09 November 2020: Database Analysis
Emerging Trends and Hot Topics in Cardiopulmonary Resuscitation Research: A Bibliometric Analysis from 2010 to 2019
Tianyuan Jia1ABCDEF, Chengzhun Luo1BEF, Shiwei Wang1BCF, Zida Wang1C, Xiaoye Lu1AD, Qian Yang1DE, Changqing Zhu1AG*DOI: 10.12659/MSM.926815
Med Sci Monit 2020; 26:e926815
Abstract
BACKGROUND: Cardiopulmonary resuscitation (CPR) is a topic of great scientific and clinical interest that has received much attention in the past decade. Our study aimed to predict the trends in CPR research activities and evaluate hot topics via bibliometric means, quantitatively and qualitatively.
MATERIAL AND METHODS: All data were collected from a search of the Web of Science Core Collection on May 12, 2020. Retrieved information was investigated with bibliometric analysis by CiteSpace and VOSviewer software and the Online Analysis Platform of Literature Metrology to analyze and predict the trends and hotspots in this field.
RESULTS: Our search returned a total of 9563 articles and reviews on CPR published from 2010 through 2019. The number of original research studies on CPR has been increasing annually. The journal Resuscitation published the greatest number of manuscripts involved CPR, and the leading country and institution with regard to contributions on CPR were the United States and the University of Pennsylvania. Keyword co-occurrence/co-citation-cluster analysis showed that the most popular terms associated with CPR occurred in the manner of cluster labels, such as therapeutic hypothermia and treatment recommendation, among others. In addition, palliative care, sepsis, extracorporeal membrane oxygenation, and brain injury were identified as new foci through burst detection analysis.
CONCLUSIONS: Our study showed that the scientific research focus on CPR is switching from traditional therapeutic treatments to a public health practice, with in-depth understanding and development of CPR-related techniques expanding over the past decade. These results demonstrate trends in the CPR research and detected the possible neo-foci for ensuing research.
Keywords: Bibliometrics, Cardiopulmonary Resuscitation, Emergency Service, Hospital, Authorship, Biomedical Research, Cluster Analysis, Internationality, Periodicals as Topic
Background
Cardiac arrest (CA) has continuously manifested as a public health burden, with the vast majority of patients having poor outcomes, regardless of being in or out of a hospital. In the United States alone, approximately 290 000 experience in-hospital cardiac arrest (IHCA) and 350 000 people experience out-of-hospital cardiac arrest (OHCA) annually, with less than 25% and 10% surviving, respectively. Around the globe, the incidence and mortality rates of CA are increasing [1–3]. Modern cardiopulmonary resuscitation (CPR), which represents additional development and advances in earlier forms of CPR, encompasses rapid first-aid and life-supporting technology for sudden cardiac and respiratory arrest. It involves emergency airway management; artificial-assisted ventilation; chest compression; electric defibrillation; correction of ventricular fibrillation (VF) or pulseless ventricular tachycardia or electrical activity; and other basic or advanced cardiac life support [3–5]. Modern CPR is capable of saving patients by promoting the return of spontaneous circulation and decreasing CA-related mortality. Furthermore, robust CPR guidelines, especially those published by the American Heart Association (AHA) in 2015 and the latest updates on 2019, underline not only the importance of high-quality CPR, but also provide detailed information about first-aid life-chain in adult CPR, such as dispatcher-assisted CPR, cardiac arrest centers, prehospital treatment of presyncope, and so forth [6,7]. Nevertheless, the success rate for CPR remains low and significant controversies need to be resolved. For example, some recommendations lack persuasive evidence because large randomized controlled trials have not been conducted; further, the clinical practice of CPR varies greatly in quality and compliance with some recommended targets is poor [8]. Consequently, urgent priorities include exploring research hotspots in combination with clinical practice and continuously advancing CPR technology to improve CA/CPR-related disease prognosis.
Recently, the use of bibliometric analysis has become a popular means of identifying trends and hotspots within specific areas of research. Such analysis enables quantitative measurement of contributions of a specific field of research, including different countries/regions, institutions, journals, authors, co-cited networks, and other details that highlight research trends or hotspots in a field [9]. However, literature-metrology study on CPR is scarce, let alone any focus on analysis and prediction of research hot topics or trends [10]. In this article, we aimed to identify potential hotspots and trends in CPR research from various aspects, including technological development, pathogens, pathophysiology, complications, prognosis, and clinical guidelines. Our goal was to contribute to the improvement of CPR performance via a comprehensive analysis of information from manuscripts published worldwide from 2010 to 2019.
Material and Methods
We restricted our literature search to original articles and reviews from 2010 to 2019, using the Web of Science Core Collection (WoSCC) database, which contains the Science Citation Index-Expanded (SCIE) and the Social Science Citation Index (SSCI). The retrieval strategy was “TS=(cardiopulmonary resuscitation) AND Language=English,” with the document types refined as “article OR review.” Document retrieval and recording were entirely completed on May 12, 2020, to avoid variation in citations caused by frequent database updates. Moreover, 2 reviewers (T. Jia and C. Luo) were independently in charge of the primary search; their agreement showed a considerable accordance. They identified 9563 studies, which cited 57 688 references that were eventually obtained and bibliometrically analyzed through the Online Analysis Platform of Bibliometry (
Results
DISTRIBUTION CHARACTERISTICS OF ARTICLES:
Altogether, 9563 research publications (8492 articles and 1071 reviews) from 2010 to 2019 were filtered out by customized retrieval strategies and inclusion criteria. An increasing trend was clearly apparent for the amount of original research literature on CPR annually as a whole (from 631 in 2010 to 1192 in 2019), although there was a plateau between 2011 and 2012 and slowdown from 2016 till the end of 2019 (Figure 1A). Growth trends and the number of publications by separate country or region were both demonstrated by publication years (only top 10 of countries/regions are listed in Figure 1B).
Among all 120 countries/regions from which literature on CPR originated, the United States contributed the largest number of publications on CPR research (3653), followed by Canada (706), Japan (657), China (640), and South Korea (615). In addition, the degree of centrality index showed by CiteSpace, particularly with regard to Freeman’s betweenness centrality in social networks, was another vital indicator used to evaluate the significance of nodes in a definite network, independent of the article counts [11]. By this measure, we found that Australia (centrality=0.13), which was ranked eighth in the number of articles, had an extraordinary centrality. This finding indicated that it was the most influential, overtaking research from the United States, England (0.12), and Italy (0.10) (Table 1). However, the centrality values of the top 10 institutions was below 0.15, which implies that these institutions had less influence than we expected. The top 10 research institutions included the University of Pennsylvania (606), University of Washington (509), University of Toronto (461), University of Pittsburgh (424), and University of Michigan (303) (Table 1). However, the map of the CPR research network presented us with a low-density level (density=0.0267) (Figure 2A), which indicates that the teams devoted to CPR research are dispersed in various institutions throughout the world and deeper cooperation is needed. In addition, we used network analysis to confirm the relationship of collaboration between countries, and we found that the most frequent cooperation occurred between the United States and Canada, followed by the United States and China (Figure 2B).
Until 2019, 1150 journals have included articles on CPR research. The top 10 most active journals published 3292 articles, which accounted for 34.42% of the 9563 articles on CPR in our research. Table 2 lists the top 10 journals, sorted by article counts. Of the top 3 journals, Resuscitation alone accounted for almost 17.69% of the articles, which far exceeded the other 2 journals. However, in terms of impact factor (IF), Circulation was in first place (23.054), followed by Critical Care Medicine (6.971), Critical Care (6.959), Resuscitation (4.572), and Pediatric Critical Care Medicine (2.798). Meanwhile, the Journal Citation Reports assessment system, which is also an important evaluating tool and method for SCI journals, divided journals into 176 different subject categories and classifies them into quartiles, according to the level of a journal’s impact factor. Our study results showed that all top 10 journals were classified as either Q1 or Q2, which means that these journals likely have a strong influence on research about CPR.
The top 10 most productive authors of all the 32 810 authors identified in the current study are shown in Table 3; the top 3 were Robert A. Berg, who ranked first with 160 articles; Vinay M. Nadkarni, 144 articles; and Clifton W. Callaway, 100 articles. The top 2 authors have different affiliations, but are in the same region: separately, Center for Resuscitation Science at the University of Pennsylvania and the Children’s Hospital of Philadelphia.
Next, the networks of citation information for authors (Figure 3A) and co-cited authors (Figure 3B) were visualized with CiteSpace software. Our research output showed that Jerry P. Nolan with 1343 co-citation counts was in first place among the top 10 co-cited authors, followed by Robert W. Neumar (1078), Gavin D. Perkins (1012), Graham Nichol (909), and Mary Ann Peberdy (985) (Table 3). Of all the values of centrality among the top 10 productive authors, only 2 scholars, Jerry P. Nolan’s (0.18) and Vinay M. Nadkarni’s (0.11) were more than 0.1, which implies that both of them have made outstanding achievements in the fields of CPR research and have provided crucial foundation for follow-up scientific studies.
The top 10 co-cited articles with cited frequency, half-life, article, and research types are listed in Table 4. Among these articles, most were published in Resuscitation and Circulation, which have always been the most influential and authoritative journals in the fields of critical and cardiovascular medicine. In addition, these top 10 articles are considered as clinical instruction in CPR research.
The visualization of keywords co-occurrence network-based methods was applied successfully in the 9563 scholarly articles to screen out 256 keywords from a total of 17 093 samples. The selection criteria included a keyword having a minimum of 60 occurrences, and the keywords were then classified into 6 clusters via VOSviewer (Figure 4).
CO-CITATION AND CLUSTER ANALYSIS OF CPR RESEARCH:
To identify CPR-related research hotspots, we created a co-citation and clustered network from 1356 references (not excluding duplicates) cited in the 9563 learning-manuscripts and mapped via CiteSpace in a hierarchical order (Figure 5A). In addition, in this special network, the size of each cluster was composed of different node types representing the number and centrality of co-cited references. The representative citations displayed the major research topics and thematic concentrations of each cluster. As shown in Figure 5A, the co-cited references clustered into 9 major cluster labels, including therapeutic hypothermia, treatment recommendation, OHCA, chest compression, AHA guideline, and so forth. In addition, Figure 5B shows the clear co-citation network in a timeline view, and the top 6 have higher degrees of citation bursts. Meanwhile, it is obvious that the central points in CPR research have shifted from a concentration on brief treatment principles to pursuing technical means for life support and standardization of the CPR process.
A burst detection algorithm is designed to identify the emerging concepts in professional terminology. We used the keywords from the 9563 articles identified in the WoSCC database search and listed the top 25 of 98 keywords with the strongest citation bursts (Figure 6). The timeline with a sky-blue background color is divided by year, and once a subject has been found to “burst,” it is marked in red on the blue timeline to signify the beginning and ending years and the duration of the burst.
