is a significant risk factor for incisional hernia after laparoscopic colorectal surgery: A single-center review: Asian J Endosc Surg, 2018; 11(4); 373-77
13. Chen WZ, Chen XD, Ma LL, Impact of visceral obesity and sarcopenia on short-term outcomes after colorectal cancer surgery: Dig Dis Sci, 2018; 63(6); 1620-30
14. der Hagopian O, Dahlberg M, Heinius G, Perirenal fat surface area as a risk factor for perioperative difficulties and 30-day postoperative complications in elective colon cancer surgery: Colorectal Dis, 2018; 20(12); 1078-87
15. Chen B, Zhang Y, Zhao S, The impact of general/visceral obesity on completion of mesorectum and perioperative outcomes of laparoscopic TME for rectal cancer: A STARD-compliant article: Medicine (Baltimore), 2016; 95(36); e4462
16. Lee KH, Kang BK, Ahn BK, Higher visceral fat area/subcutaneous fat area ratio measured by computed tomography is associated with recurrence and poor survival in patients with mid and low rectal cancers: Int J Colorectal Dis, 2018; 33(9); 1303-7
Figures
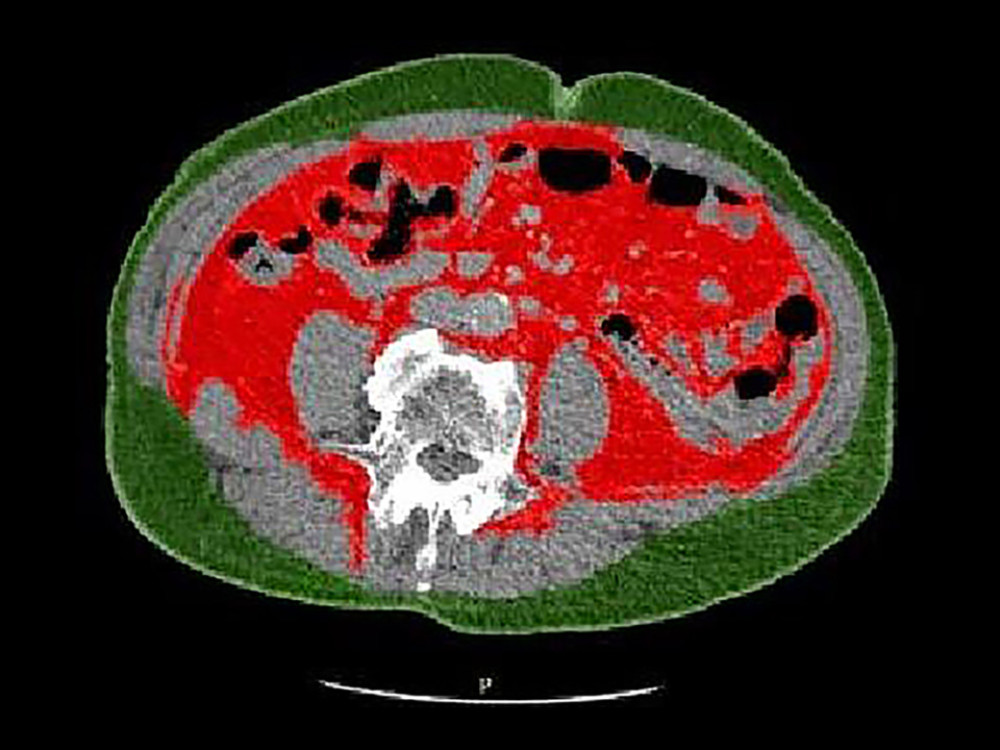 Figure 1. A representative image taken at the level of the L4/L5 intervertebral space, showing computer-derived SFA (green) and VFA (red).
