25 January 2021: Clinical Research
Bronchiolitis Associated with Infection in Infants in Foshan China: An Epidemiologic Study
Cheng Chen1AE, Chunwang Lin1AEG*, Xiangming Zhong2AB, Diemei Wen1BD, Jingping Zhang1CDDOI: 10.12659/MSM.928148
Med Sci Monit 2021; 27:e928148
Abstract
BACKGROUND: Bronchiolitis is common in infants under 2 years of age. Most infections are caused by respiratory syncytial virus (RSV), but the importance of Mycoplasma pneumoniae (MP) in the etiology of bronchiolitis is unclear.
MATERIAL AND METHODS: We investigated the clinical characteristics of bronchiolitis caused by MP in 79 infants admitted to Shunde Women’s and Children’s Hospital of Guangdong Medical University and Sanshui Women’s and Children’s Healthcare Hospital from January 2016 to December 2018. Infection with MP was confirmed by the presence of serum immunoglobulin M.
RESULTS: The peak detection rates of MP in the years 2016, 2017, and 2018 were 19.2%, 21.3%, and 24.0%, respectively. In each year, the peak of MP infections occurred during June and July. MP-associated bronchiolitis was mainly seen in infants from 6 to 12 months of age. Compared with RSV-associated bronchiolitis, the age of patients with bronchiolitis associated with MP was significantly older and they had a shorter hospital stay (all P<0.01 or P<0.05).
CONCLUSIONS: Our study indicated that MP is an important cause of bronchiolitis, with peaks of occurrence during June and July every year. Pulmonary interstitial infiltration was a characteristic of this infection. Azithromycin treatment can shorten the course of MP-associated bronchiolitis. Investigation of the epidemiological characteristics of pediatric MP-associated bronchiolitis can help diagnose and treat the disease correctly.
Keywords: Azithromycin, bronchiolitis, Epidemiology, Mycoplasma pneumoniae, Respiratory Syncytial Viruses, Epidemiologic Studies, Hospitalization, Infant, Infant, Newborn, Length of Stay, Pneumonia, Mycoplasma, Respiratory Syncytial Virus Infections
Background
Bronchiolitis is the most common lower respiratory tract disorder in infants. The most common pathogen found in patients with bronchiolitis is respiratory syncytial virus (RSV) [1,2]. Another common cause of respiratory tract infection in children is
It is difficult to culture MP, and infections are confirmed by polymerase chain reaction (PCR) gene amplification or serology. In recent years, bronchiolitis caused by MP has received increasing attention. A study of 211 infants with bronchiolitis reported an MP-positive rate of 7.1% in moderate or severe cases [10]. This is important evidence of an association between MP and bronchiolitis in infants.
The present study identified the clinical characteristics, seasonal distribution, and treatment of MP-associated bronchiolitis in infants in the subtropical city of Foshan, China.
Material and Methods
ETHICS STATEMENT:
This study conformed to the Helsinki Declaration regarding medical research involving the human body. The Ethics Committee of Affiliated Shunde Women’s and Children’s Hospital of Guangdong Medical University approved the study (No. Sdfy2015036). The parents of all study participants gave written informed consent before the study. All patient information was anonymized.
SUBJECTS AND DIAGNOSTIC CRITERIA:
This retrospective study investigated infantile patients with bronchiolitis from January 2016 to December 2018 at Shunde Women’s and Children’s Hospital of Guangdong Medical University and Sanshui Women’s and Children’s Healthcare Hospital. The study population (n=368) comprised 125, 122, and 121 patients with bronchiolitis treated in the years 2016, 2017, and 2018, respectively. Among them, bronchiolitis was associated with MP and RSV in 79 and 289 patients, respectively. Overall, there were 190 boys (51.6%) and 178 girls (48.4%), with average ages of 11 months (6–36 months) and 7.5 months (3–11 months).
For inclusion in this study, all patients met the following criteria [12]: aged 0–3 years; MP-immunoglobulin M (IgM) antibodies ≥1: 320, or positive respiratory virus antibody reaction; cough, wheezing, increased respiration, and/or fever; widespread double-lung wheezing revealed by physical examination; and chest computed tomography (CT) showing messy, reticular, high-density shadows appearing as mist in bilateral lungs with increased brightness. Patients with any of the following were excluded from this study: bronchial asthma, congenital heart disease, bronchopulmonary dysplasia, and cystic fibrosis.
BLOOD SPECIMEN COLLECTION:
The MP antibodies and respiratory virus antibodies were measured and interpreted in a blind manner. The measurement of the MP antibodies and respiratory virus antibody levels was fully automated. Blood samples of patients were obtained on admission to the hospital and/or after treatment. In brief, 2-mL venous blood samples were collected in a tube with K2-EDTA and routinely processed.
DETECTION OF MP ANTIBODY: Plasma MP antibodies (MP-IgM) were analyzed by an immune agglutination assay using a kit (Fujirebio, Tokyo, Japan). The experimental process was performed strictly in accordance with the instructions. Positive MP infection was defined as a single antibody titer of 1: 320 for MP-IgM [12].