Although the number of keywords with the most robust citation bursts approached 100, not all of them had real significance in clinical practice. Figure 6 shows those that specifically pertain to research trends for CPR. Throughout 2010 to 2019, VF had the highest burst strength (26.6972), followed by targeted temperature management (TTM, 24.9031), cardiopulmonary resuscitation (22.4629), mild hypothermia (20.5559), and palliative care (19.379). In terms of the beginning year, of the last 8 keywords at the bottom of Figure 6, aside from the 3 with the strongest burst strength, the rest included compression, vasopressin, Utstein style, ischemia, and automated external defibrillator were the focus of CPR research. In the ensuing years, some keywords had only a short-term burst, such as sudden death, reperfusion, neuron specific enolase, and septic shock, among others. Regardless of the beginning year of bursts, however, plenty of bursts have continued until 2019, including prognostication, TTM, and some that emerged in 2017 (i.e., sepsis, palliative care, extracorporeal membrane oxygenation [ECMO], and brain injury).
Discussion
The visualization functions of CiteSpace, VOSviewer, and the Online Analysis Platform of Literature Metrology enabled conducting a bibliometric analysis of original articles involving in CPR research over the past decade. The analysis clearly showed a growing trend in the number of scientific articles published on the topic from 2010 through 2019. From this, we find that CPR has gradually become an important subject in fields of related research. Furthermore, we also find that the burst of studies during the most recent 10 years has mainly varied with the quinquennial updates of authoritative clinical guidelines, particularly those developed by the AHA-led International Liaison Committee on Resuscitation since 2000. Obviously, the development of CPR-related technology is a driving force for this research, but more importantly, thousands of scholars and researchers have gained a deeper understanding of the epidemiology, pathophysiology, treatment, and prognostication about CPR-related illnesses and complications as well as strengthened the role of evidence-based medicine.
An analogous conclusion can also be drawn from the rank of the journals with the largest number of articles published on CPR. As shown in Tables 2 and 4, the journals with enormous influence in emergency/critical care and cardiovascular medicine were predictably the most prominent in our analysis: the overwhelming majority of the articles appeared in
By combining the keyword co-occurrence and co-citation cluster analysis (Figures 3, 4A, 4B), it is not difficult to find that treatment recommendation (e.g., therapeutic hypothermia, an important part of care bundle), authoritative and instructive guidelines (AHA and emergency cardiovascular care), CPR technical means (extracorporeal life support and chest compressions), and prognostication (survival and prognosis) have always been central topics of investigations on CPR. Furthermore, as previously mentioned, VF and TTM have attracted considerable research attention in the past decade, but since 2017, sepsis, palliative care, ECMO, and brain injury have become the novel foci (Figures 5, 6). This shift could be explained by issues related to patient-specific pathophysiology having been solved through new techniques, so scholars have started to pay more attention to risks that threaten long-term survival of patients. Keyword bursts with the most strength and prominence can reveal recent trends and hotspots in CPR research.
VF has been considered to be a leading pathogenesis of sudden cardiac arrest, in or out of the hospital, but definitely more emergent and dangerous in OHCA [18]. Thus, a great amount of research and constantly updated guidelines during the past decade have focused on VF-related pathophysiology and explored how to correct the progress of VF and reduce the associated damage via a feasible first-aid strategy [4,7,19]. Recently, awareness and utilization of AEDs have unambiguously increased, but even so, the overall survival from CA remains low. Ample animal experiments and clinical trials support previous findings that showed improved survival to hospital discharge when CPR was provided for a prescribed time period before defibrillation rather than an immediate shock approach in patients with OHCA due to VF [13,20,21]. Moreover, as mentioned in a section of recent guidelines of the European Resuscitation Council, patients failing to receive early defibrillation can still benefit from effective chest compression provided by bystanders than those without CPR, although averaging 3% to 4% decline in survival per minute delay to defibrillation [16]. Meanwhile, assessment of the success of defibrillation is also indispensable to the process of CPR of sudden cardiac arrest resulting from VF. Most recently, a study has proposed that VF waveform measures combined with prior shock outcome may make possible prediction of defibrillation success during CPR [22].
TTM, also known as therapeutic hypothermia, was a new treatment concept first proposed by Holzer in 2010 [23]. Throughout the ensuing decade, TTM has been identified as a therapeutic intervention to limit neurologic injury after a patient’s resuscitation from CA, and it gradually became a central point of PCAS care research owing to concerns arising from equal outcomes from 2 clinical studies that used profoundly distinct target temperature levels [24]. In addition, a notable divergence has been identified via meta-analyses. Specifically, more recent meta-analyses showed that TTM may not improve mortality or neurological outcomes in postarrest survivors, while the great majority of previous studies indicated consistency with current best medical practice as recommended by international resuscitation guidelines [25–28]. Nevertheless, most current guidelines persist in recommending that all adult comatose survivors of OHCA with an initial shockable cardiac rhythm should receive TTM with a selected and constant temperature between 32°C and 36°C [3,29,30]. Hence, employing therapeutic hypothermia as a standard of care strategy of postarrest care in survivors may need to be reevaluated by more persuasive research evidence in the years to come.
The subtle relationship between palliative care and CPR, as an extremely controversial ethical issue, began to be explored more deeply and to provoke ongoing debate early in the 21st century. Despite palliative care and CPR appearing to be incompatible and mutually exclusive, the related national council and association of palliative medicine guidelines have stated that CPR is relevant in palliative care if the quality of a patient’s life could be promoted [31]. A review published in 2013 concluded that CPR is futile for in-hospital cancer patients with widespread incurable disease and poor performance status, and there is a trend for survival to decline with increasing extent of the cancer disease [32]. In addition, as the “do not attempt cardiopulmonary resuscitation” decisions have become embedded into clinical practice in the United Kingdom, recent studies concentrate more on the decisive role of patients’ autonomy on decision making, which is especially prominent in this policy [33–35]. Consequently, ongoing research is laying further stress on the feasibility of CPR in light of different populations in palliative care clinical practice.
Venoarterial ECMO, which evolved as a salvage therapeutic tool in CPR situations refractory to medical treatment including ECMO and cardiopulmonary bypass and is referred to as extracorporeal cardiac life support (ECLS) or extracorporeal cardiopulmonary resuscitation (ECPR), has been applied to striving for additional time to treat reversible underlying causes of CA over the past years, especially in patients with OHCA [5,36–38]. Moreover, Matsuoka et al. [39] recently conducted a population-based cohort study and clearly showed that hospitals’ ECPR capabilities are associated with favorable neurologic outcomes in OHCA patients who had refractory VF or pulseless ventricular tachycardia. This positive result has been demonstrated in many other meta-analyses [40–42] and a current case report [43]. However, in a nationally representative cross-sectional study, researchers found that patients hospitalized with CA who received ECMO had significantly higher mortality than those who did not [44]. This was no doubt different from the outcomes reported in studies on OHCA and IHCA. Thus, in the near future, conducting more high-quality evidence RCTs to identify the actual prognosis and survival of patients for whom ECMO is used, regardless of OHCA or IHCA, might be the new research focus of CPR treatments driven by emerging extracorporeal technologies.
In addition to the keywords mentioned above, sepsis/septic shock-associated CA and brain injury, which are always likely to have a worse prognosis than CA without sepsis, are also drawing increased attention. As early as 2011, sepsis was considered to be a potential prearrest predictor of mortality after IHCA in a meta-analysis, even though many broad-scale studies have not demonstrated prearrest sepsis as a predisposing factor for IHCA, and epidemiological data on sepsis-associated CA are limited [45,46]. Hereafter, aiming to describe the prearrest period in severe sepsis and septic shock more clearly and in greater detail, a more representative experimental swine model of human CA and CPR has been successfully made [47]. In addition, an increasing number of research studies have begun to focus on the long-term survival rate after a prearrest sepsis and multiorgan dysfunction inducing IHCA, and conclusions are in accordance with short-term outcomes [48–50]. Nevertheless, owing to the complexity of a combined effect generated by the pathophysiology of ongoing septic shock and PCAS and the higher rates of mortality with sepsis-associated IHCA, high-quality CPR and other traditional interventions or care are insufficient. More research should target sepsis-related pathophysiology before, during, and after CA in order to improve patient outcomes [46].
Interestingly, either severe sepsis or PCAS can lead to systemic inflammation or ischemia-reperfusion injury and finally cause some extent of brain injury, even developing into irreversible damage or brain death [46,51]. Meanwhile, a bibliometric analysis spanning 25 years has shown that
Conclusions
STRENGTHS AND LIMITATIONS:
Our study is the first bibliometric analysis specifically on CPR research activities. In contrast with traditional analyses, our analysis, which was based on professional bibliometric software, displays a better status of CPR research hotspots and trends, despite some limitations. First, only original articles and reviews were included. Second, some words were counted more than once because of their multiple expressions. Finally, as a result of the highly cited guidelines in the field of CPR, the accuracy of top co-cited authors and their articles was inevitably reduced.
Figures
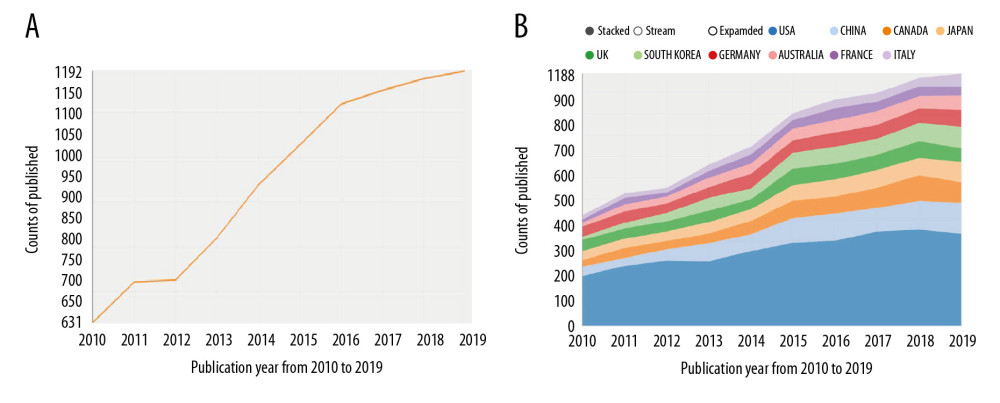 Figure 1. The number and linear growth trends of academic publications (A) and the top 10 countries/regions (B) for cardiopulmonary resuscitation research from 2010 to 2019.
