19 June 2020: Clinical Research
Effect of Parenting Training on Neurobehavioral Development of Infants
Mei Jiang1ABD, Quyan Zhang1BCEF, Wei Zhang1CDE, Wei He1D, Ke Huang1D, Guo Peng1D, Jinhui Huang1D, Mingyi Zhao1BCDEFG*DOI: 10.12659/MSM.924457
Med Sci Monit 2020; 26:e924457
Abstract
BACKGROUND: Early interventions have been believed to have a positive influence on the neurodevelopment of infants. Our Child Health Center has carried out parenting training for parents of infants for several years to promote the neurobehavioral development of infants at an early stage.
MATERIAL AND METHODS: We enrolled 117 families with term infants age 0–3 months who had completed a parenting training class at the Child Health Center of the Department of Pediatrics, the Third Xiangya Hospital. Parenting training included 4 parts: nursing, intelligence, social contact, and physical ability. A nurse practitioner demonstrated procedures to parents, who then performed them at home for 1 month. The Neonatal Behavioral Neurological Assessment (NBNA) was used to evaluate infants before and 1 month after parenting training.
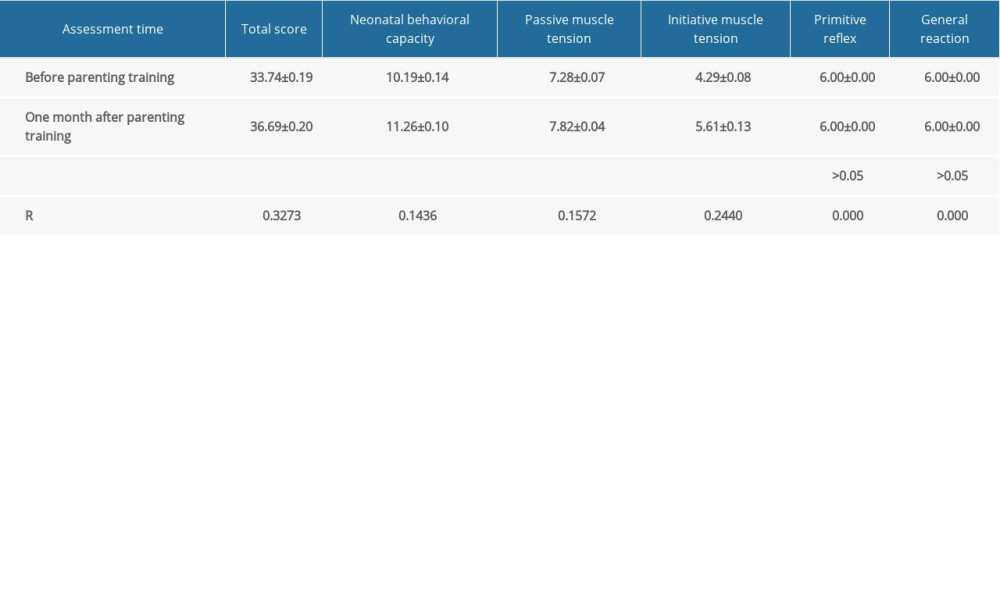
RESULTS: In the comparative analysis before and after parenting training, there was a significant increase in the NBNA scores. For the infants whose parents received parenting training, the NBNA scores in total score (33.74±0.19 before parenting training vs. 36.69±0.20 after 1 month), neonatal behavioral capacity (10.19±0.14 before parenting training vs. 11.26±0.10 after 1 month), passive muscle tension (7.28±0.07 before parenting training vs. 7.82±0.04 after 1 month), and initiative muscle tension (4.29±0.08 before the parenting training vs. 5.61±0.13 after 1 month) were significantly higher one month before (P<0.01).
CONCLUSIONS: Term infant neurobehavior was associated with participation in parenting training, suggesting that these practices of parenting training support better early neurobehavioral development of infants.
