02 August 2020: Articles 
Hepatic Hydatid Cyst Misdiagnosed as Simple Cyst: A Case Report
Unusual clinical course, Mistake in diagnosis, Unusual or unexpected effect of treatment, Diagnostic / therapeutic accidents, Unexpected drug reaction, Educational Purpose (only if useful for a systematic review or synthesis)
Yan Xu1EF, Xiaoling Hu2F, Jiangbin Li1F, Rui Dong1AD*DOI: 10.12659/AJCR.923281
Am J Case Rep 2020; 21:e923281
Abstract
BACKGROUND: Hepatic hydatid cysts is a cystic disease of the liver caused by echinococcosis. Echinococcosis usually forms a monolocular cyst and causes space occupying effect, while alveolar echinococcosis often progresses into a polycystic mass that dilates into the adjacent liver parenchyma, with different clinical manifestations. In clinical practice, hepatic hydatid cyst and simple cyst are generally diagnosed clearly, but there are still misdiagnosed cases.
CASE REPORT: A 40-year-old female patient with no symptoms had a computed tomography and magnetic resonance imaging examination that revealed multiple round-like shadows of varying sizes in her liver. Combined with the laboratory and imaging results, the diagnosis was considered as hepatic hemangioma and hepatic cyst. Therefore, we planned to perform ultrasound guided microwave ablation of hepatic hemangioma and laparoscopic fenestration of hepatic cyst. Considering the possibility of hepatic hydatid cysts during the operation, partial hepatectomy was performed.
CONCLUSIONS: More attention should be paid to the differential diagnosis of cystic space occupying lesions in the liver. For the treatment of hepatic cyst, if suspected, must change the surgical strategy.
Keywords: Diagnostic Errors, Echinococcosis, Hepatic, Liver Diseases, Alcoholic, Surgical Tape, Cysts, Hemangioma, Liver Diseases, Magnetic Resonance Imaging, Tomography, X-Ray Computed
Background
Hepatic hydatid cysts are a cystic disease caused by echinococcus, which can even cause death in severe cases, it mainly occurs in the liver (50% to 70%) and is relatively rare in the lungs and other parts [1]. In hepatic hydatid cysts, the most common symptom is right epigastric pain (38.2%) and the least is jaundice (11.7%). The most common sign is a lump in the right upper quadrant (88.2%), and the least is ascites (5.8%) [2]. Computed tomography (CT) or magnetic resonance imaging (MRI) should be performed for incidental findings of liver cysts with septate, calcified, irregular walls or subcysts. CT can identify small cysts larger than 1 cm in diameter and observe the internal structure of cysts, liver parenchyma and biliary tract. When used in combination with serology, CT has a high specificity and sensitivity (close to 96%). MRI is superior to CT in showing the internal structure of cysts and potential biliary tract involvement. Elevated eosinophils were observed in approximately 39% of patients on laboratory examination, and elevated alanine aminotransferase (ALT) values suggested hepatolysis syndrome in patients without underlying liver disease [3]. Asymptomatic simple hepatic cyst should be closely followed up and puncture drainage is not recommended. Symptomatic simple hepatic cysts should be treated with laparoscopic fenestration. Laparoscopic or open surgery is recommended for complicated liver echinococcosis with multiple vesicles, asci, ruptured cysts, bleeding or secondary infection, and postoperative medication should be given [4].
Case Report
A 40-year-old female patient was diagnosed with hemangioma in a local hospital before June 2019. She did not receive any treatment due to no symptoms. There are endemic regions with much higher incidence of hydatid cysts, such as north-western China. But the patient was not from this area and had no history of pastoral contact.