DETECTION OF MONOCLONAL ANTIBODIES AGAINST RESPIRATORY VIRUSES:
Monoclonal antibodies against respiratory viruses were detected by direct immunofluorescence labeling. All assay kits were purchased from Chemicon (Billerica, USA) and included RSV, adenovirus, influenza virus A, influenza virus B, and parainfluenza virus (PIV) 1, 2, and 3.
THERAPY FOR BRONCHIOLITIS ASSOCIATED WITH MP:
The therapy for MP-associated bronchiolitis was the same as for MP pneumonia. Azithromycin was orally administered at 10 mg/kg/d for 6 consecutive days [12], and the remaining therapy was the same as for RSV-associated bronchiolitis.
STATISTICAL ANALYSES:
Statistical analyses were performed using SPSS version 20.0 statistical software (SPSS, Chicago, IL, USA). Continuous data are presented as mean±standard deviation. Lung wheezing and durations of fever, cough, rales, and hospitalization were analyzed using the
Results
DETECTION OF MP AND RESPIRATORY VIRUSES:
Pathogen antibodies were identified in 412 specimens. Specifically, respiratory syncytial virus (RSV) or MP was found in 289 (70.1%) and 79 patients (19.2%), respectively. Fewer patients were found with PIV 2 (16, 3.9%), influenza virus B (13, 3.2%), adenovirus (6, 1.5%), or PIV 3 (5, 1.2%). Influenza virus A and PIV 1 were found in 2 patients (0.5%) each. Patients with no detectable pathogens were excluded from the study.
PREVALENCE AND SEASONS OF MP AND RSV INFECTIONS FROM JANUARY 2016 TO DECEMBER 2018:
The Foshan region in China has a subtropical climate, which is defined as spring (March–May), summer (June–August), autumn (September–November), and winter (December–February), with an average annual temperature and humidity of 21.9°C and 77%, respectively. The peak of MP infection occurs in summer (June–August). The number of patients with bronchiolitis associated with MP in the years 2016, 2017, and 2018 were 24, 26, and 29, respectively, and the corresponding MP detection rates were 19.2%, 21.3%, and 24.0%, respectively.
The highest detection rates of MP were in June 2016 (41.6%), July 2017 (42.6%), and June 2018 (44.6%). Overall, there were 50 patients (63.3%) from June–July 2016 to June–July 2018, with peaks in successive years. The lowest MP-positive rates were observed each year between December and February.
The numbers of patients with bronchiolitis associated with RSV in the years 2016, 2017, and 2018, were 101, 96, and 92, respectively. The peaks of RSV infection occurred between April and May of any particular year. Specifically, the highest rates occurred in May 2016 (49.8%), April 2017 (51.6%), and April 2018 (52.2%). The lowest RSV-positive rates were observed between July and October of each year (Figure 1).
DISTRIBUTION OF MP INFECTION IN DIFFERENT YEARS:
Among all the patients, 42 were boys and 37 were girls, with a boy-to-girl ratio of 1.135: 1, without any significant sex difference. Among the 79 patients with bronchiolitis associated with MP, the youngest and oldest patients were 4 months and 3 years of age, respectively. The median age was 11 months (range, 4 months to 3 years). Fifteen patients (19.0%) were 4 or 5 months old, 38 (48.1%) were 6 months to 1 year, 21 (26.6%) were 1 to 2 years, and 5 (6.3%) were aged 2 to 3 years. Between January 2016 and December 2018, the numbers of patients with MP infection in the age groups 4 to 5 months and 6 to 12 months were significantly higher than that of other age groups (Figure 2).
CLINICAL CHARACTERISTICS OF PATIENTS WITH BRONCHIOLITIS ASSOCIATED WITH MP:
The clinical characteristics of patients with bronchiolitis associated with MP or RSV are shown in Table 1. Fever was recorded in 39 patients (49.4%), and the median fever duration was 3.0±1.50 h. Severe cough was a prominent symptom in 79 patients (100%); 11 patients (13.9%) had dyspnea, 6 (7.6%) had O2 saturation <90%, and 79 (100%) had wheezing. The white blood cell and thrombocyte counts were 8.6±1.7×109/L and 456±46.3×109/L, respectively. Thirty-one patients (39.2%) had thrombocytosis. C-reactive protein was 25.5±3.5 mg/L, and procalcitonin level was 0.16±0.08 ng/mL. Twenty-four patients (30.4%) had elevated creatine kinase isoenzyme (CK-MB), troponin I (CTnI), or both. Alanine aminotransferase (ALT) levels were elevated in 16 (20.3%) patients. All patients had abnormal chest X-ray findings, including 63 (79.7%) with pulmonary interstitial infiltration and 16 (20.3%) with emphysema.