Keywords: Child Health Services, Early Intervention (Education), Neurobehavioral Manifestations, Patient Participation, Child Development, Infant, Infant Behavior, Infant, Newborn, Muscle Tonus, Parenting, Parents, Reflex, Social Behavior
Background
During pregnancy, structural differentiation of the central nervous system (CNS) occurs rapidly at 23–32 weeks of gestation [1]. The procedure occurs in utero in a term pregnancy, but it is always unstable in preterm pregnancy, with numerous stressors [2]. A preterm infant has a rather immature nervous system, which may lead to long-term neurodevelopmental consequences, such as severe neurosensory impairment. Because of the plasticity of the CNS in infants, it is believed that positive interventions can improve neurodevelopment, including cognitive and behavioral outcomes [3]. To improve the neurodevelopment, several efforts have been made, both internally and externally.
It was reported that modifications of care practices could improve infants’ clinical and neurobehavioral functioning [2]. Studies showed that better neurobehavioral stability was associated with higher levels of developmental care. Use of the Newborn Individualized Developmental Care and Assessment Program (NIDCAP) improved cognitive and motor development [4,5]. Moreover, it was preliminarily reported that patterned feeding intervention during a critical time in neurologic system development may enhance neural connections [1]; unfortunately, the outcomes of that clinical trial have not been reported yet.
Despite some exciting outcomes, the effects of these interventions on preterm infants’ neurobehavioral development remain unclear, and stronger and more consistent evidence is needed [6]. The long-term effects remain uncertain, but these findings have significant influences on the development of interventions to promote neurodevelopment during the early stage of infants.
However, the influence of systematic parent behavior on infant neurobehavioral development has rarely been studied. The role of parents in early intervention is significant [3]. A study revealed that specific parenting behaviors, particularly parent-child synchrony, were associated with neurobehavioral development [7]. Parents are encouraged to smile, laugh, and share their emotions so that they can have a positive influence on the development of infants.
Most relevant research has focused on the effects of early intervention on neurodevelopment, but its influence on term infants is rarely discussed. Due to the plasticity of the CNS in infants, we believe interventions practiced by parents during the early stage of term infants may have a positive effect on neurodevelopment. Appropriate and systematic stimulation of infants may benefit establishment of neuronal networks [1], which is called parenting training. We set up a training series involving nursing, intelligence, social contact, and physical ability. Our intervention is performed by parents, which solves the problem of cost [3]. Theoretically, interventions during a critical time in CNS development should enhance neural connections, thus enhancing language and other cognitive and neurobehavioral skills [1].
The Child Health Center in the Department of Pediatrics, the Third Xiangya Hospital is the first in China to offer parenting training. Both guidance and training are involved, so it guarantees the quality of such training and enables parents to get correct guidance, which is why parenting training is of great importance in health guidance. The parenting training has been conducted for several years and receives positive feedback from parents. To help more families get useful guidance at an early time, it is essential to promote the use of a demonstrative and individualized education model of early development of children.
The overall objective of this study was to test the effect of parenting training on the neurodevelopment of term infants, which is measured using the Neonatal Behavioral Neurological Assessment (NBNA) [8]. We hypothesized that infants who receive parenting training will have a higher neurobehavioral level.
Material and Methods
STUDY PARTICIPANTS:
Participants were families with term infants age 0–3 months who had a physical examination at the Child Health Center of the Third Xiangya Hospital of Central South University during the year of 2019. Apgar scores for 5 minutes of all these infants were higher than 8. The term infants were in good health and had no known diseases. Informed parental consent was necessary for family participation, and the study was approved by the Ethics Committee of the Third Xiangya Hospital of Central South University. We initially recruited 134 infants. The parents completed parenting training at the Child Health Center of the Third Xiangya Hospital of Central South University and practiced the methods at home. To guarantee that parents could practice the course according to the guidance, we assessed the completeness of this training after the class and guided them until all participants could individually perform the methods correctly. To guarantee the quality of practice at home, we contacted with parents by telephone during the research and provided guidance as needed. At the 1-month follow-up, 17 families refused follow-up.