Figure 1. The number and linear growth trends of academic publications (A) and the top 10 countries/regions (B) for cardiopulmonary resuscitation research from 2010 to 2019. 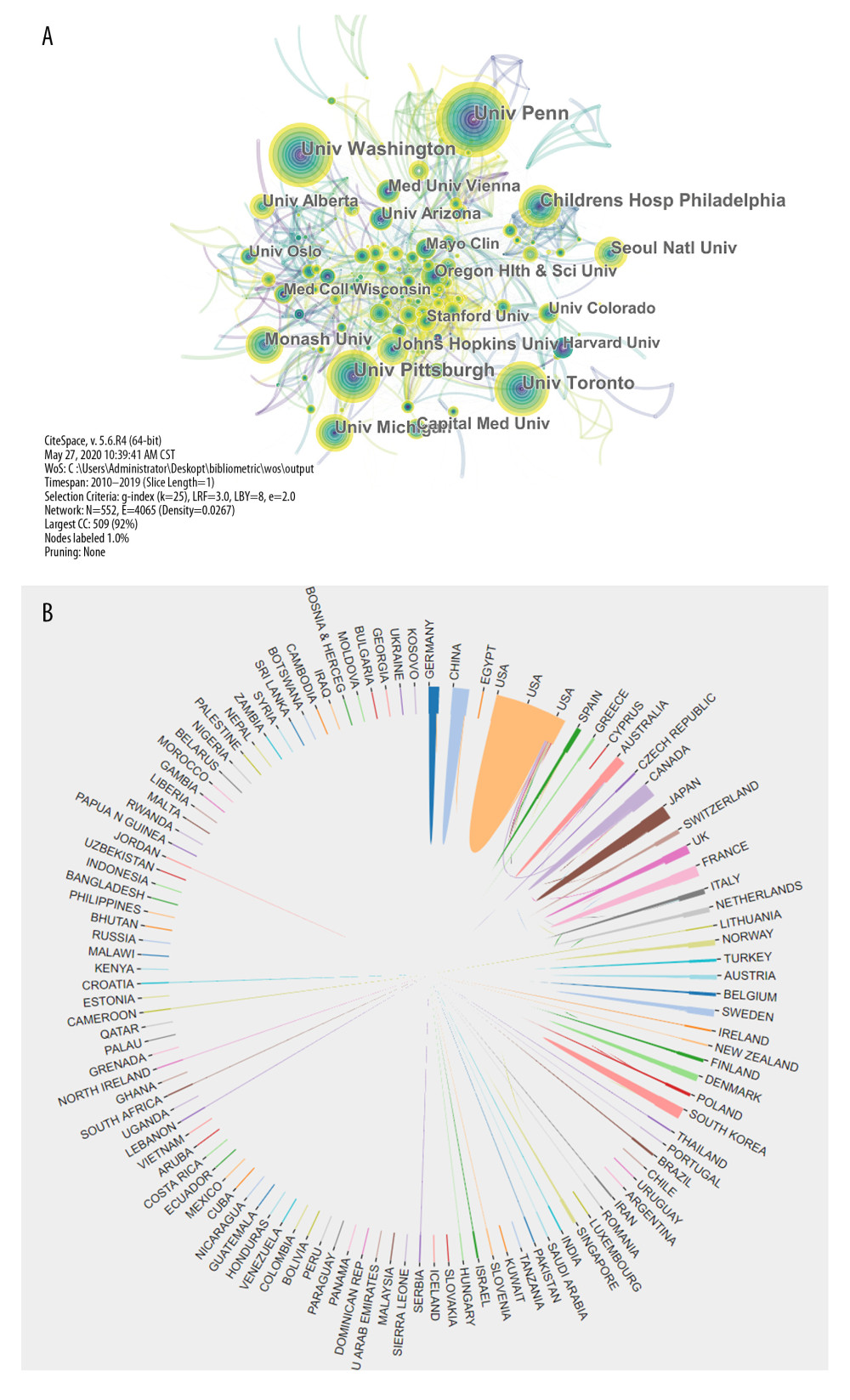 Figure 2. The interagency network that engaged in cardiopulmonary resuscitation research (A) and the collaboration network map of countries/regions (B).
Figure 2. The interagency network that engaged in cardiopulmonary resuscitation research (A) and the collaboration network map of countries/regions (B). 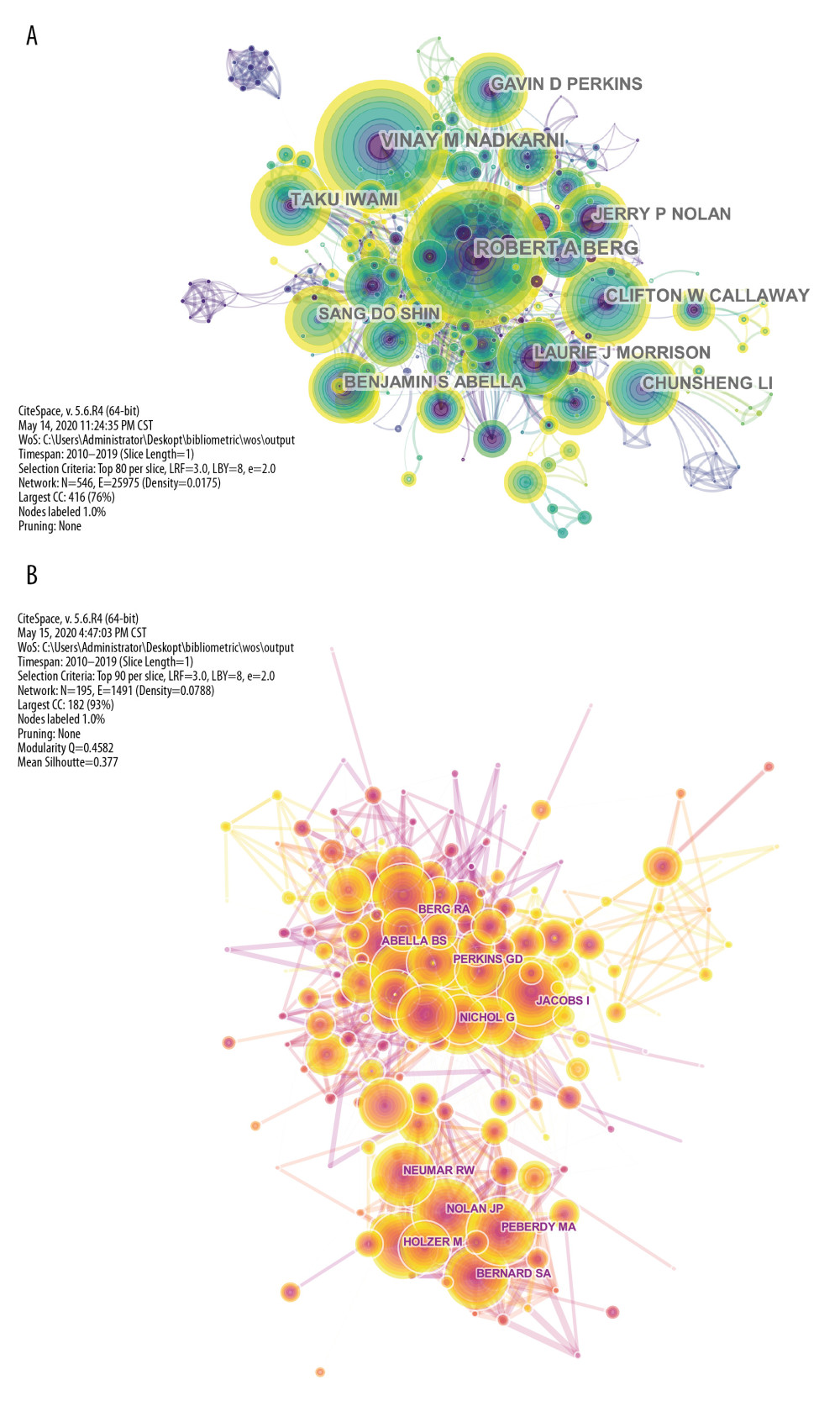 Figure 3. The network map of the most productive authors (A) and the most frequently cited authors (B) who participated in cardiopulmonary resuscitation research.
Figure 3. The network map of the most productive authors (A) and the most frequently cited authors (B) who participated in cardiopulmonary resuscitation research. 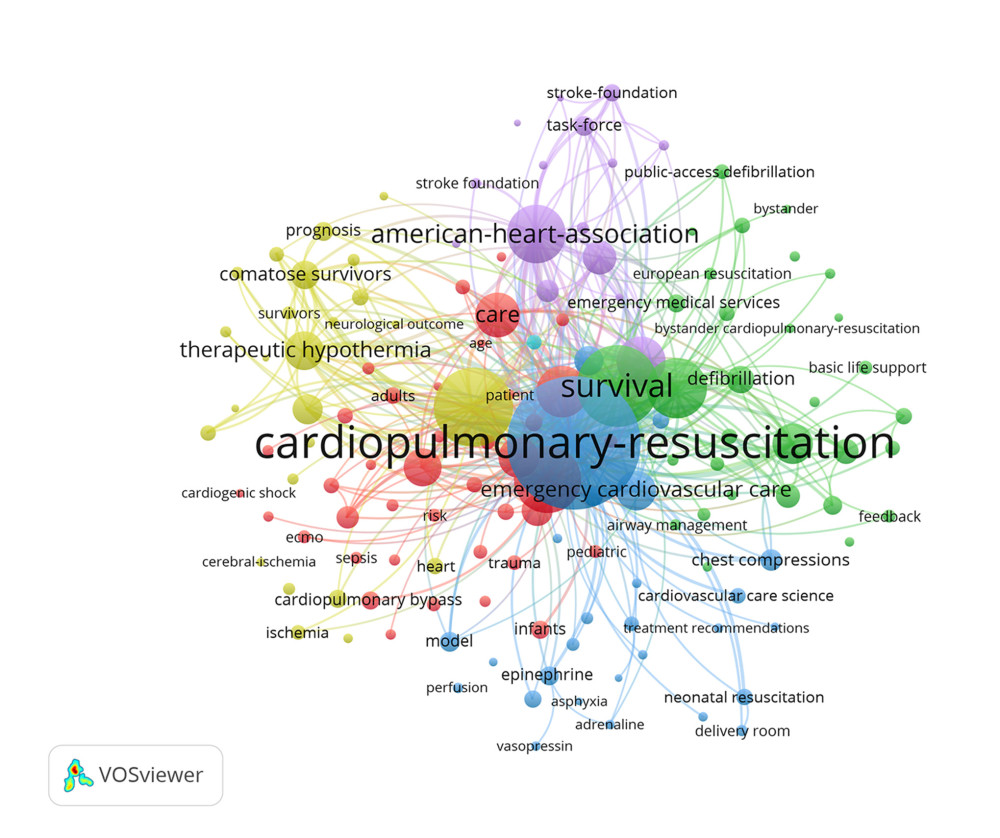 Figure 4. The network map of keyword clustering showed 256 keywords from a total of 17 093 samples with a minimum of 60 occurrences and classified into 6 clusters.