Figure 1. A representative image taken at the level of the L4/L5 intervertebral space, showing computer-derived SFA (green) and VFA (red).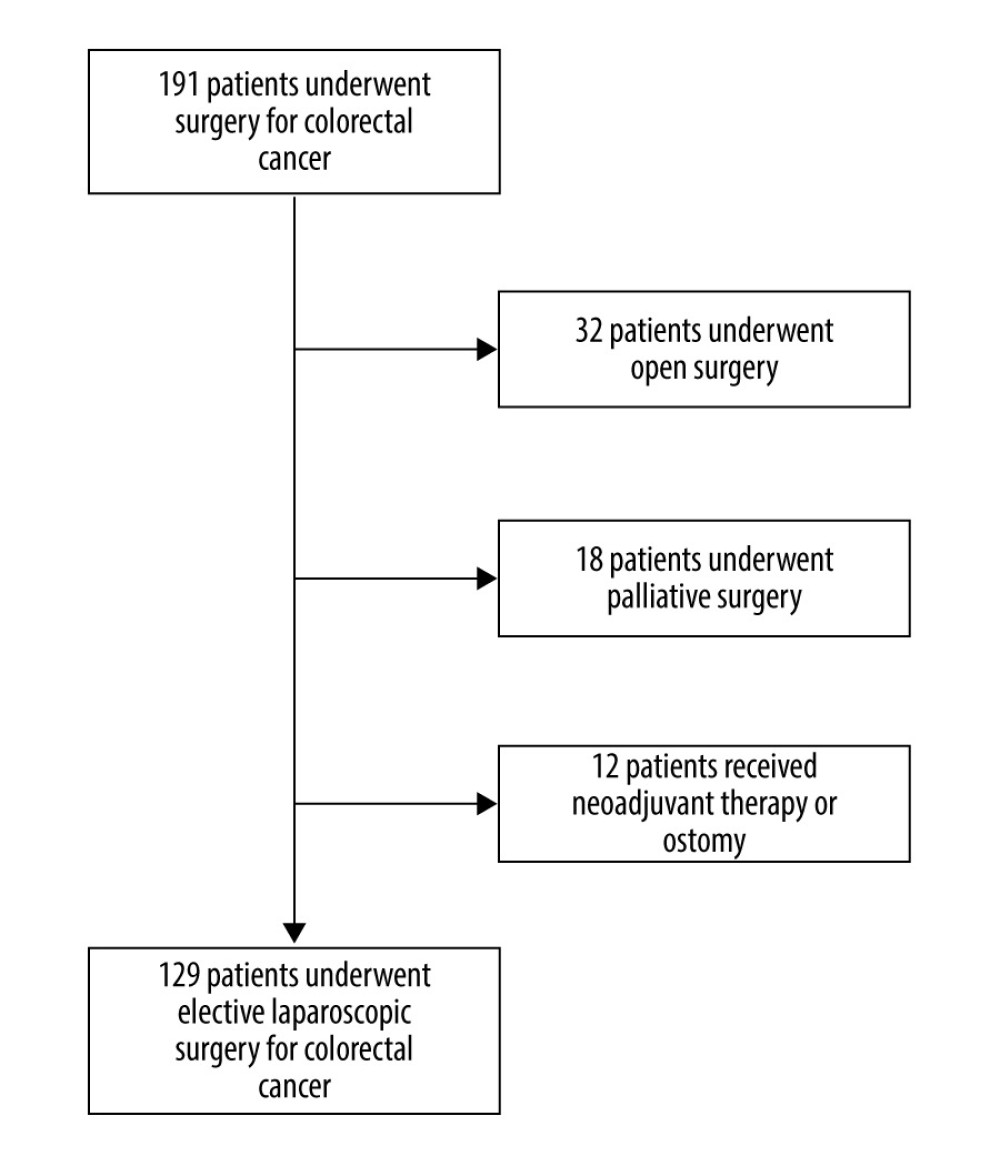 Figure 2. Flowchart of exclusion criteria to arrive at final cohort.