NEUROBEHAVIORAL EVALUATION:
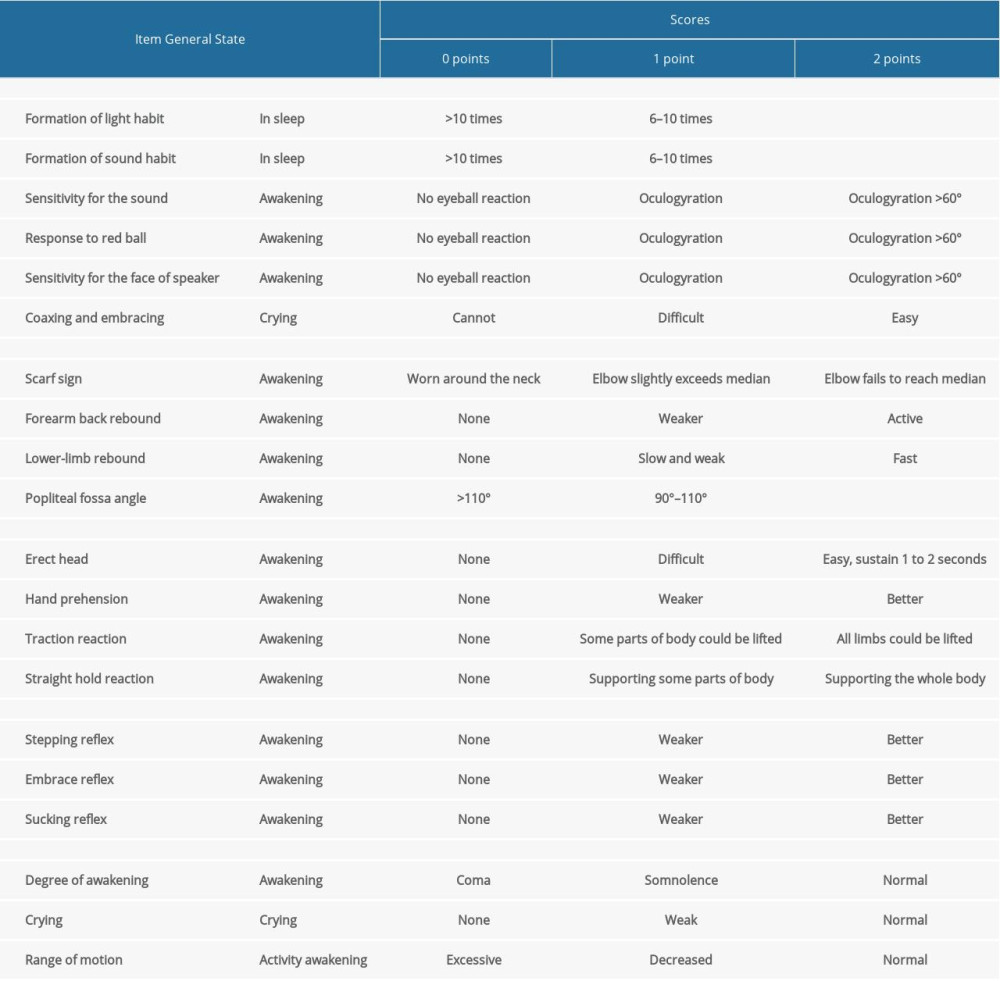
Infant neurobehavior was evaluated using the neonatal behavioral neurological assessment (NBNA). The NBNA is a standardized test to evaluate the neurobehavioral status of newborns. The assessment has 5 parts – neonatal behavioral capacity, passive muscle tension, initiative muscle tension, primitive reflex, and general reaction – and each part has the following items. There are 20 items at all. Each item was assigned 0–2 points. The environment was kept quiet and the temperature was maintained at about 26°C [8] (Table 1).