Figure 4. The network map of keyword clustering showed 256 keywords from a total of 17 093 samples with a minimum of 60 occurrences and classified into 6 clusters. 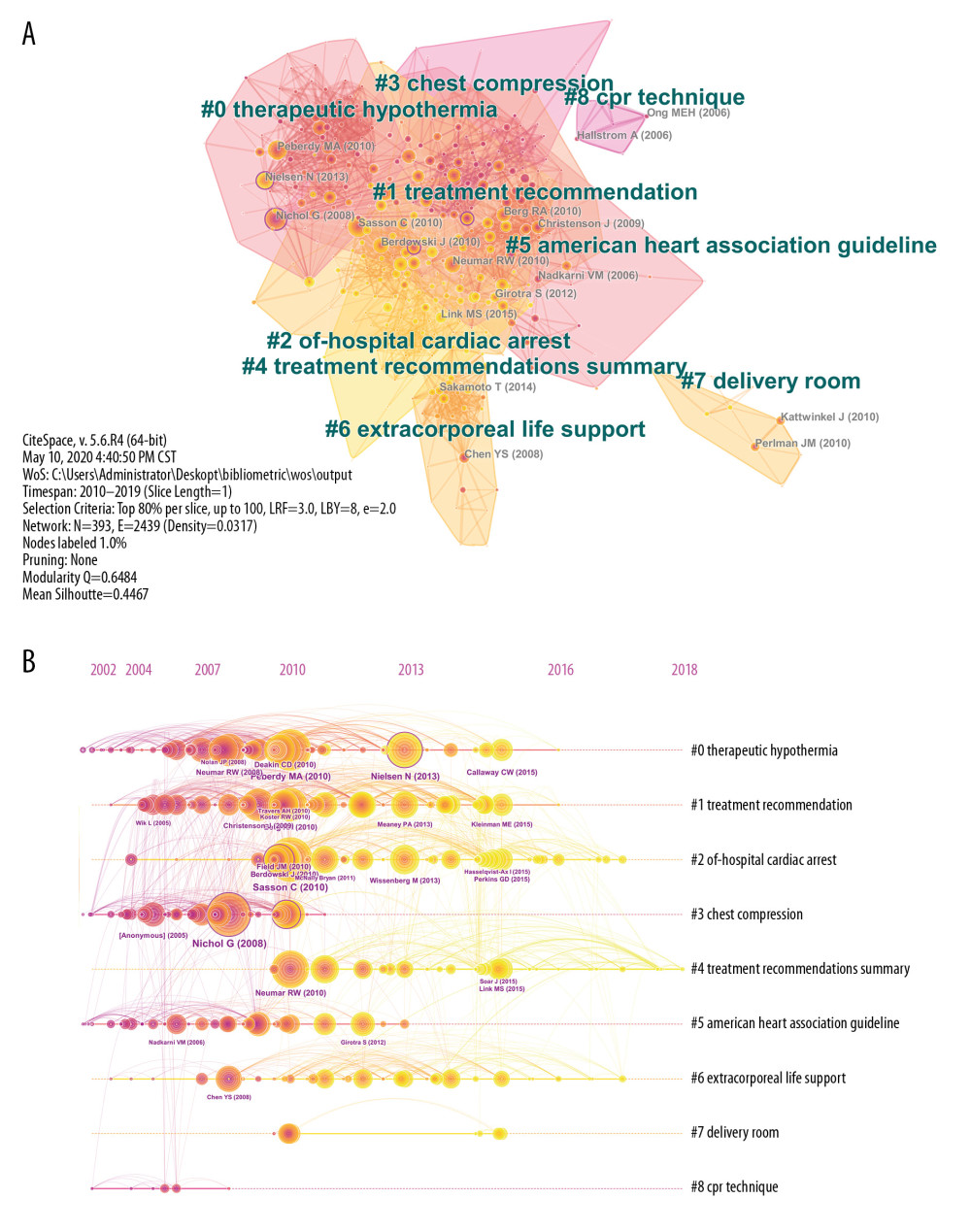 Figure 5. The clustered network map of co-cited references on cardiopulmonary resuscitation research (A) and the timeline view of co-citation clusters with their cluster labels on the right (B).
Figure 5. The clustered network map of co-cited references on cardiopulmonary resuscitation research (A) and the timeline view of co-citation clusters with their cluster labels on the right (B). 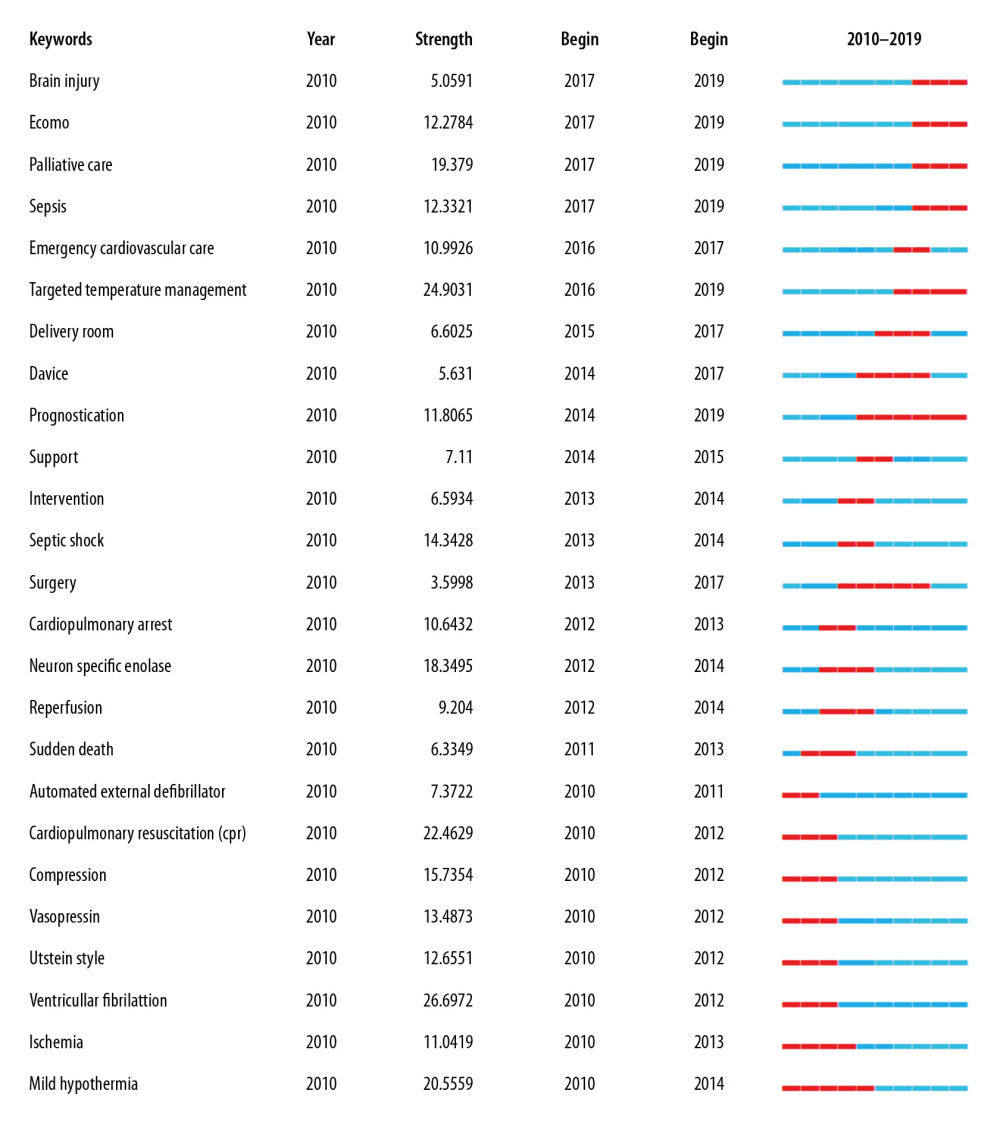 Figure 6. Keywords with the strongest citation bursts in original articles on cardiopulmonary resuscitation research activities published from 2010 to 2019.
Figure 6. Keywords with the strongest citation bursts in original articles on cardiopulmonary resuscitation research activities published from 2010 to 2019. Tables
Table 1. The top 10 countries/regions and institutions contributing to publications in cardiopulmonary resuscitation research.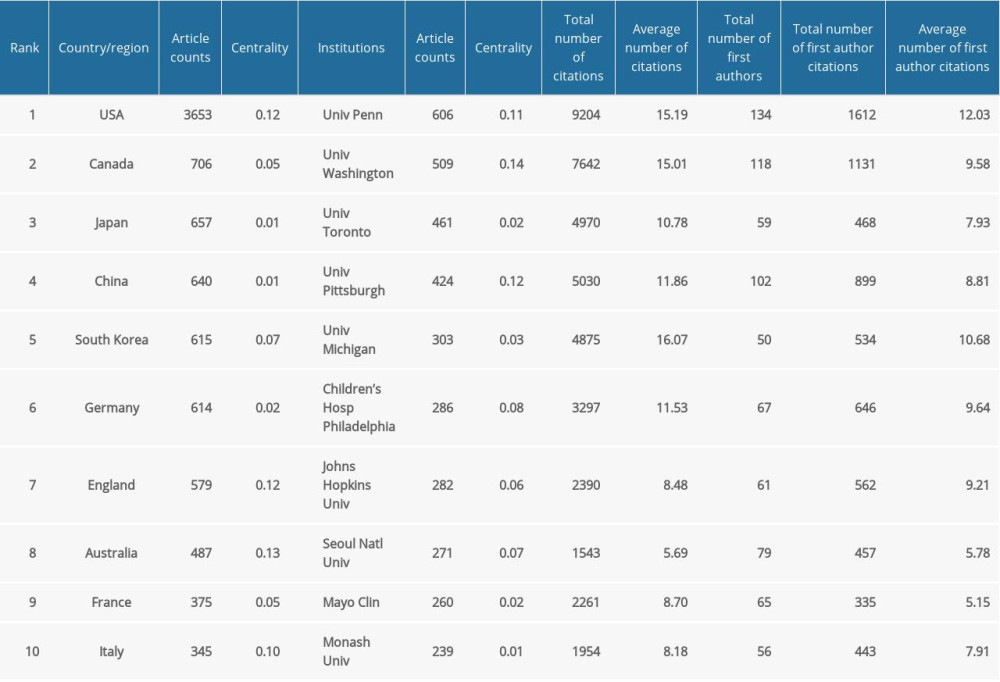 Table 2. The top 10 most active journals publishing articles in cardiopulmonary resuscitation research (sorted by count).
Table 2. The top 10 most active journals publishing articles in cardiopulmonary resuscitation research (sorted by count). Table 3. The top 10 most productive authors and co-cited authors contributed to publications in cardiopulmonary resuscitation research (sorted by count).
Table 3. The top 10 most productive authors and co-cited authors contributed to publications in cardiopulmonary resuscitation research (sorted by count). Table 4. The top 10 co-cited authors and their co-cited articles (sorted by cited frequency).