Figure 2. Flowchart of exclusion criteria to arrive at final cohort.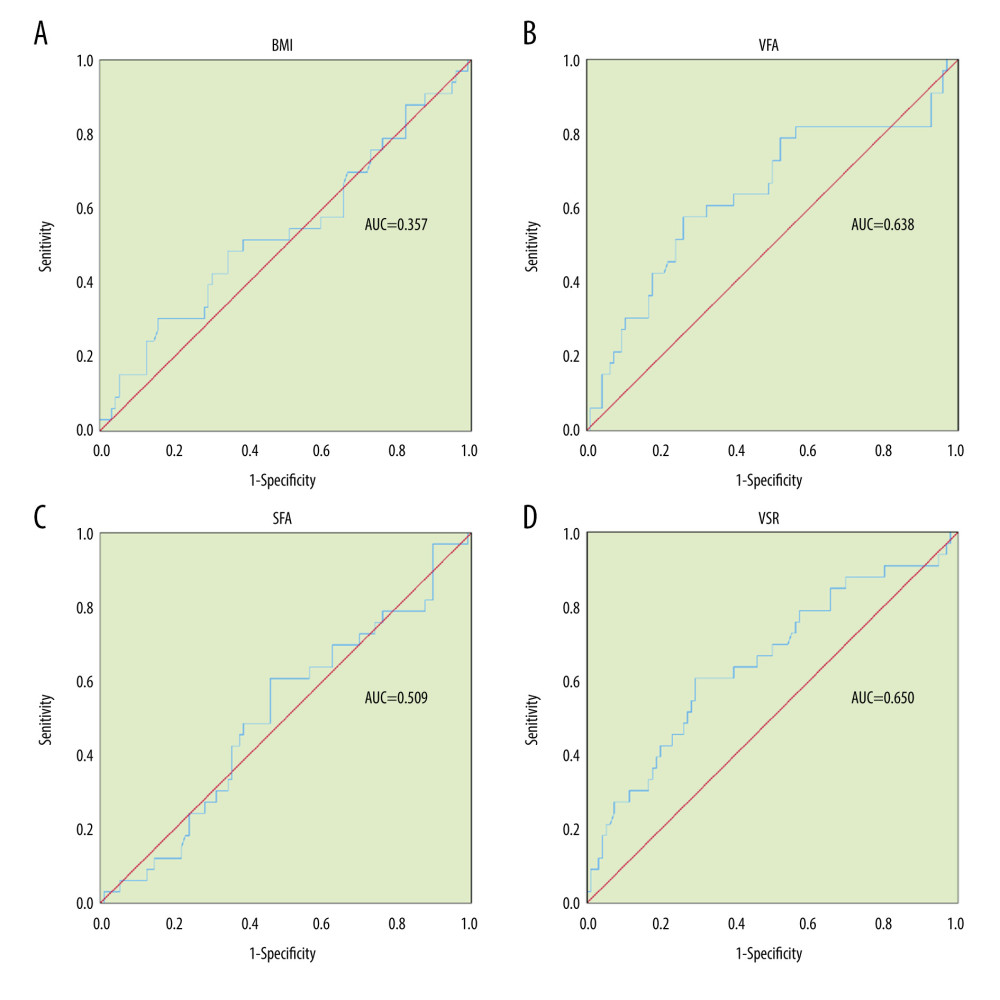 Figure 3. (A–D) ROC curves showing the accuracy of anthropometric measurement in predicting postoperative complications.
Figure 3. (A–D) ROC curves showing the accuracy of anthropometric measurement in predicting postoperative complications.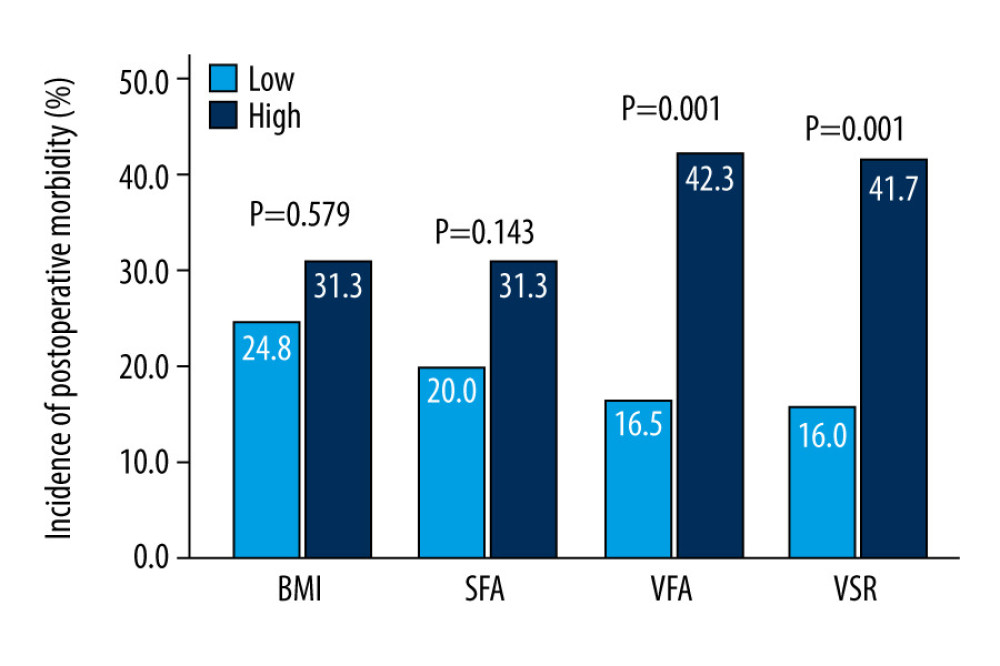 Figure 4. Comparison of anthropometric measurement in predicting postoperative complication. * Unadjusted P values, Pearson chi-squared test.