PROTOCOL OF PARENTING TRAINING:
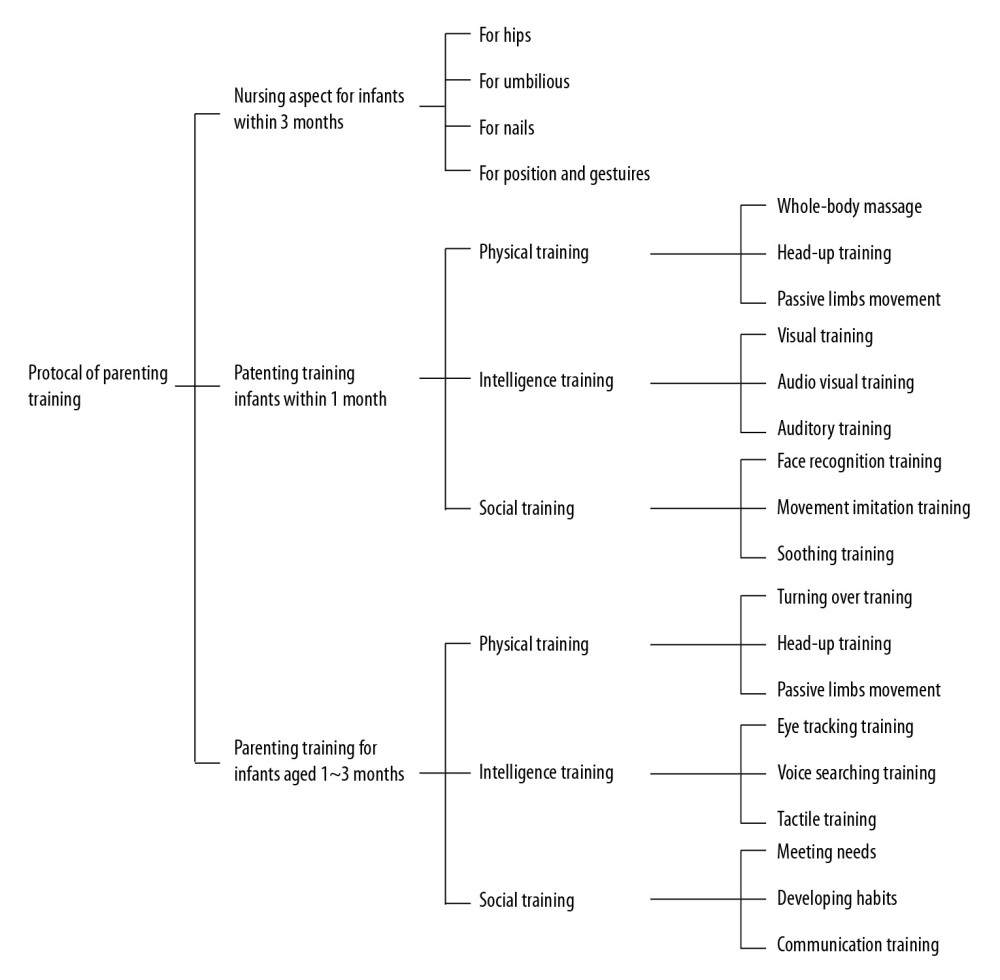
Parenting training protocol consists of 4 parts: nursing, physical training, social training, and intelligence training. There are many specific items in each part. According to different parts and postures, nursing can be divided into 4 aspects in parenting training: for hips, for umbilicus, for nails, and for position. Physical training, social training, and intelligence training are divided into 2 categories according to the age of infants: physical training for infants within 1 month (whole-body massage, head-up training, and passive limb movement training); social training for infants within 1 month (face recognition training, movement imitation training, and soothing training); intelligence training for infants within 1 month (visual training, auditory training and audio-visual training); physical training for infants aged 1~3 months (turn over training, head-up training, and passive limb movement training); social training for infants aged 1~3 months (meeting needs, developing habits, and communication training); and intelligence training for infants aged 1~3 months (eye tracking training, voice searching training, and tactile training) (Figure 1).
STATISTICAL ANALYSIS:
GraphPad Prism 8 statistical software was used for data analysis. All data are presented as mean ± standard deviation (X±s). The chi-square test was used for enumeration data. Pearson test was used to compare and analyze the correlation between constants and variables.