Table 4. The top 10 co-cited authors and their co-cited articles (sorted by cited frequency).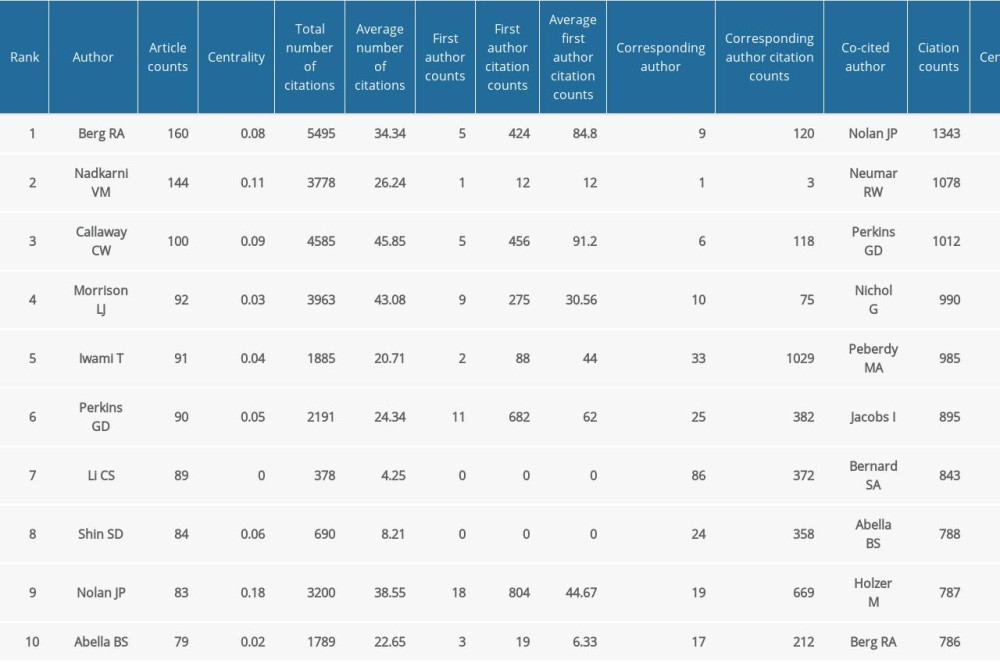
References
1. Andersen LW, Holmberg MJ, Berg KM, In-hospital cardiac arrest: A review: JAMA, 2019; 321(12); 1200-10
2. Myat A, Song K-J, Rea T, Out-of-hospital cardiac arrest: Current concepts: Lancet, 2018; 391(10124); 970-79
3. Hassager C, Nagao K, Hildick-Smith D, Out-of-hospital cardiac arrest: In-hospital intervention strategies: Lancet, 2018; 391(10124); 989-98
4. Harris AW, Kudenchuk PJ, Cardiopulmonary resuscitation: The science behind the hands: Heart, 2018; 104(13); 1056-61
5. Link MS, Berkow LC, Kudenchuk PJ, Part 7: Adult advanced cardiovascular life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care [published correction appears in Circulation. 2015 Dec 15;132(24): e385]: Circulation, 2015; 132(18 Suppl 2); S444-64
6. Panchal AR, Berg KM, Hirsch KG, 2019 American Heart Association focused update on advanced cardiovascular life support: Use of advanced airways, vasopressors, and extracorporeal cardiopulmonary resuscitation during cardiac arrest: An update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care: Circulation, 2019; 140(24); e881-94
7. Nolan JP, Hazinski MF, Aickin R, Part 1: Executive summary: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: Resuscitation, 2015; 95; e1-31
8. Nassar BS, Kerber R, Improving CPR performance: Chest, 2017; 152(5); 1061-69
9. Thompson DF, Walker CK, A descriptive and historical review of bibliometrics with applications to medical sciences: Pharmacotherapy, 2015; 35(6); 551-59
10. Dippenaar N, Watermeyer MJ, Tchouambou Simo NC, The top 100 cited articles published on cardiopulmonary resuscitation: Resuscitation, 2017; 114; e13-14
11. Freeman LC, Centrality in social networks conceptual clarification: Social Networks, 1978; 1(3); 215-39
12. Abella BS, Alvarado JP, Myklebust H, Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest: JAMA, 2005; 293(3); 305-10
13. Nichol G, Thomas E, Callaway CW, Regional variation in out-of-hospital cardiac arrest incidence and outcome: JAMA, 2008; 300(12); 1423-31
14. Neumar RW, Nolan JP, Adrie C, Post-cardiac arrest syndrome: Epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council: Circulation, 2008; 118(23); 2452-83
15. Peberdy MA, Callaway CW, Neumar RW, Part 9: Post-cardiac arrest care: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care: Circulation, 2010; 122(18 Suppl 3); S768-86
16. Perkins GD, Handley AJ, Koster RW, European Resuscitation Council guidelines for resuscitation 2015: section 2. Adult basic life support and automated external defibrillation: Resuscitation, 2015; 95; 81-99
17. Neumar RW, Otto CW, Link MS, Part 8: Adult advanced cardiovascular life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care: Circulation, 2010; 122(18 Suppl 3); S729-67
18. Bell SM, Lam DH, Kearney K, Hira RS, Management of refractory ventricular fibrillation (prehospital and Emergency Department): Cardiol Clin, 2018; 36(3); 395-408
19. Eisenberg MS, Psaty BM, Cardiopulmonary resuscitation: Celebration and challenges: JAMA, 2010; 304(1); 87-88
20. Berg RA, Hilwig RW, Kern KB, Ewy GA, Precountershock cardiopulmonary resuscitation improves ventricular fibrillation median frequency and myocardial readiness for successful defibrillation from prolonged ventricular fibrillation: A randomized, controlled swine study: Ann Emerg Med, 2002; 40(6); 563-71
21. Cobb LA, Fahrenbruch CE, Walsh TR, Influence of cardiopulmonary resuscitation prior to defibrillation in patients with out-of-hospital ventricular fibrillation: JAMA, 1999; 281(13); 1182-88
22. Coult J, Kwok H, Sherman L, Ventricular fibrillation waveform measures combined with prior shock outcome predict defibrillation success during cardiopulmonary resuscitation: J Electrocardiol, 2018; 51(1); 99-106
23. Holzer M, Targeted temperature management for comatose survivors of cardiac arrest: N Engl J Med, 2010; 363(13); 1256-64
24. Silverman MG, Scirica BM, Cardiac arrest and therapeutic hypothermia: Trends Cardiovasc Med, 2016; 26(4); 337-44
25. Kalra R, Arora G, Patel N, Targeted temperature management after cardiac arrest: Systematic review and meta-analyses: Anesth Analg, 2018; 126(3); 867-75
26. Lindsay PJ, Buell D, Scales DC, The efficacy and safety of pre-hospital cooling after out-of-hospital cardiac arrest: A systematic review and meta-analysis: Crit Care, 2018; 22(1); 66
27. Arrich J, Holzer M, Havel C, Hypothermia for neuroprotection in adults after cardiopulmonary resuscitation: Cochrane Database Syst Rev, 2016; 2(2); CD004128
28. Arrich J, Holzer M, Herkner H, Müllner M, Cochrane corner: Hypothermia for neuroprotection in adults after cardiopulmonary resuscitation: Anesth Analg, 2010; 110(4); 1239
29. Callaway CW, Donnino MW, Fink EL, Part 8: post-cardiac arrest care: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care: Circulation, 2015; 132(18 Suppl 2); S465-82
30. Donnino MW, Andersen LW, Berg KM, Temperature management after cardiac arrest: An advisory statement by the Advanced Life Support Task Force of the International Liaison Committee on Resuscitation and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation: Circulation, 2015; 132(25); 2448-56
31. Willard C, Cardiopulmonary resuscitation for palliative care patients: A discussion of ethical issues: Palliat Med, 2000; 14(4); 308-312
32. Kjørstad OJ, Haugen DF, Cardiopulmonary resuscitation in palliative care cancer patients: Tidsskr Nor Laegeforen, 2013; 133(4); 417-21
33. Low C, Finucane A, Mason B, Spiller J, Palliative care staff’s perceptions of do not attempt cardiopulmonary resuscitation discussions: Int J Palliat Nurs, 2014; 20(7); 327-33
34. Taubert M, Norris J, Edwards S, Snow V, Finlay IG, Talk CPR – a technology project to improve communication in do not attempt cardiopulmonary resuscitation decisions in palliative illness: BMC Palliat Care, 2018; 17(1); 118
35. Hall CC, Lugton J, Spiller JA, Carduff E, CPR decision-making conversations in the UK: An integrative review: BMJ Support Palliat Care, 2019; 9(1); 1-11
36. Mosier JM, Kelsey M, Raz Y, Extracorporeal membrane oxygenation (ECMO) for critically ill adults in the emergency department: History, current applications, and future directions: Crit Care, 2015; 19; 431
37. Latimer AJ, McCoy AM, Sayre MR, Emerging and future technologies in out-of-hospital cardiac arrest care: Cardiol Clin, 2018; 36(3); 429-41
38. Dennis M, Buscher H, Gattas D, Prospective observational study of mechanical cardiopulmonary resuscitation, extracorporeal membrane oxygenation and early reperfusion for refractory cardiac arrest in Sydney: The 2CHEER study: Crit Care Resusc, 2020; 22(1); 26-34
39. Matsuoka Y, Ikenoue T, Hata N, Hospitals’ extracorporeal cardiopulmonary resuscitation capabilities and outcomes in out-of-hospital cardiac arrest: A population-based study: Resuscitation, 2019; 136; 85-92
40. Chen Z, Liu C, Huang J, Clinical efficacy of extracorporeal cardiopulmonary resuscitation for adults with cardiac arrest: Meta-analysis with trial sequential analysis: Biomed Res Int, 2019; 2019 6414673
41. Cardarelli MG, Young AJ, Griffith B, Use of extracorporeal membrane oxygenation for adults in cardiac arrest (E-CPR): A meta-analysis of observational studies: ASAIO J, 2009; 55(6); 581-86
42. Kim SJ, Kim HJ, Lee HY, Comparing extracorporeal cardiopulmonary resuscitation with conventional cardiopulmonary resuscitation: A meta-analysis: Resuscitation, 2016; 103; 106-16
43. Riera J, Argudo E, Ruiz-Rodríguez JC, Full neurological recovery 6 h after cardiac arrest due to accidental hypothermia: Lancet, 2020; 395(10236); e89
44. Patel JK, Meng H, Qadeer A, Parikh PB, Impact of extracorporeal membrane oxygenation on mortality in adults with cardiac arrest: Am J Cardiol, 2019; 124(12); 1857-61
45. Ebell MH, Afonso AM, Pre-arrest predictors of failure to survive after in-hospital cardiopulmonary resuscitation: A meta-analysis: Fam Pract, 2011; 28(5); 505-15
46. Morgan RW, Fitzgerald JC, Weiss SL, Sepsis-associated in-hospital cardiac arrest: Epidemiology, pathophysiology, and potential therapies: J Crit Care, 2017; 40; 128-35
47. Chalkias A, Spyropoulos V, Koutsovasilis A, Cardiopulmonary arrest and resuscitation in severe sepsis and septic shock: A research model: Shock, 2015; 43(3); 285-91
48. Chao PW, Chu H, Chen YT, Long-term outcomes in critically ill septic patients who survived cardiopulmonary resuscitation: Crit Care Med, 2016; 44(6); 1067-74
49. Koivikko P, Arola O, Inkinen O, Tallgren M, One-year survival after inhospital cardiac arrest-does prearrest sepsis matter?: Shock, 2018; 50(1); 38-43
50. Galvagno SM, Outcomes following sepsis and cardiopulmonary resuscitation: Fare thee well or worse for wear?: Crit Care Med, 2016; 44(6); 1232-33
51. Schneider A, Albertsmeier M, Böttiger BW, Teschendorf PPost-resuscitation syndrome. Role of inflammation after cardiac arrest: Der Anaesthesist, 2012; 61(5); 424-36 [in German]
52. Ferhatoglu SY, Yapici N, A bibliometric analysis of the articles focusing on the subject of brain death published in Scientific Citation Index- expanded indexed journals: Analysis of 3487 articles published between 1995–2019: Transplant Proc, 2020; 52(3); 706-11
53. Geocadin RG, Callaway CW, Fink EL, Standards for studies of neurological prognostication in comatose survivors of cardiac arrest: A scientific statement from the American Heart Association: Circulation, 2019; 140(9); e517-42
54. Feng G, Jiang G, Li Z, Wang X, Prognostic value of electroencephalography (EEG) for brain injury after cardiopulmonary resuscitation: Neurol Sci, 2016; 37(6); 843-49
55. Welbourn C, Efstathiou N, How does the length of cardiopulmonary resuscitation affect brain damage in patients surviving cardiac arrest? A systematic review: Scand J Trauma Resusc Emerg Med, 2018; 26(1); 77
56. Kramer P, Miera O, Berger F, Schmitt K, Prognostic value of serum biomarkers of cerebral injury in classifying neurological outcome after paediatric resuscitation: Resuscitation, 2018; 122; 113-20
Figures
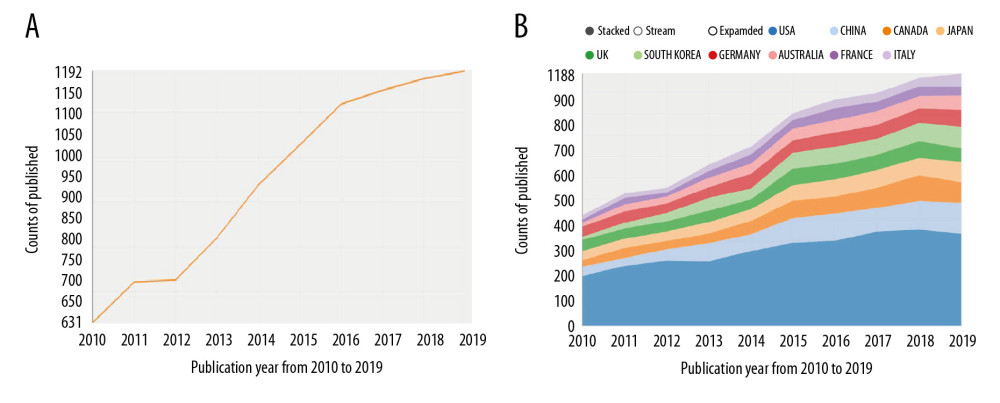 Figure 1. The number and linear growth trends of academic publications (A) and the top 10 countries/regions (B) for cardiopulmonary resuscitation research from 2010 to 2019.