Figure 4. Comparison of anthropometric measurement in predicting postoperative complication. * Unadjusted P values, Pearson chi-squared test. Tables
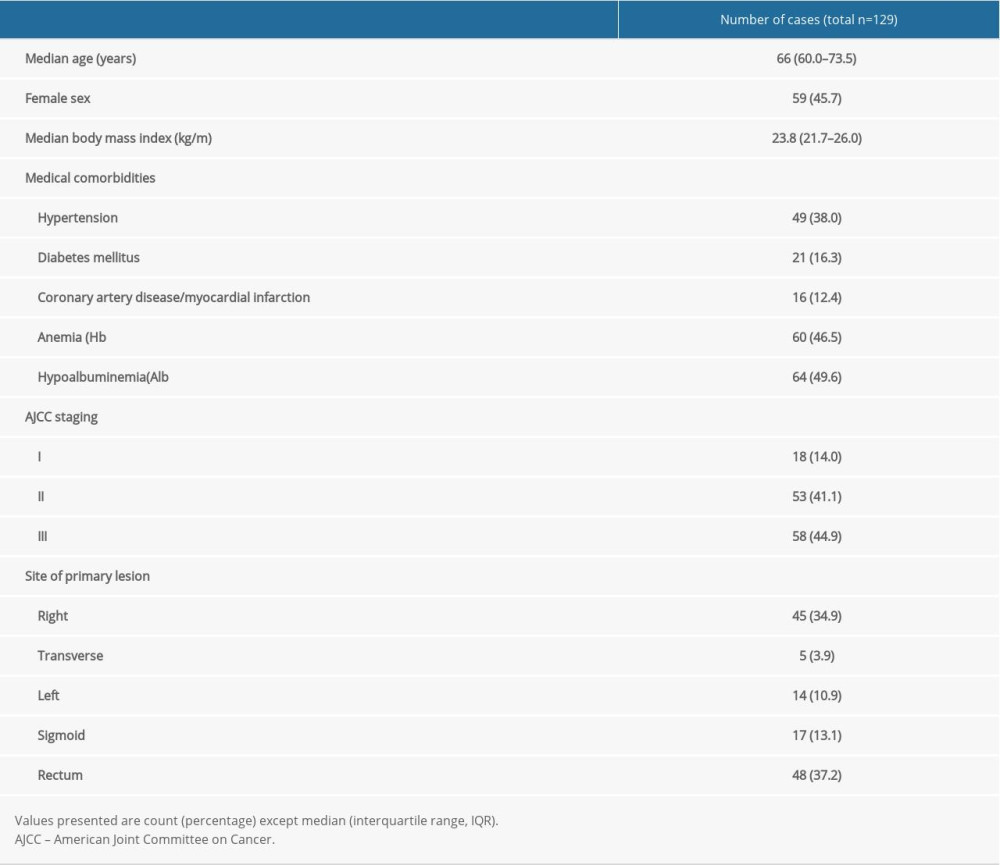 Table 1. Patient baseline characteristics.