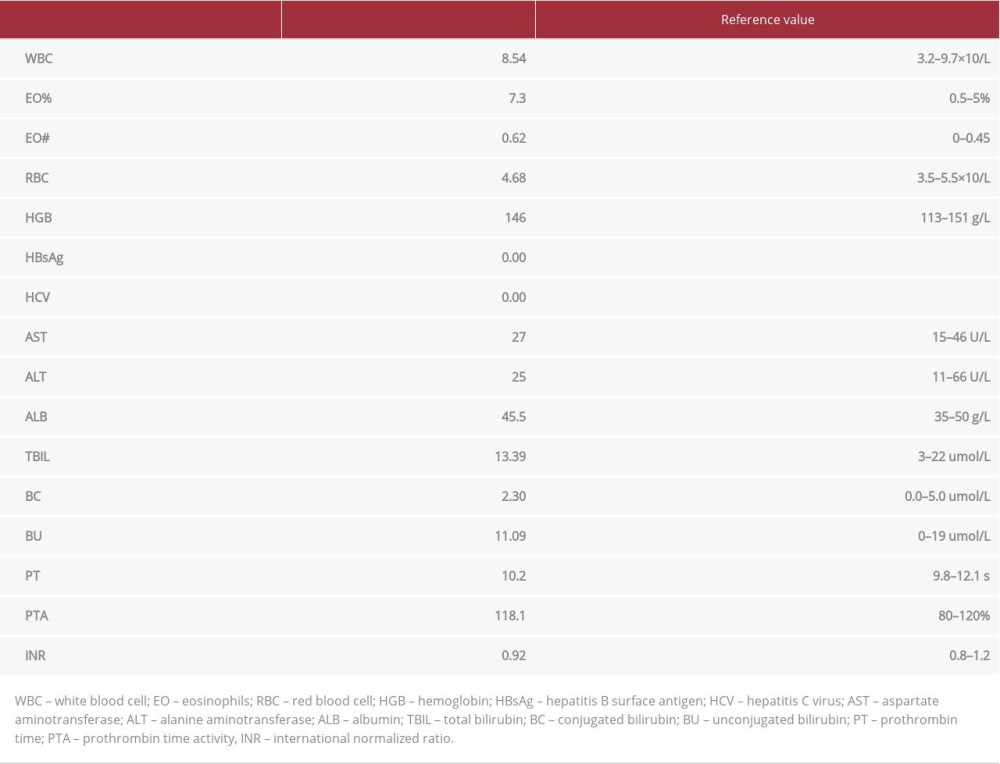
She had a follow-up CT re-examination in our hospital on July 30, 2019 that demonstrated multiple round low-density shadows seen in the left lobe and the front segment of the right lobe, with blurred boundaries; the larger one was about 3.9×3.8 cm, which was diagnosed as multiple liver cysts (Figure 1). A reexamination of MRI on September 5, 2019 showed that there were multiple round, long T1 signal and T2 signal, high STIR signal in the anterior upper segment of the right lobe and the lateral segment of the left lobe in the liver. The larger one was located in the segment of the right lobe, about 4.9×4.8×3.5 cm. The lesion’s margin of the right anterior upper segment and the left lateral segment of the liver was slightly enhanced at arterial phase, significantly enhanced at the substance phase and portal phase, while the remaining lesions were not significantly enhanced. It was diagnosed as multiple intrahepatic hemangiomas and multiple hepatic cysts (Figure 2). After admission laboratory examination results are shown in Table 1. Combined with the laboratory and imaging results, the diagnosis was considered as 1) hepatic hemangioma; 2) hepatic cyst. Therefore, we planned to perform ultrasound guided microwave ablation of hepatic hemangioma and laparoscopic fenestration of hepatic cyst on September 18, 2019.
During the operation, laparoscopic exploration revealed that there were 3 circle-like firm and rubbery masses at the lower margin of the right lobe of the liver, which suggested the possibility of hepatic hydatid cyst (Figure 3). Due to the limited space of laparoscopic operation and the unclear nature of liver mass, the patient’s procedure was converted to open laparotomy for ultrasound guided microwave ablation of hepatic hemangioma, laparoscopic exploration and partial hepatectomy. The postoperative specimen was a thick-walled firm and rubbery cystic mass containing yellow viscous cystic fluid (Figure 4). Postoperative pathology showed chronic granulomatous inflammation of the liver accompanied by coagulative necrosis and cystic changes, with a few scolex, which was considered as hepatic hydatid cysts (Figure 5). The patient was discharged 5 days after surgery.
Discussion
A hydatid cyst is a single, fluid-filled spherical vesicle consisting of an inner cell layer (germinal layer) and an outer stratum corneum. The cyst expands gradually, causing granulomatous host reaction, followed by fibrous capsule wall development. With the passage of time, the internal division and the development of the daughter cysts changed the morphology of the monolocular cyst, which is typical of the early hydatid cyst. When the final host mistakenly eats the parasitic ovum, the life cycle of echinococcosis can start again, with the protoscolex attaching to the intestinal mucosa, and developing to the adult stage within 30 to 80 days. Echinococcosis usually forms a monolocular cyst and causes space occupying effect, while alveolar echinococcosis often progresses into a polycystic mass that dilates into the adjacent liver parenchyma and resembles an aggressive malignancy [5].