Figure 1. The number and linear growth trends of academic publications (A) and the top 10 countries/regions (B) for cardiopulmonary resuscitation research from 2010 to 2019.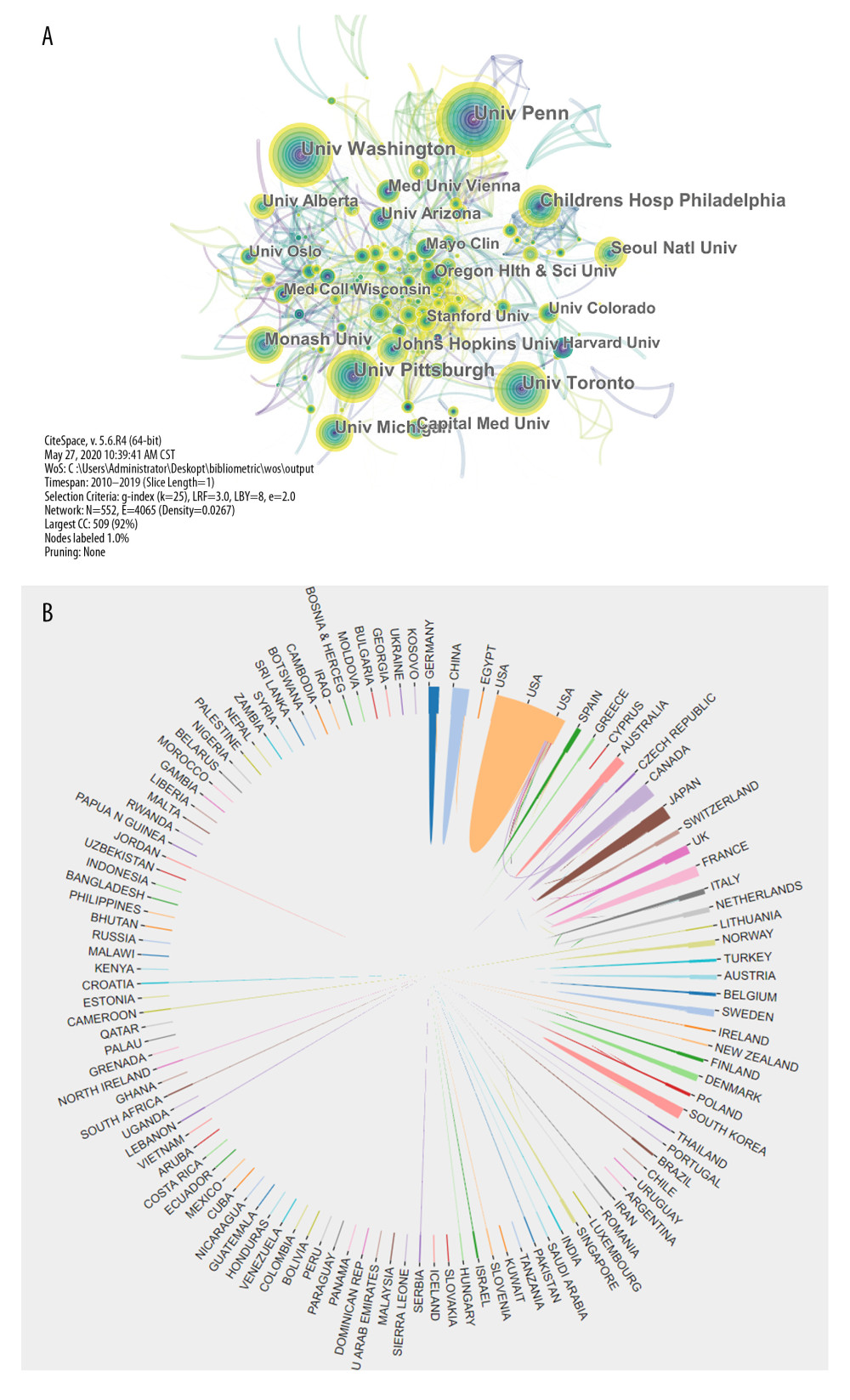 Figure 2. The interagency network that engaged in cardiopulmonary resuscitation research (A) and the collaboration network map of countries/regions (B).
Figure 2. The interagency network that engaged in cardiopulmonary resuscitation research (A) and the collaboration network map of countries/regions (B).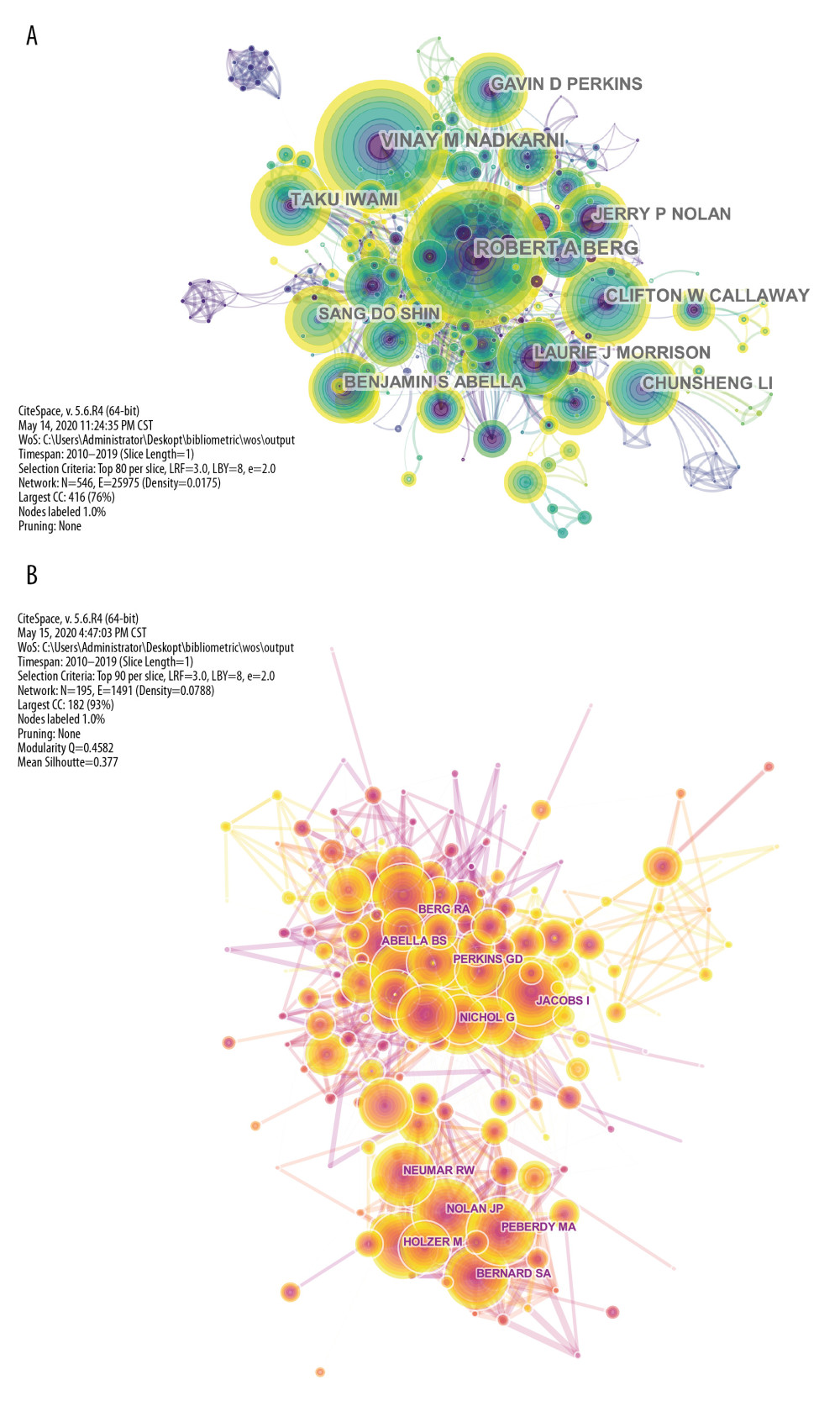 Figure 3. The network map of the most productive authors (A) and the most frequently cited authors (B) who participated in cardiopulmonary resuscitation research.