Result
BASIC INFORMATION:
The study included 117 infants and their family. All participants performed the parenting training at home for 1 month. The characteristics of this group are shown in Table 2.
COMPARISON OF NEUROBEHAVIORAL EVALUATION:
The results in Table 3 show that 1 month after parenting training, the neurobehavioral evaluation of infants increased. Parenting training was associated with optimal neurobehavioral development. Before parenting training, the average total score of NBNA was 33.74±0.19 and after this, the score increased to 36.69±0.20 (P<0.01). The neonatal behavioral capacity score increased to 11.26±0.10 from 10.19±0.14 (P<0.01), the passive muscle tension score increased to 7.82±0.04 from 7.28±0.07 (P<0.01), and the initiative muscle tension score increased to 5.61±0.13 from 4.29±0.08 (P<0.01). The participation of parenting training was not associated with the primitive reflex score or the general reaction score (P>0.05).
Discussion
This study reinforces the view that parenting training plays a crucial role in the early neurodevelopment of infants. Our findings prove that parenting training is of great importance to the neurobehavioral development of infants in the early stage, showing that the neurobehavioral assessment scores increased remarkably after 1-month parenting training. For example, parenting training had a significant effect on neonatal behavioral capacity, passive muscle tension, and initiative muscle tension. Importantly, these findings prove that parenting training, which is a form of early intervention, can promote the neurodevelopment of all infants, not just preterm infants [1,2,7].
The evolution of the human brain is attributed to interactions between genes and environment, with experience guiding final maturation of the neural system [9]. It is believed that neural circuits are highly sensitive to experience, especially in the early development period. The underlying mechanism of neural plasticity is synaptic plasticity. Due to CNS plasticity, virtually any experience can change the brain, and synaptic change is somewhat age-dependent [10]. As a result, the early stage of infants is significant in brain development. The relationship between experiences and CNS plasticity two-way, which means the brain can produce adaptive behavioral changes after external stimulus [11]. By providing positive interventions, the potential of the brain can be activated. Our findings agree with the principle of some behavioral rehabilitation and early intervention programs [10,12].
Environmental enrichment (EE) was reported to accelerate brain development in rodents [13], and it is known to have profound influence on the CNS at functional, anatomical, and molecular levels [14], but the underlying mechanism is still unclear [14,15]. Abundant external stimulation may be a key factor in the early stage of EE, and we believe that family plays a vital role in providing stimulation. In addition to evidence of the short-term effects of EE, some studies reported on the long-term effects. It was reported that early educational and health enrichment led to increases in psychophysiological orienting and arousal after several years [16]. Both short-term and long-term effects of EE warrant further research and discussion.
However, few studies emphasize the role of family in early intervention programs. There is convincing evidence proving the relationship between the quality of early nurturance and brain development, reporting that maternal support in early childhood was strongly predictive of hippocampal volume measured at school age, which is the crucial region of memory and stress modulation [17]. Family-centered care is a philosophy of care that emphasizes the integrity of the family and individualizing care [18]. A retrospective cohort study focused on the environmental enrichment, parent-guided environmental interaction, and infant development assessed the effect of a home-based family-centered early developmental habilitation program, finding that both cognitive and behavioral outcomes were improved [11].
Infants possess the senses of sight, hearing, touch, and other ability, so repetitive and regular stimulus outside may stimulate the maturity of the neuro system. Parenting training can be divided into 4 parts: nursing, intelligence, social contact, and physical ability. Because most parents in China are new parents and do not have much basic knowledge about how to nurse infants, we added a nursing component to the training, which includes use of the hip and navel, the correct way to hold an infant, and other suggested nursing patterns. The reason is that we consider that. This kind of knowledge is the foundation of subsequent training, guaranteeing the efficacy of parenting training. With correct basic nursing knowledge, parents could go on to subsequent contents. For example, the physical ability component includes full-body massage and passive motion of the infants’ body. Full-body massage can promote blood circulation, enterocinesia, and digestion and absorption of food. It was reported that body massage in preterm infants had a positive effect on brain development, especially visual development [19,20]. It was also reported that massaged infants had higher cognitive scores [21]. Passive motion of the infants’ body may increase the muscular strength and joint range of motion, leading to higher motor function.
