09 November 2021: Clinical Research
Association Between Severe Chronic Obstructive Pulmonary Disease and Polyneuropathy
Ahmet Arisoy1ABCDEF*, Abdullah Yilgor2BCD, İbrahim H. Uney1BCDOI: 10.12659/MSM.932690
Med Sci Monit 2021; 27:e932690
Abstract
BACKGROUND: Chronic obstructive pulmonary disease (COPD) is a life-threatening and devastating disease associated with low-grade systemic inflammation. In adults, the most common disease of the peripheral nervous system is peripheral neuropathy. While most polyneuropathy has a mixed presentation, some cases are motor dominant and others are sensory dominant. We investigated polyneuropathy in patients with COPD and hypothesized that low-grade systemic inflammation and other pathologies in patients with COPD cause peripheral axonal polyneuropathy.
MATERIAL AND METHODS: We included 62 patients with COPD without any neurological signs or symptoms, and 30 healthy volunteers with no known neurological or pulmonary diseases as controls. There were 38 men in the COPD group and 17 men in the control group; the mean ages of the 2 groups were 64.88 and 62.7 years, respectively. According to the Global Initiative for Chronic Obstructive Lung Disease COPD report, all COPD patients were group D. After collecting demographic and clinical characteristics of the participants, we performed an electrophysiological examination to investigate polyneuropathy and pulmonary function test results. C-reactive protein, hemoglobin, creatinine, partial carbon dioxide pressure (pCO₂) levels were recorded. Electrophysiological examination was performed with a Medelec Synergy device using standard neurographic procedures, and the results were assessed.
RESULTS: Significant differences were found for forced expiratory volume in 1 sec (FEV1), %FEV1, forced vital capacity (FVC), %FVC, pCO₂, and hemoglobin and creatinine levels, but all participants had a creatinine level within the normal range. There was no difference in sensory neuropathy between the groups, but a significant difference was found in terms of motor neuropathy.
CONCLUSIONS: As noted in previous studies, systemic inflammation, increased oxidative stress, decreased oxygen pressure, and multiple comorbidities in patients with COPD may all contribute to the development of neuropathy.
Keywords: Inflammation, Polyneuropathies, Pulmonary Disease, Chronic Obstructive, Respiratory Function Tests, Female, Humans, Male
Background
Chronic obstructive pulmonary disease (COPD) is an important health problem and one of the leading causes of death in the world. Airway and/or alveolar abnormalities in patients with COPD are usually caused by significant exposure to noxious gases and particles [1]. This exposure produces characteristic changes, including chronic inflammation and structural changes. The inflammation involves specific inflammatory cell types and almost the entire lung. There is growing evidence that low-grade systemic inflammation plays a role in COPD and comorbid conditions [2].
Peripheral neuropathy is a common neurological condition [3]. While most polyneuropathy has a mixed presentation, some cases are motor dominant and others are sensory dominant. Damage to the nerves has a range of causes, including genetic and metabolic factors, autoimmune disorders, infection, drug or environmental toxicity, and malignancy [4].
The question of causal links between peripheral neuropathy and COPD is complex because neuropathy, like COPD, is age related. The effects of premature aging have been demonstrated in mouse models. Premature aging is also considered to be an important factor in the development of COPD. The association between peripheral neuropathy and COPD has been explained by the deleterious effects of chronic hypoxemia on peripheral nerves as well as systemic inflammation. A common risk factor for COPD and neuropathy is smoking, which includes exposure to a variety of adverse compounds [5].
We hypothesized that systemic inflammation and oxidative/antioxidative imbalance in patients with COPD cause polyneuropathy, but this polyneuropathy is usually not studied. In this study we investigated peripheral neuropathy in COPD cases with no clinical evidence of neuropathy.
Material and Methods
SUBJECTS AND STUDY DESIGN:
Exclusion criteria included known neurological diseases, continuous corticosteroid use, cervical disc hernia, diabetes mellitus, renal disease, heart failure, connective tissue disease, alcohol abuse, and malignancy. A detailed neurological and physical examination was performed for each participant.