Figure 3. The network map of the most productive authors (A) and the most frequently cited authors (B) who participated in cardiopulmonary resuscitation research.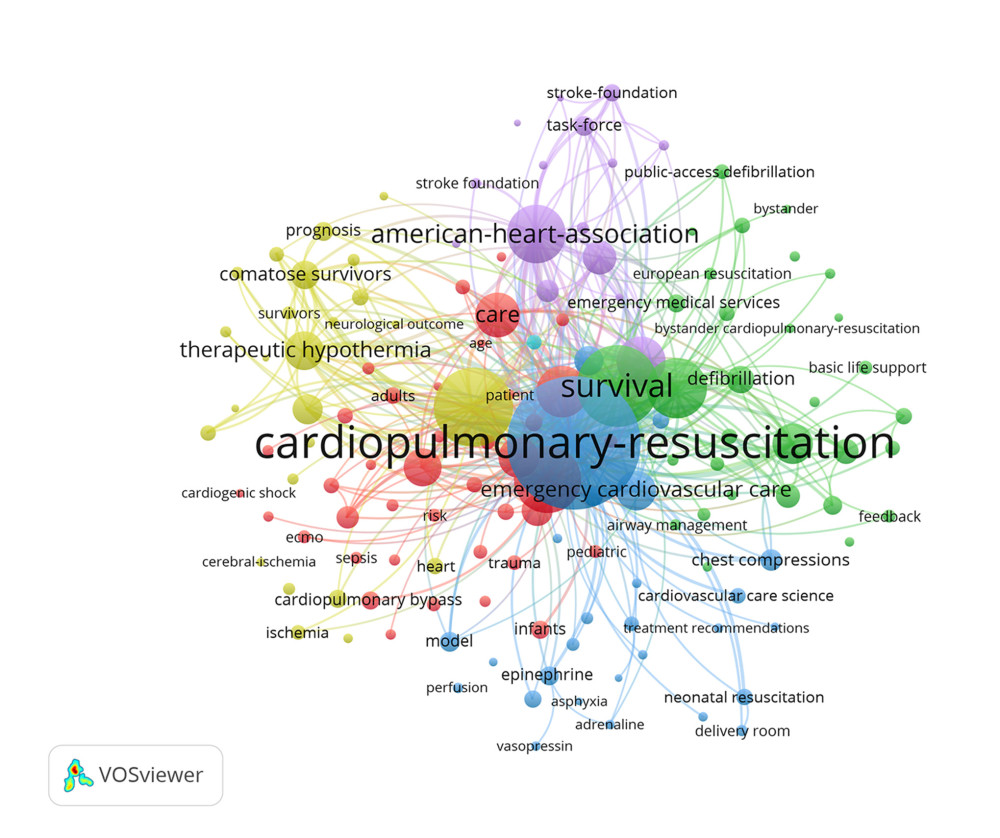 Figure 4. The network map of keyword clustering showed 256 keywords from a total of 17 093 samples with a minimum of 60 occurrences and classified into 6 clusters.
Figure 4. The network map of keyword clustering showed 256 keywords from a total of 17 093 samples with a minimum of 60 occurrences and classified into 6 clusters.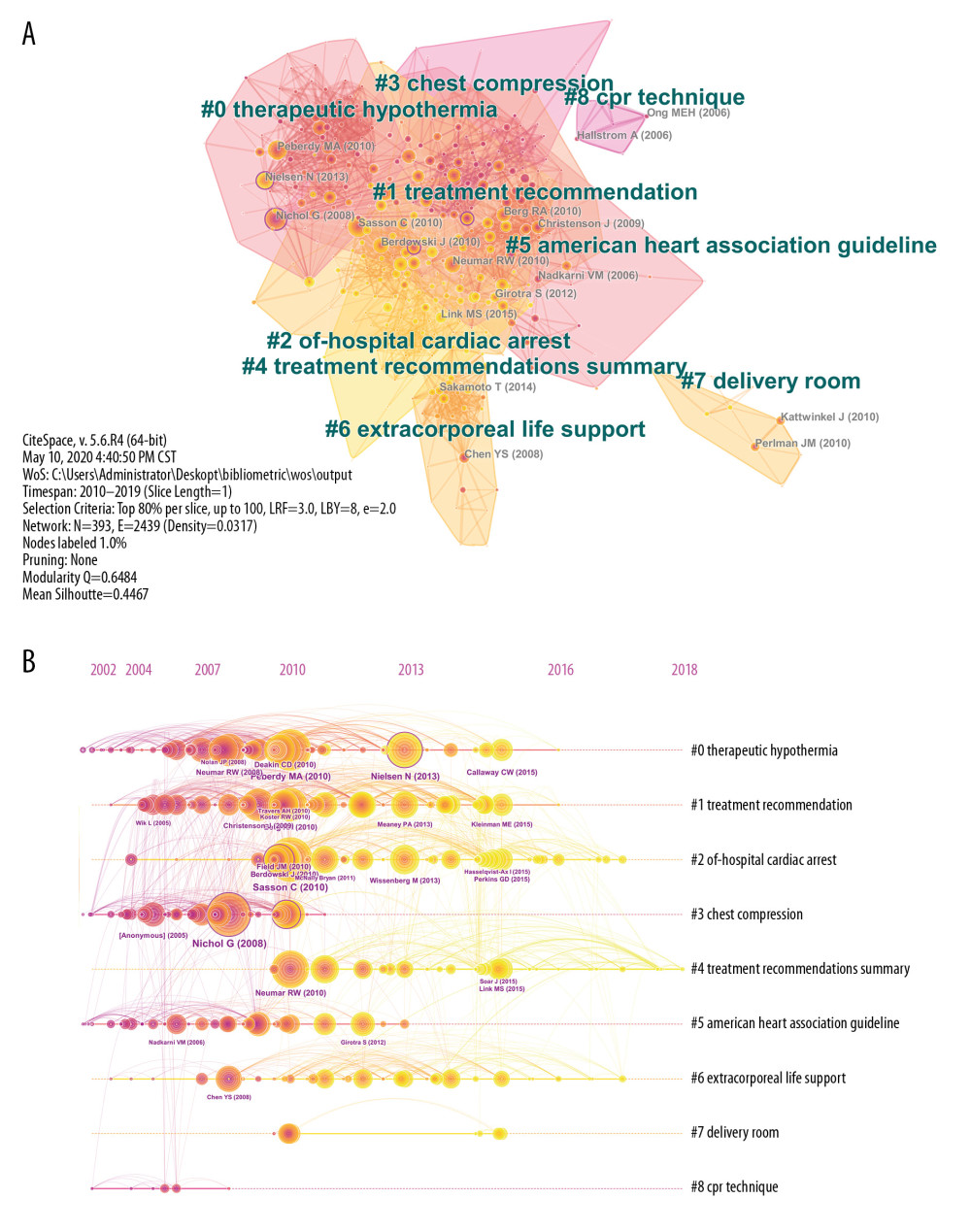 Figure 5. The clustered network map of co-cited references on cardiopulmonary resuscitation research (A) and the timeline view of co-citation clusters with their cluster labels on the right (B).
Figure 5. The clustered network map of co-cited references on cardiopulmonary resuscitation research (A) and the timeline view of co-citation clusters with their cluster labels on the right (B).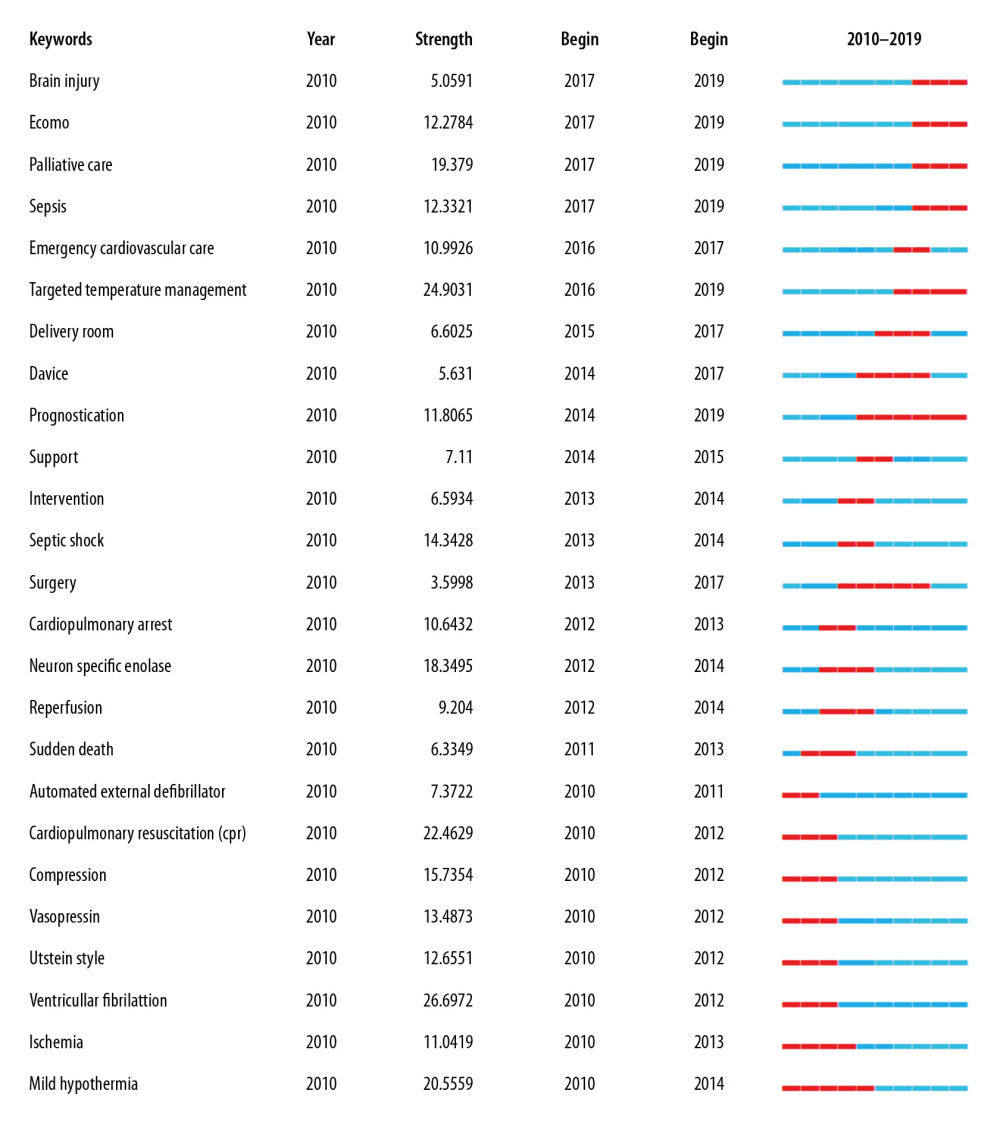 Figure 6. Keywords with the strongest citation bursts in original articles on cardiopulmonary resuscitation research activities published from 2010 to 2019.