Other than the supplemented content of training, the form of parenting training class is improved to have better outcomes. In parenting training class, the experienced nurse practitioner used slides and vivid baby-like models to elaborate the contents of training instead of only playing the training video to parents. Parents can use designed models and tools to practice the procedure under the guidance of a nurse practitioner. This face to face and hand by hand pattern of training maximizes the efficiency of training and guarantees the quality of training. Moreover, the nurse practitioner not only teach parents how to practice the training, but also tells parents why they need to practice the training. Knowing the necessity of training, parents show higher program compliance, guaranteeing that infants can receive correct, valid, and long-term care. Because we established the training class, the degree of satisfaction of trained parents remains high.
Moreover, in the routine process of assessment, we do not only assess the neurobehavioral development of infants, but also tell parents about inadequacy or problems in the process of development and give specific guidance to parents, which means that we give parents both the general parenting training class and specific guidance for the CNS development of infants.
Limitations of our study include not accounting for natural growth of CNS and lack of a control group. Considering the natural process of CNS development, the increased level of neurobehavioral assessment may not be affected just by the 1-month parenting training. Even without parenting training, the neurobehavioral assessment score may also increase spontaneously and slowly. Lack of a control group makes the experiment less rigorous and complete, and the effect of various significant factors that might influence the results and should theoretically be excluded cannot be eliminated or even reduced. It is possible that the improved neurobehavioral assessment scores of infants with 1-month parenting training would be similar to those of infants of parents who did not receive parenting training. Moreover, the interplay between parenting training and some other unknown or uncontrollable environmental factors cannot be eliminated.
Our findings are of great theoretical and clinical significance. The outcomes add to the credibility of early intervention to improve CNS development. It also provides a new form of early intervention that can be practiced in the clinic and at home. The substantial content and improved form of training greatly increase the feasibility of practicing these suggested procedures.
The mechanism underlying the effect of early intervention on CNS development of infants at the early stage remains unclear. Different parts of parenting training have a comprehensive influence on infants, so it is hard to know the specific effect of each part. Moreover, there is also a parenting training class targeted at families with term infants 3–6 months old. In the future, we plan to evaluate the effects and assess difference between these 2 interventions. Our results will show the effect of parenting training on CNS development of infants and may popularize its use in the clinic and by the family at home.
Conclusions
In conclusion, term infant neurobehavioral development was associated with participation in parenting training, suggesting that these practices of parenting training support better early neurobehavioral development of infants.
Supplementary Materials: Protocol of Parenting Training
NURSING ASPECT:
There are 4 aspects for nursing care in parenting training: hips, umbilicus, nails, and position. For the hips, parents should first clean the buttocks of the newborn with warm water, absorb the water with cotton towel, and evenly smear with MEBO after air drying. For the umbilicus, avoid covering the umbilicus with diapers. Absorb water in the umbilicus of the infant with sterilized dry cotton swabs after bathing. The infant’s nails should be cut into a circular arc once a week. For position, the side of the hand holding the child and sleeping position relative to baby should always be changed on time, meaning the parent holds the infant with the left hand one week, and the next week the parent should do it with the right hand. For the sleeping position, if the parent sleeps on the left side of the infant one week, next week the parent should sleep on the right side of the infant. Also, if one week the infant sleeps with head at the end of the bed, the next week the infant should sleep with head at the other side. When the infant prostrates naturally, the head and back should be on the same plane. Furthermore, the nose, navel, and perineum of the infant should be in line.