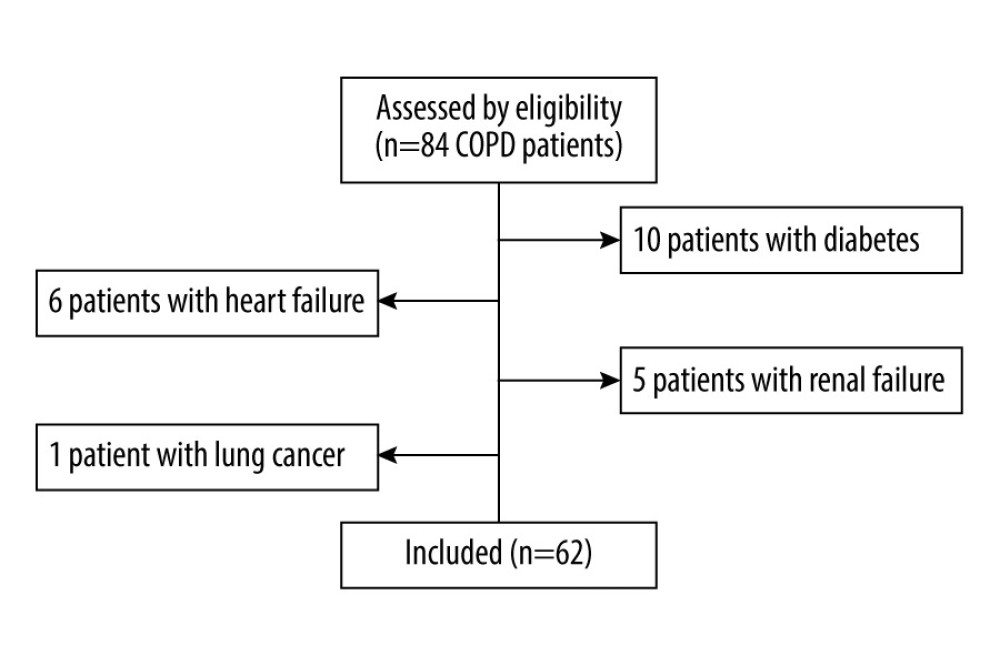
Eighty-four patients with COPD who were hospitalized in the pulmonary disease clinic or who visited the outpatient clinic were selected for the study. Among these patients, 10 patients with diabetes, 6 patients with heart failure, 5 patients with renal failure, and 1 patient with cancer were excluded from the study. The flow chart in Figure 1 shows the participants’ progress through the study. We continued the study with 62 patients with COPD. None of the participants had any known diagnosed or treated peripheral neurological deficits or neuropathies.
EXPERIMENTAL PROCEDURES:
The post-bronchodilator forced expiratory volume in 1 sec/forced vital capacity (FEV1/FVC) values of all COPD patients were <0.7, in keeping with the 2021 Global Initiative for Chronic Obstructive Lung Disease (GOLD) COPD guidelines. The participants were classified in group D of the GOLD guidelines: their GOLD grades were 2 in 10 cases, 3 in 25 cases, and 4 in 27 cases. All participants with COPD had a history of hospitalization or for 2 COPD exacerbations in the last year, and their Modified Medical Research Council score was >1. Thirty healthy volunteers with no neurological or pulmonary diseases were included as controls. Age, sex, C-reactive protein (CRP) level, hemoglobin level, creatinine level, smoking status, partial carbon dioxide pressure (pCO2) level, pulmonary function test results, and electromyography (EMG) results were all recorded. The EMG and pulmonary function test were performed in the COPD group before discharge after any acute exacerbation had resolved.
After neurological examination, electrophysiological examination was performed with a Medelec Synergy device (Oxford Instruments, Surrey, England) using standard neurographic procedures, and the results were assessed according to the American Diabetes Association Diabetic Neuropathy Guidelines [6]. The room temperature was 22–24°C and the temperature of the participants’ extremities was 34°C; the participants’ extremities were heated when necessary. Nerve conduction tests were performed in 2 motor and 2 sensory nerves (median and ulnar nerves) in the upper extremities and in 2 motor (tibial and common peroneal nerves) and 2 sensory nerves (sural and peroneal sensory nerves) in the lower extremities. Nerve conduction velocity was measured using the orthodromic method, and nerve conduction was evaluated at supramaximal intensity to obtain the highest amplitude. Axonal pathology and demyelination in nerves were defined as decreased sensory/motor nerve action potential amplitude and decreased sensory/motor nerve conduction velocity. Polyneuropathy was defined as the presence of 2 or more abnormalities detected in the electrophysiological examination.