The prevalence of hepatic cyst is 0.1% to 0.5%, and only less than 10% to 15% of patients will have symptoms that cause clinical attention, such as abdominal mass, abdominal pain (stretching the liver capsule), and compression symptoms (pressing the biliary tract causes jaundice, pressing the portal vein causes portal hypertension, etc.) [6].
Surgery is the main treatment, involves excising most of the cyst wall either by laparotomy or laparoscopy. Although laparoscopy is much less effective than the closed cyst resection, it has the advantage of reducing the difficulties of an eventual re-intervention, less trauma, and a lower incidence of complications. For patients with symptomatic simple hepatic cysts smaller than 500 cc in volume by using puncture, aspiration, injection, and re-aspiration (PAIR) technique is a safe and effective procedure with high success rate [7]. But the cost of such procedures cannot be supported by all health systems.
Different types of hepatic hydatid cysts may sometimes be very similar to hepatic cyst, mainly depending on the stage of development of hepatic hydatid cyst, especially in the early stage, a hepatic hydatid cyst is usually manifested as full-fluid cyst, simple imaging is difficult to distinguish from simple hepatic cyst [8]. This is the key to making early diagnosis difficult.
The differential diagnosis between hepatic hydatid cyst and simple hepatic cyst mainly includes the following points: 1) serology with eosinophil in about 39% of patients with hepatic hydatid have eosinophil elevation [3]. Other serological indicators such as EgAg5, EgAgBs, endophilin B1, and rEgAgB2 can be used as diagnostic indicators of hepatic hydatid cyst, but their clinical applicability still needs further study [9]. However, it is important to note that a single serological indicator cannot determine the diagnosis of hepatic hydatid cyst. 2) The calcification degree of cyst is not a reliable index to evaluate the activity of hepatic hydatid. Immunological tests, especially IgG4 and IgE, may be useful in assessing the activity of hepatic hydatid because they detect a higher proportion and titer during the activity phase [10]. 3) Biochemical analysis includes the concentration of glucose, Ca+ and uric acid in hepatic hydatid cyst fluid is significantly higher than that of simple hepatic cyst [11,12]. 4) Imaging, as far as current studies are concerned, the imaging features of hepatic hydatid cyst are clearly defined thick-walled cystic lesions. The difference in CT density can be used as one of the differential diagnostic indicators of hepatic hydatid cyst and simple hepatic cyst. The apparent diffusion coefficient (ADC) of diffusion weighted imaging (DWI) in MRI is significant for the differential diagnosis of hepatic hydatid cyst and simple hepatic cyst, and
Surgery is the main method for the treatment of complicated hepatic hydatid cyst (including greater than 5 cm in diameter, polycystic vesicles, infection, close relationship with biliary tract and adjacent organs, etc.) [14].
Some studies have reported that the recurrence rate of hepatic hydatid after primary surgery is 6% to 30%, and there is no significant difference in postoperative complications between laparoscopic surgery and open surgery [15]. However, open surgery is still the main surgical treatment at present, and more and more studies hope to achieve therapeutic purposes with more minimally invasive methods, such as perforator-grinder-aspirator-apparatus (PGAA) and nanosecond pulsed electric field (nsPEF). However, laparoscopic surgery also has some defects, such as difficulty in exposing partial cysts and increased risk of fluid leakage. Recurrent hepatic hydatid cyst, due to the large size of the hydatid cyst, adhered to the site of previous treatment, have a close relationship with the liver blood vessels and other problems; hepatectomy is still the main treatment method. In addition, percutaneous aspiration is a safe treatment for patients who are not suitable for surgical treatment and who have long-term use of medications for management and financial difficulties [16,17].
Postoperative drug therapy is important for hepatic hydatid. Albendazole is the most effective first-line drug for the treatment of hepatic hydatid cyst. How to improve drug release performance is a breakthrough point to improve drug treatment effect.