PHYSICAL TRAINING FOR INFANTS WITHIN 1 MONTH:
Whole-body massage: Cover eyebrows of the infant with both hands, and do it from the inside out to the temple and from both sides of alar to the root of the nose for facial massage. Perform chest massage from the middle of the chest upward in a circular manner. Perform abdominal massage clockwise. Finally perform the massage and knead for palm of hands, the sole of foot, fingers, and toes.
Head-up training: Let the infant lie prone on the table. Hold the infant’s armpits with both hands, and slowly raise the infant’s head. According to the strength of the infant, the strength of the upper support can be gradually reduced.
Passive limb movement: When performing upper-limb training, the wrists of infant need to be hold by both hands. Stretch first, and then flex. When performing lower-limb training, ankles of the infant need to be held by both hands. Bend up first, and then stretch.
INTELLIGENCE TRAINING FOR INFANTS WITHIN 1 MONTH:
Visual training: The infant lies supine, facing straight ahead. A soft red ball is presented at the midline of the body, at the height of about 20 cm from the eyes. The parent shakes the ball gently to attract the infant’s attention first. When the infant is watching the red ball, the parent should move it slowly from the center line to one side, with synchronous rotation of the ball. Take turns on both sides, 3–4 times a day, no more than 5 minutes each time.
Auditory training: Let the infant listen in a quiet environment, and then attract the infant to turn its head, with shaking the sand hammer gently 20 cm away from the ears. Another feasible way is to call the infant softly near the ear to attract the infant to turn its head. Take turns on both sides 3–4 times a day, no more than 5 minutes each time. To avoid distraction, there should be no visual stimuli when auditory training is going on.
Audio-visual training: The parent calls the infant at the distance of about 20 cm and slowly moves the head from midline to left or right 90° to attract the infant’s eyes to follow.
SOCIAL TRAINING FOR INFANTS WITHIN 1 MONTH:
Face recognition training: The name of the infant should be called, the voice should be kind, gentle and persistent, and the facial expressions should be mobile.
Movement imitation training: The parent makes some facial movements, such as sticking out the tongue, to induce the infant to imitate the action. This should not be compulsive.
Soothing training: There are 3 aspects. First, the parent should use gentle words and abdomen touch. Second, the hands of the infant are held by the parent and then put on the abdomen. Third, bend over to pick up the infant.
PHYSICAL TRAINING FOR INFANTS AGED 1~3 MONTHS:
Turn over training: Let the infant lie on the table, and attract it to turn around. When the infant cannot turn over actively, the parent should pull the lower limbs sideways and gently push its back to help it turn over. It is best to train no more than 5 minutes each time.
Head-up training: At this time, the infant can actively complete the neck up movement with 45~90°.
Passive limb movement: Hold the baby’s wrist to do flat extension and flexion movement. Hold the baby’s ankle to do upward bending and extension movement. Repeat each operation 4 times.
INTELLIGENCE TRAINING FOR INFANTS AGED 1~3 MONTHS:
Eye tracking training: Attract the infant with some colorful object. A soft red ball is presented at the midline of the infant’s body and the height of about 20 cm from the infant’s eyes to attract the infant. Make sure that the infant’s eyes focus on the red ball, move it slowly from the midline to the left or right side, then repeat it from midline to the top or the bottom side. It is best to train no more than 5 minutes each time.
Voice searching training: Attract the infant with some objects making melodious sounds. Shake the sand hammer gently 20 cm away from the infant’s ears. Do it from left to right side, or from top to bottom side. It is best to train no more than 5 minutes each time.
Tactile training: Put different textured items (e.g., small bell, small building block) in the infant’s hands and guide them to grasp. It is normal that the infant cannot hold them. These objects should be innocuous, suitable to grasp, and smooth to avoid scratches.
SOCIAL TRAINING FOR INFANTS AGED 1~3 MONTHS:
Meeting needs: Parents need to know the signals of needs. Coax and pacify the infant and give timely response.
Develop habits: Help the baby find and develop a regular rhythm of life, such as eating, drinking, and sleeping regularly. A gradual decrease in the number of night feedings can form a circadian rhythm. Creating a good environment can form regular sleeping habits, including dimming the lights.