STATISTICAL ANALYSIS:
Descriptive statistics for the continuous variables included mean, standard deviation, and range. Categorical variables are expressed as numbers and percentages. One-way analysis of variance was used to compare the group means of continuous variables, and Duncan’s multiple-comparison test was used to detect differences between the groups. Pearson’s correlation coefficient analysis was performed separately in the groups to determine the relationship between these variables. The chi-square test was used to determine the relationship between groups and the categorical variables. A
Results
Sixty-two COPD patients and 30 healthy participants were included in this study. There were 24 women in the COPD group and 13 women in the control group; the mean ages of the 2 groups were 64.88±8.62 and 62.7±9.65 years, respectively (
Only one participant (3.3%) in the control group had sensory and motor polyneuropathy, whereas 27 participants (44%) in the COPD group had sensory and 36 (58%) participants had motor polyneuropathy. No significant difference was observed between groups in the frequency of sensory polyneuropathy, but there was a significant difference in motor polyneuropathy between the groups (chi-square for sensory polyneuropathy 3.78 and
No significant differences were found for latency, amplitude, or velocity of nerve activity in the sensory components of the median and ulnar nerve between the groups. No significant differences were found for latency or amplitude values of the sensory component of the sural and superficial peroneal nerves. A significant difference was found in nerve velocity in the sensory component of the sural and superficial peroneal nerves.
No significant differences were found for latency, amplitude, or velocity values in the motor component of the ulnar, common peroneal, or tibial nerves between the groups. No significant differences were found for latency or amplitude values in the motor component of the median nerve, but there was a significant difference in the velocity of the motor component of the median nerve.
The latency, amplitude, and velocity values of the motor and sensory components of aforementioned nerves are given in Tables 2 and 3.
Pearson’s correlation analyses detected a significant correlation between FEV1/FVC and amplitude values in the motor component of the ulnar nerve (
Discussion
Systemic inflammation in patients with COPD could play a role in multiple comorbid conditions. COPD is characterized by many cell types and inflammatory mediators. In addition, oxidative stress and a protease/antiprotease imbalance are observed in COPD patients [1].
The most common types of polyneuropathies are axonal neuropathies, characterized by insult or degeneration. Action potentials are unable to propagate when the axon is degenerated, and this can be measured using electrophysiological tests [4].
Oxidative stress increases in neurodegenerative diseases such as Alzheimer disease [7,8], and Sifuentes-Franco et al [9] suggested that oxidative stress plays a role in the pathogenesis of polyneuropathy in patients with diabetes. Herder et al [10] reported that painful distal sensorimotor polyneuropathy is linked to systemic subclinical and vascular inflammation in the older population.
Oxidative stress, systemic inflammation, and a protease/antiprotease imbalance are observed in both COPD and polyneuropathy. A few studies have investigated the association between COPD and neuropathy. We investigated polyneuropathy in individuals with severe COPD and compared the results with same-age controls. A significant association was found between COPD and polyneuropathy.
One hypothesized underlying mechanism of polyneuropathy in COPD is chronic hypoxia of the peripheral nervous system [11,12]. Since chronic hypoxia affects patients with more severe COPD, this means that polyneuropathy will mostly affect patients with more severe COPD. One study identified an association between chronic hypoxemia and polyneuropathy in patients with COPD, identifying polyneuropathy in 30 of 151 participants with clinical signs of mild sensory motor and distal neuropathy [13].
Agrawal et al [14] detected neuropathy in 5 of 30 COPD patients. These 5 patients had significantly higher cigarette consumption, longer disease duration, and more advanced airflow obstruction compared with COPD patients without peripheral neuropathy.
Ozge et al [15] investigated the association between COPD and polyneuropathy and detected polyneuropathy in 44.8% of COPD cases. The incidence of neuropathy and the rate of axonal neuropathy were significantly higher in the hypoxemic group than in the normoxemic group. Our participants were all hypoxemic and belonged to group D according to the 2021 GOLD guidelines. Sensory polyneuropathy was detected in 43.5% of our cases, and motor polyneuropathy in 58%.
In contrast to our study, Visser et al [2] found no association between neuropathy and COPD. They prospectively studied 345 patients with cryptogenic axonal polyneuropathy and 465 controls, investigating COPD prevalence in both groups. No association was found between neuropathy and COPD. While they investigated the presence of COPD in polyneuropathy patients in their studies, we investigated the presence of polyneuropathy in COPD patients.
Kahnert et al [5] reported findings on polyneuropathy in patients with COPD in their study evaluating data from the fourth visit of the COSYCONET cohort. They used repeated tuning fork and monofilament testing, unlike our study, to investigate the presence of polyneuropathy in patients with COPD. They identified base excess and ankle-brachial index as major determinants of peripheral neuropathy in patients with COPD. All other associations, particularly those with lung function and physical capacity, were indirect.