Figure 6. Keywords with the strongest citation bursts in original articles on cardiopulmonary resuscitation research activities published from 2010 to 2019. Tables
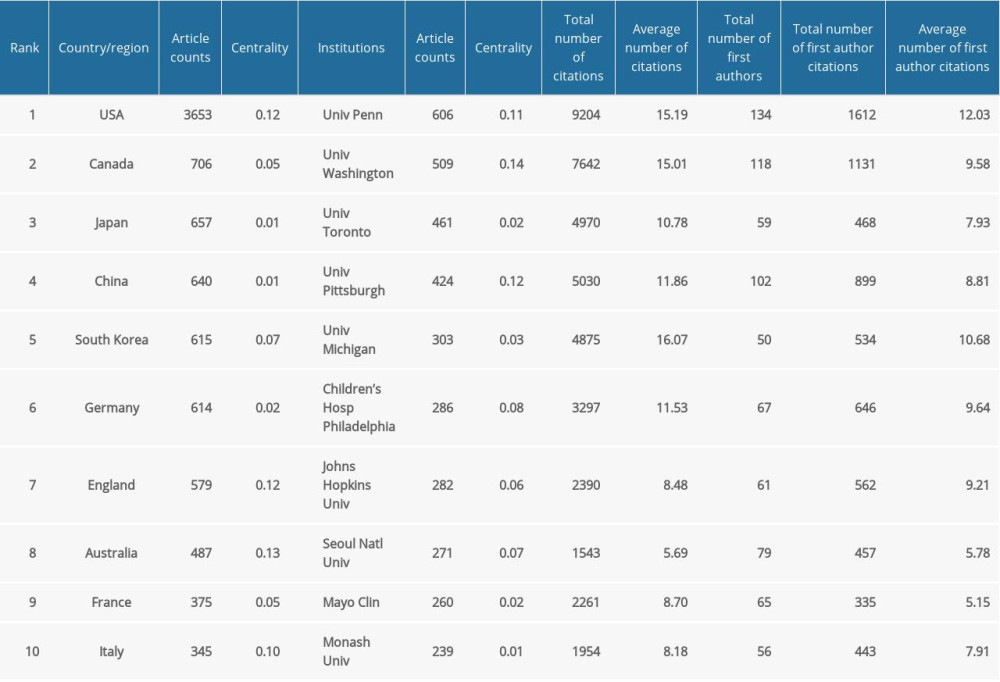 Table 1. The top 10 countries/regions and institutions contributing to publications in cardiopulmonary resuscitation research.
Table 1. The top 10 countries/regions and institutions contributing to publications in cardiopulmonary resuscitation research. Table 2. The top 10 most active journals publishing articles in cardiopulmonary resuscitation research (sorted by count).
Table 2. The top 10 most active journals publishing articles in cardiopulmonary resuscitation research (sorted by count). Table 3. The top 10 most productive authors and co-cited authors contributed to publications in cardiopulmonary resuscitation research (sorted by count).
Table 3. The top 10 most productive authors and co-cited authors contributed to publications in cardiopulmonary resuscitation research (sorted by count).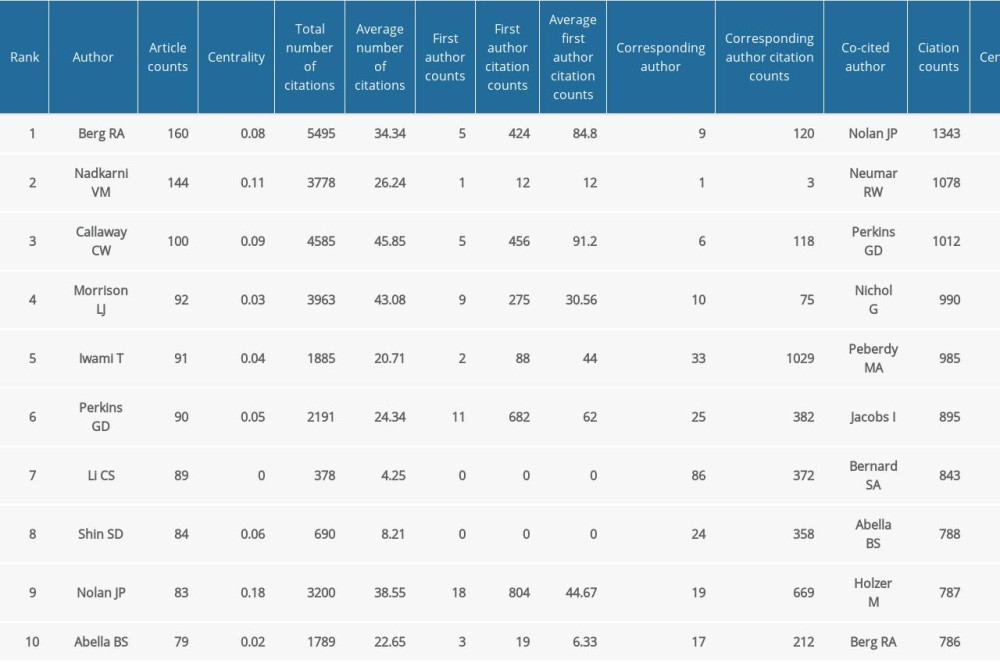 Table 4. The top 10 co-cited authors and their co-cited articles (sorted by cited frequency).
Table 4. The top 10 co-cited authors and their co-cited articles (sorted by cited frequency).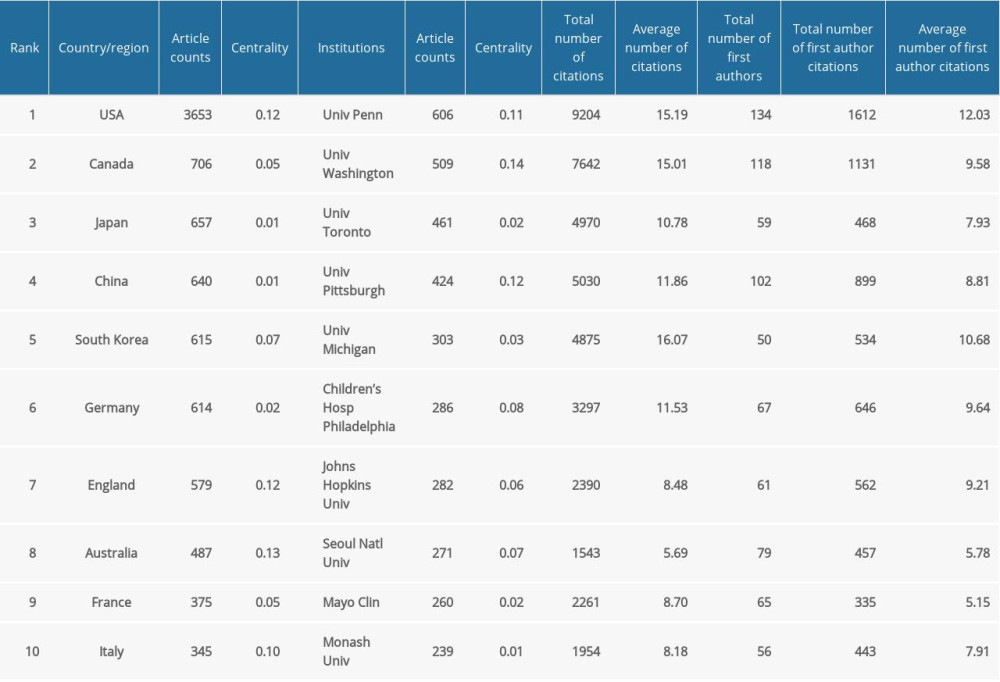 Table 1. The top 10 countries/regions and institutions contributing to publications in cardiopulmonary resuscitation research.
Table 1. The top 10 countries/regions and institutions contributing to publications in cardiopulmonary resuscitation research. Table 2. The top 10 most active journals publishing articles in cardiopulmonary resuscitation research (sorted by count).
Table 2. The top 10 most active journals publishing articles in cardiopulmonary resuscitation research (sorted by count). Table 3. The top 10 most productive authors and co-cited authors contributed to publications in cardiopulmonary resuscitation research (sorted by count).
Table 3. The top 10 most productive authors and co-cited authors contributed to publications in cardiopulmonary resuscitation research (sorted by count).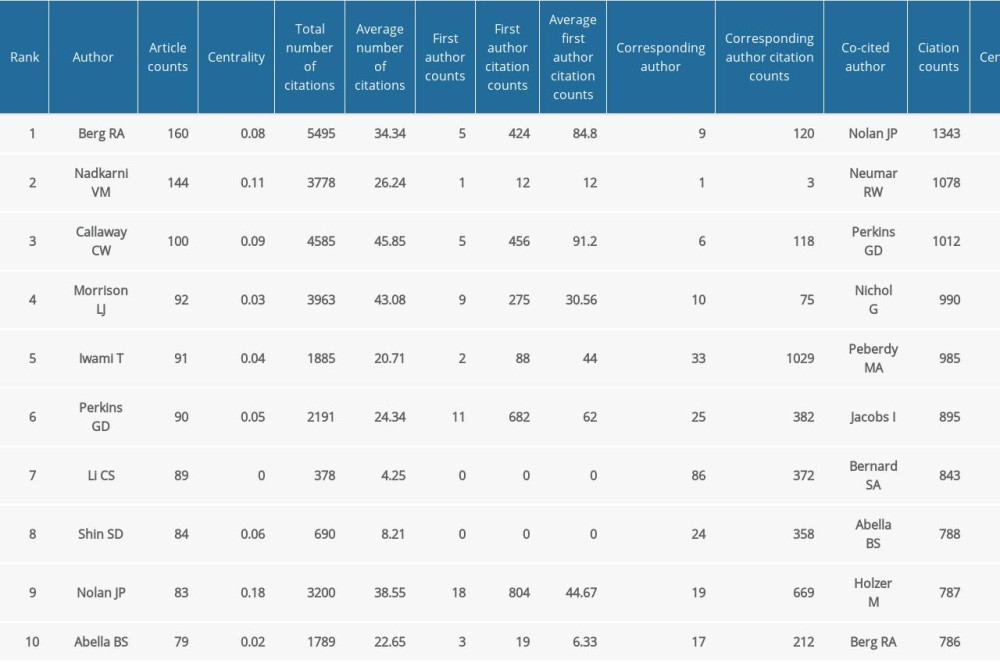 Table 4. The top 10 co-cited authors and their co-cited articles (sorted by cited frequency).
Table 4. The top 10 co-cited authors and their co-cited articles (sorted by cited frequency). In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