Communication training: The mother holds the infant and communicates with the infant face to face, such as saying “baby, I’m mother”, to amuse the baby and lead the baby to find the mother.
References
1. Pickler RH, Wetzel PA, Meinzen-Derr J, Patterned feeding experience for preterm infants: study protocol for a randomized controlled trial: Trials, 2015; 16; 255
2. Montirosso R, Del Prete A, Bellù R, Level of NICU quality of developmental care and neurobehavioral performance in very preterm infants: Pediatrics, 2012; 129(5); e1129-137
3. Spittle A, Treyvaud K, The role of early developmental intervention to influence neurobehavioral outcomes of children born preterm: Semin Perinatol, 2016; 40(8); 542-48
4. Wallin L, Eriksson M, Newborn Individual Development Care and Assessment Program (NIDCAP): A systematic review of the literature: Worldviews Evid Based Nurs, 2009; 6(2); 54-69
5. Ohlsson A, Jacobs SE, NIDCAP: A systematic review and meta-analyses of randomized controlled trials: Pediatrics, 2013; 131(3); e881-93
6. Symington A, Pinelli J, Developmental care for promoting development and preventing morbidity in preterm infants: Cochrane Database Syst Rev, 2006(2); CD001814
7. Treyvaud K, Anderson VA, Howard K, Parenting behavior is associated with the early neurobehavioral development of very preterm children: Pediatrics, 2009; 123(2); 555-61
8. Bao XNeonatal behavioral ability and assessment: Journal of Practical Diagnosis and Therapy, 2003; 17(06); 441-43 [in Chinese]
9. Sale A, Berardi N, Maffei L, Environment and brain plasticity: Towards an endogenous pharmacotherapy: Physiol Rev, 2014; 94(1); 189-234
10. Kolb B, Muhammad A, Harnessing the power of neuroplasticity for intervention: Front Hum Neurosci, 2014; 8; 377
11. Poggioli M, Minichilli F, Bononi T, Effects of a home-based family-centred early habilitation program on neurobehavioural outcomes of very preterm born infants: A Retrospective Cohort Study: Neural Plast, 2016; 2016 4323792
12. Markham JA, Greenough WT, Experience-driven brain plasticity: Beyond the synapse: Neuron Glia Biol, 2004; 1(4); 351-63
13. Landi S, Sale A, Berardi N, Retinal functional development is sensitive to environmental enrichment: A role for BDNF: FASEB J, 2007; 21(1); 130-39
14. Baroncelli L, Braschi C, Spolidoro M, Nurturing brain plasticity: Impact of environmental enrichment: Cell Death Differ, 2010; 17(7); 1092-103
15. Sale A, Berardi N, Maffei L, Enrich the environment to empower the brain: Trends Neurosci, 2009; 32(4); 233-39
16. Raine A, Venables PH, Dalais C, Early educational and health enrichment at age 3–5 years is associated with increased autonomic and central nervous system arousal and orienting at age 11 years: Evidence from the Mauritius Child Health Project: Psychophysiology, 2001; 38(2); 254-66
17. Luby JL, Barch DM, Belden A, Maternal support in early childhood predicts larger hippocampal volumes at school age: Proc Natl Acad Sci USA, 2012; 109(8); 2854-59
18. Lester BM, Miller RJ, Hawes K, Infant neurobehavioral development: Semin Perinatol, 2011; 35(1); 8-19
19. Guzzetta A, Baldini S, Bancale A, Massage accelerates brain development and the maturation of visual function: J Neurosci, 2009; 29(18); 6042-51
20. Guzzetta A, D’Acunto MG, Carotenuto M, The effects of preterm infant massage on brain electrical activity: Dev Med Child Neurol, 2011; 53(Suppl 4); 46-51
21. Abdallah B, Badr LK, Hawwari M, The efficacy of massage on short and long term outcomes in preterm infants: Infant Behav Dev, 2013; 36(4); 662-69
In Press
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952