One limitation of this study was the small number of participants. Additionally, all COPD patients had at least 1 hospitalization or 2 exacerbations within the last year, and all often used short-term systemic corticosteroids. Both the COPD and control participants were relatively old and had comorbid conditions, and they used multiple drugs. COPD patients are usually immobile because of their disease status. This study did not determine which of the factors mentioned contributed to or caused neuropathy.
Conclusions
In conclusion, a strong association was observed between neuropathy and COPD. As mentioned in previous studies, the patients with COPD had low-grade systemic inflammation, increased oxidative stress, decreased partial oxygen pressure, and multiple comorbid conditions. All these factors may have contributed to the development of neuropathy. Further studies are needed to determine which of the mentioned factors contributed this association.
References
1. Global Initiative for Chronic Obstructive Lung Disease (GOLD), Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease, 2021, GOLD Available from: https://goldcopd.org/wp-content/uploads/2020/11/GOLD-REPORT-2021-v1.1-25Nov20_WMV.pdf
2. Visser NA, Notermans NC, Teding van Berkhout F, Chronic obstructive pulmonary disease is not a risk factor for polyneuropathy: A prospective controlled study: Chron Respir Dis, 2017; 14(4); 327-33
3. Yavuz GO, Yılgör A, Yavuz IH, Effects of omalizumab therapy on peripheral nerve functions: Short observational study: Postepy Dermatol Alergol, 2019; 36(2); 211-16
4. Ramdharry G, Peripheral nerve disease: Handb Clin Neurol, 2018; 159; 403-15
5. Kahnert K, Föhrenbach M, Lucke T, The impact of COPD on polyneuropathy: Results from the German COPD cohort COSYCONET: Respir Res, 2020; 21(1); 28
6. , Report and recommendations of the San Antonio conference on diabetic neuropathy: Ann Neurol, 1988; 24(1); 99-104
7. Zis P, Dickinson M, Shende S, Oxidative stress and memory decline in adults with Down syndrome: Longitudinal study: J Alzheimers Dis, 2012; 31(2); 277-83
8. Zis P, McHugh P, McQuillin A, Memory decline in Down syndrome and its relationship to iPF2alpha, a urinary marker of oxidative stress: PLoS One, 2014; 9(6); e97709
9. Sifuentes-Franco S, Pacheco-Moisés FP, The role of oxidative stress, mitochondrial function, and autophagy in diabetic polyneuropathy: J Diabetes Res, 2017; 2017; 1673081
10. Herder C, Bongaerts BW, Rathmann W, Differential association between biomarkers of subclinical inflammation and painful polyneuropathy: Results from the KORA F4 study: Diabetes Care, 2015; 38(1); 91-96
11. Vila A, Reymond F, Paramelle B, Peripheral neuropathies and chronic respiratory insufficiency: An electrophysiological study: Rev Electroencephalogr Neurophysiol Clin, 1986; 15; 331-40
12. Nowak D, Brüch M, Arnaud F, Peripheral neuropathies in patients with chronic obstructive pulmonary disease: A multicenter prevalence study: Lung, 1990; 168(1); 43-51
13. Pfeiffer G, Kunze K, Brüch M, Polyneuropathy associated with chronic hypoxaemia: Prevalence in patients with chronic obstructive pulmonary disease: J Neurol, 1990; 237(4); 230-33
14. Agrawal D, Vohra R, Gupta PP, Sood S, Subclinical peripheral neuropathy in stable middle-aged patients with chronic obstructive pulmonary disease: Singapore Med J, 2007; 48(10); 887-94
15. Ozge A, Atiş S, Sevim S, Subclinical peripheral neuropathy associated with chronic obstructive pulmonary disease: Electromyogr Clin Neurophysiol, 2001; 41(3); 185-91
Tables
 Table 1. Characteristics of participants.