Conclusions
More attention should be paid to the differential diagnosis of cystic space occupying lesions in the liver. In this case, preoperative ultrasound, CT, and MR did not indicate hepatic hydatid cyst, and the elevated eosinophils in the blood routine of the patient did not attract the attention of clinicians, resulting in preoperative misdiagnosis as simple hepatic cyst. Due to the timely change of treatment methods after intraoperative laparoscopic exploration, the adverse clinical results caused by fluid leakage, which may be caused by puncture and other operations, were avoided. For cystic space occupying lesions with complicated liver conditions, multiple examination methods including MRI, serology and immunoassay should be combined to improve the diagnostic rate. In this case, it was because of the complicated situation of cystic lesions in the lower margin of the right liver lobe that laparoscopic exploration was decided, instead of direct puncture and drainage guided by ultra-sound to deal with cystic lesions, so as to avoid the possibility of strong allergic reaction caused by the leakage of cystic fluid. In patients with cystic liver disease, it is still a challenge for surgeons to make a clear diagnosis and adopt appropriate treatment. This case can provide some references for the future treatment of cystic liver lesions.
Figures
References:
1.. Nunnari G, Pinzone MR, Gruttadauria S, Hepatic echinococcosis: Clinical and therapeutic aspects: World J Gastroenterol, 2012; 18; 1448-58
2.. El-Ghareeb AS, Waked NM, Al-Feky HM, Clinical and parasitological studies on pulmonary and hepatic hydatid cysts in hospitalized children and adults: J Egypt Soc Parasitol, 2016; 46; 9-18
3.. Botezatu C, Mastalier B, Patrascu T, Hepatic hydatid cyst – diagnose and treatment algorithm: J Med Life, 2018; 11; 203-9
4.. Marrero JA, Ahn J, Rajender RK, ACG clinical guideline: Tdiagnosis and management of focal liver lesions: Am J Gastroenterol, 2014; 109; 1328-47 , 1348
5.. Eckert J, Deplazes P, Biological, epidemiological, and clinical aspects of echinococcosis, a zoonosis of increasing concern: Clin Microbiol Rev, 2004; 17; 107-35
6.. Haap M, Seeger A, Haas CS, Giant solitary hepatic cyst: Liver Int, 2008; 28; 840
7.. Akhan O, Islim F, Balci S, Percutaneous treatment of simple hepatic cysts: The long-term results of PAIR and catheterization techniques as single-session procedures: Cardiovasc Intervent Radiol, 2016; 39; 902-8
8.. Caremani M, Lapini L, Caremani D, Occhini U, Sonographic diagnosis of hydatidosis: The sign of the cyst wall: Eur J Ultrasound, 2003; 16; 217-23
9.. Han X, Kim J, Wang H: Parasite Vector, 2019; 12; 323
10.. Conchedda M, Caddori A, Caredda A, Degree of calcification and cyst activity in hepatic cystic echinococcosis in humans: Acta Trop, 2018; 182; 135-43
11.. Shanshan W, Hui L, Yan L, The study of biochemical profile of cyst fluid and diffusion-weighted magnetic resonance imaging in differentiating hepatic hydatid cysts from liver simple cysts: J Clin Lab Anal, 2018; 32; e22192
12.. Mortele KJ, Ros PR, Cystic focal liver lesions in the adult: differential CT and MR imaging features: Radiographics, 2001; 21; 895-910
13.. Aksoy S, Erdil I, Hocaoglu E, The role of diffusion-weighted magnetic resonance imaging in the differential diagnosis of simple and hydatid cysts of the liver: Niger J Clin Pract, 2018; 21; 212-16
14.. Brunetti E, Kern P, Vuitton DA, Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans: Acta Trop, 2010; 114; 1-16
15.. Jabbari NA, Mehrabi BM, Asadi M, Evaluation and comparison of the early outcomes of open and laparoscopic surgery of liver hydatid cyst: Surg Laparosc Endosc Percutan Tech, 2015; 25; 403-7
16.. Ormeci N, Soykan I, Bektas A, A new percutaneous approach for the treatment of hydatid cysts of the liver: Am J Gastroenterol, 2001; 96; 2225-30
17.. Pelaez V, Kugler C, Correa D, PAIR as percutaneous treatment of hydatid liver cysts: Acta Trop, 2000; 75; 197-202
Figures
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942966
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250