Table 1. Patient baseline characteristics.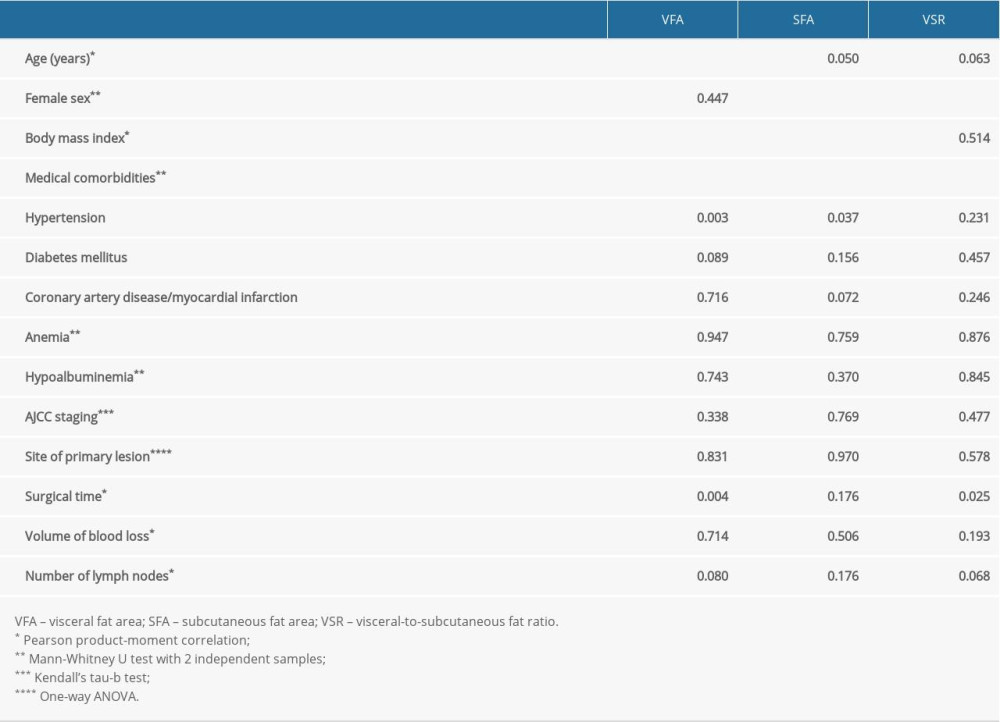 Table 2. Degree of collinearity between patient baseline characteristics and CT-derived anthropometries.
Table 2. Degree of collinearity between patient baseline characteristics and CT-derived anthropometries.