Table 1. Characteristics of participants.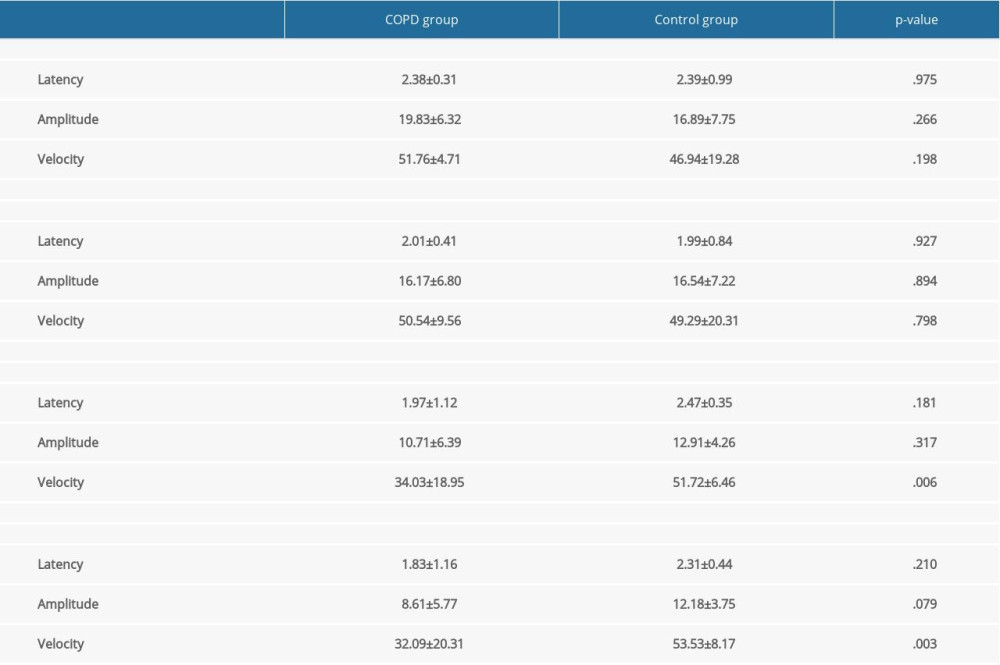 Table 2. Latency, amplitude, and velocity values of the sensory component of the nerves.
Table 2. Latency, amplitude, and velocity values of the sensory component of the nerves.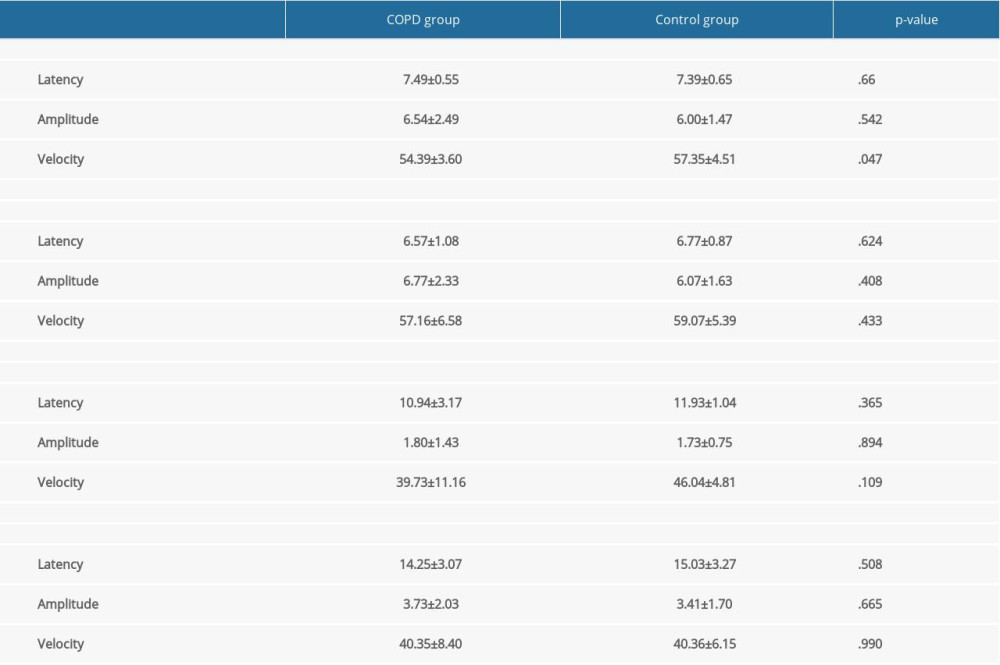 Table 3. Latency, amplitude, and velocity values of the motor component of the nerves.
Table 3. Latency, amplitude, and velocity values of the motor component of the nerves. Table 1. Characteristics of participants.