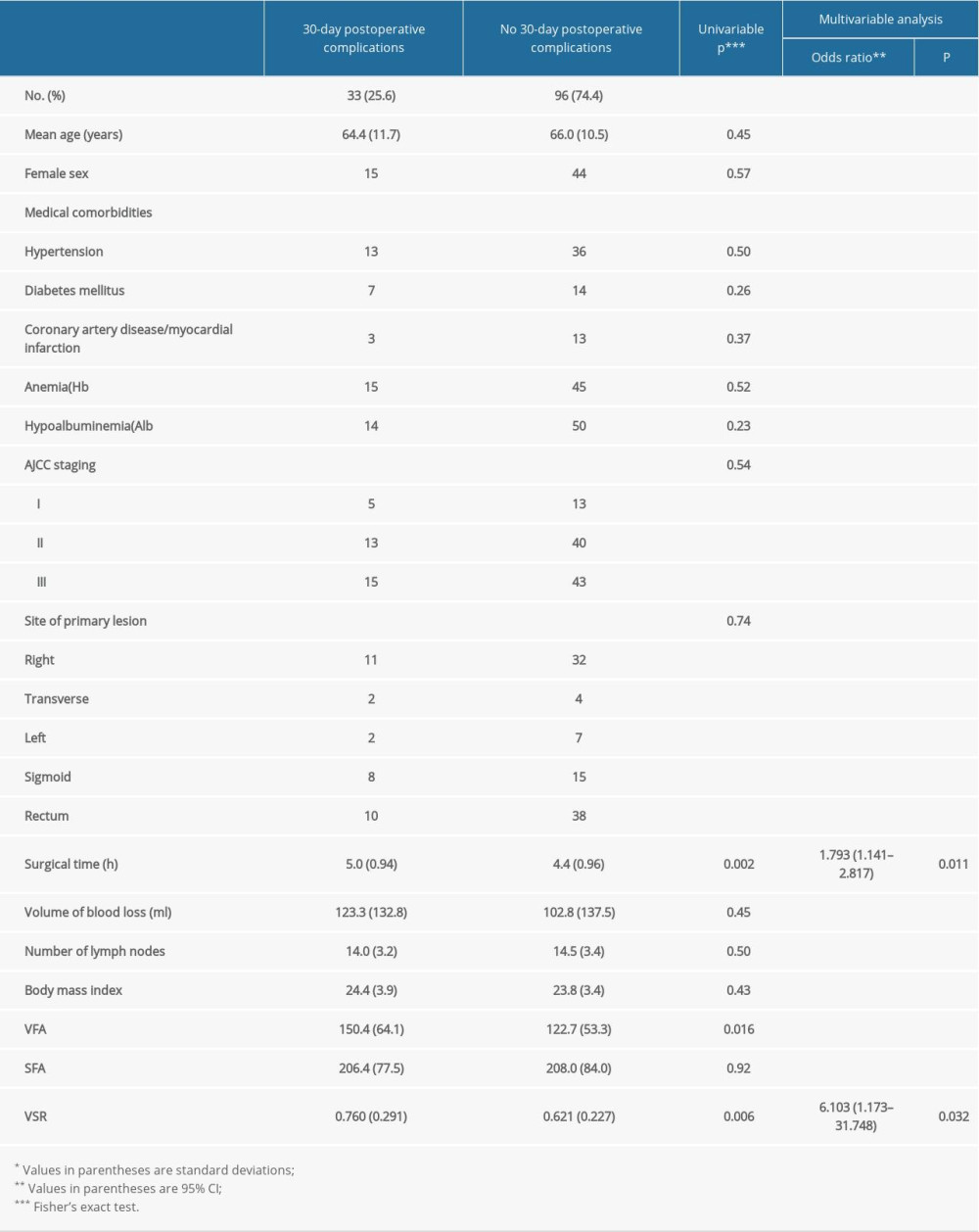 Table 3. Univariable and multivariable analysis of 30-day postoperative complications.
Table 3. Univariable and multivariable analysis of 30-day postoperative complications.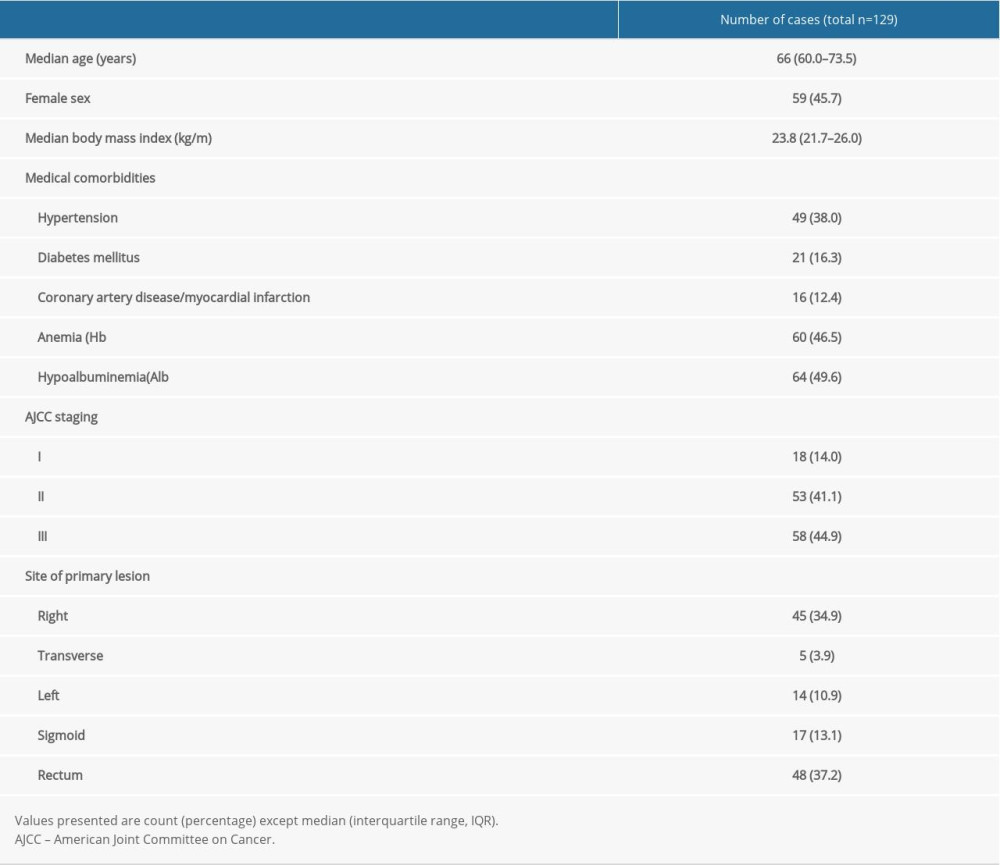 Table 1. Patient baseline characteristics.
Table 1. Patient baseline characteristics.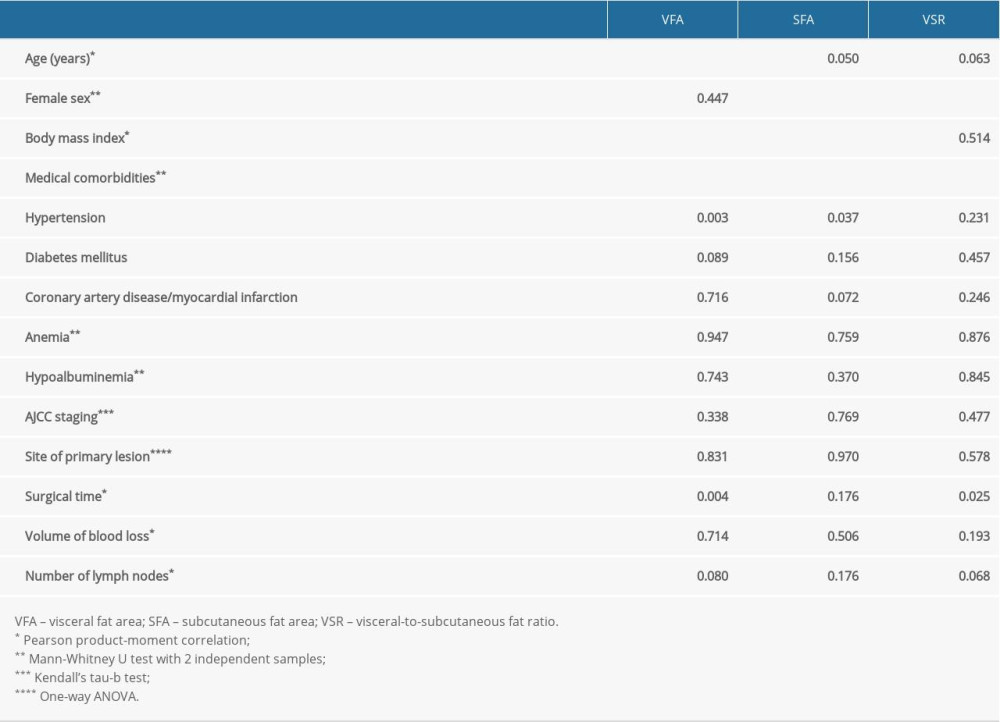 Table 2. Degree of collinearity between patient baseline characteristics and CT-derived anthropometries.