Table 1. Characteristics of participants.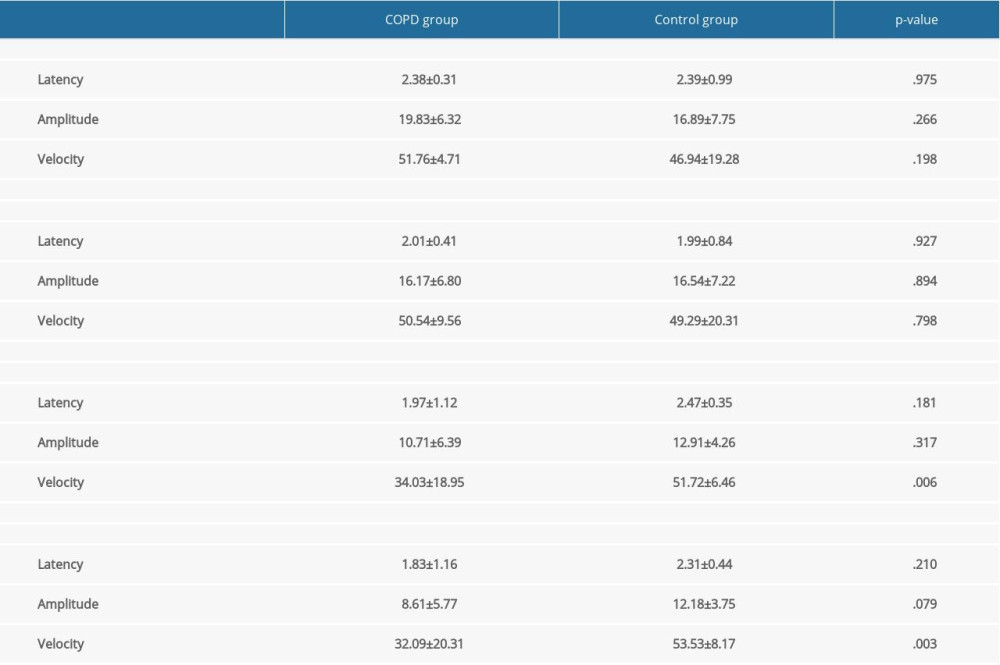 Table 2. Latency, amplitude, and velocity values of the sensory component of the nerves.
Table 2. Latency, amplitude, and velocity values of the sensory component of the nerves.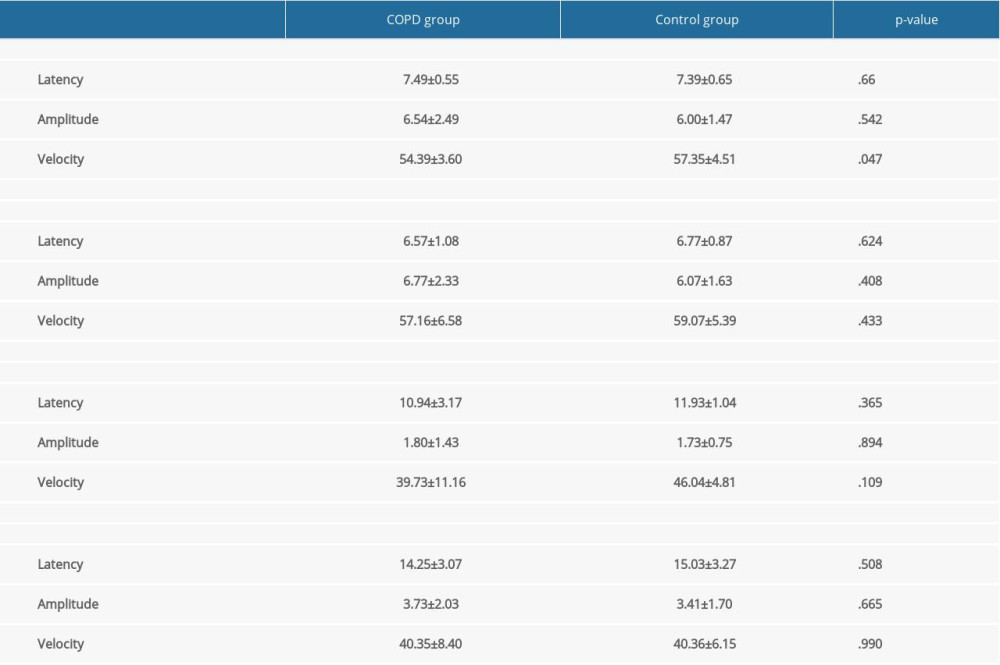 Table 3. Latency, amplitude, and velocity values of the motor component of the nerves.
Table 3. Latency, amplitude, and velocity values of the motor component of the nerves. In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952