Table 2. Degree of collinearity between patient baseline characteristics and CT-derived anthropometries.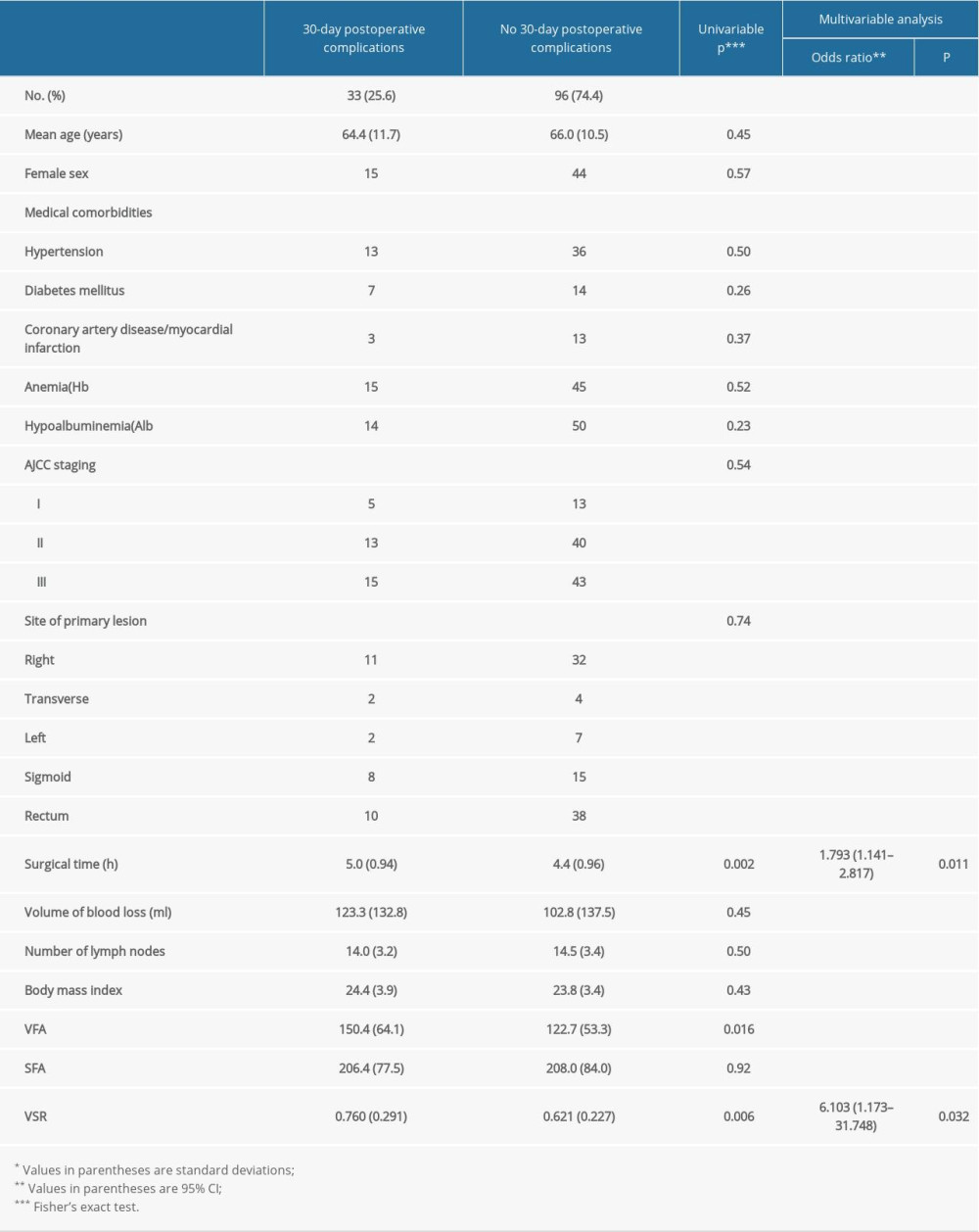 Table 3. Univariable and multivariable analysis of 30-day postoperative complications.
Table 3. Univariable and multivariable analysis of 30-day postoperative complications. In Press
05 Mar 2024 : Clinical Research
Muscular Function Recovery from General Anesthesia in 132 Patients Undergoing Surgery with Acceleromyograph...Med Sci Monit In Press; DOI: 10.12659/MSM.942780
05 Mar 2024 : Clinical Research
Effects of Thermal Insulation on Recovery and Comfort of Patients Undergoing Holmium Laser LithotripsyMed Sci Monit In Press; DOI: 10.12659/MSM.942836
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