CHARACTERISTICS OF MP- AND RSV-ASSOCIATED BRONCHIOLITIS:
The median ages of patients with MP- and RSV-associated bronchiolitis were 11 months and 7.5 months, respectively. Hyperpyrexia was more common in patients with bronchiolitis associated with MP, and cough was also more severe in this group. However, tachypnea was more common in patients with RSV infection than in those with MP infection, and SaO <90% was more common in patients with RSV infection (P<0.01). Moreover, these patients also had more severe disease (n=61), and 78% of them had prematurity with low birth weight (n=25) and/or <6 months old (n=54), as one of the factors or overlap. Increased C-reactive protein, procalcitonin, CK-MB, and CTnI levels were significantly more common in patients with MP infection than in those with RSV (all P<0.01 or P<0.05). Pulmonary interstitial infiltration was significantly more common in patients infected with MP than in those infected with RSV (P<0.01), with messy, reticular, high-density or a fuzzy (misty) appearance; it was found in 63 patients (79.8%) and 12 patients (4.15%), respectively (Figure 3A, 3B). Emphysema was significantly more common in RSV-associated bronchiolitis than in MP-associated bronchiolitis (P<0.01): emphysema was found in 238 patients (82.4%) and 16 patients (20.3%), respectively (Figure 3C).
CLINICAL OUTCOMES OF PATIENTS WITH MP- AND RSV-ASSOCIATED BRONCHIOLITIS:
The 2 groups differed significantly with regard to end of fever, cough, rales, and hospitalization (all P<0.05; Table 2). Specifically, in patients with MP- (RSV-) associated bronchiolitis, the time to end of fever was 3.0±1.5 h (2.1±0.8 h), time to cough cessation was 9.5±1.2 days (6.5±1.1 days), and time to disappearance of wheezing rales was 4.1±1.2 days (6.2±1.2 days); corresponding hospitalizations were 7.5 days (7.0–9.5 days) and 9.5 days (8.5–10.5 days), respectively.
Discussion
We investigated the clinical characteristics of bronchiolitis caused by MP in 79 infants admitted to Shunde Women’s and Children’s Hospital of Guangdong Medical University and Sanshui Women’s and Children’s Healthcare Hospital from January 2016 to December 2018. This study found that MP is an important causative pathogen of bronchiolitis in Foshan China, especially in children from 4 to 10 months of age, with seasonal peaks in summer, unlike in northern China and in higher-latitude countries. Pulmonary interstitial infiltration is the main imaging feature, unlike in RSV-associated bronchiolitis. Understanding the epidemiological characteristics of MP-associated bronchiolitis in children is helpful to determine the correct diagnosis and treatment.
In this study, MP was the second most common (after RSV) pathogen causing bronchiolitis, and the detection rate was 19.2%. This suggests the importance of MP as a pathogen causing bronchiolitis. MP was reported as an important pathogen in children with community-acquired pneumonia [13,14]. Two studies from Guangzhou and Suzhou in southern China reported that the rate of MP infection was 11.3% and 36.08%, respectively [14,15], and another study in 5 cities of southern and northern China reported that the rate of MP infection was 25.5% [16]. The present study showed an endemic peak of MP infection during the past 3 years in the population seeking medical treatment in hospitals, and it reached a level of 63.3% in June and July in the years 2016 to 2018. The epidemic pattern of MP infection is somewhat similar to that of other countries [5,17,18].
Our data showed that the positive rate of MP is highest in summer, with a peak prevalence between June and July each year, and the positive rate is very low in winter. This indicates that the epidemic season of MP in the Foshan region was summer. These results are consistent with the seasonal patterns reported in previous epidemiological studies by Ji et al. [19]. The present study showed that the infection rate of MP was positively correlated with air temperature. This is supported by a previous study in which a gradual increase in the rate of MP infections occurred as the environmental temperature rose [20,21]. Defilippi et al. [22] revealed that the first epidemic peak occurred in June, and the second epidemic peak was in December and January. Hadil et al. [23] reported that the peak of an MP epidemic occurred in autumn, with fewer patients in winter and spring. However, another study showed that MP infection rates were highest in winter [24], and Foy et al. [25] reported that there was no seasonal difference in the epidemiology of MP. Altogether, the above studies show that children may experience MP infection at any time of the year, but the epidemiology of MP varies by region and climate. In spring, RSV infection was more likely in children with bronchiolitis. In summer, MP infection is more likely in children with bronchiolitis. This is useful for the diagnosis and treatment of children with bronchiolitis.
In addition, the present study found that MP-associated bronchiolitis was mainly seen in infants from 6 months to 1 year of age, with a detection rate of 48.1% in that age group. This result is obviously different from that in previous reports of MP pneumonia, in which MP infections occurred mainly in patients between 5 and 14 years of age [26]. MP infection in infants was reported to be a relatively rare occurrence [10]. However, MP infection can occur at any age. Defilippi et al. [22] revealed that MP infection can occur in young children. This study revealed that in 102 MP-positive children aged 1 month to 13.5 years, 28.38% were < 3 years old, confirming the finding of younger age of MP infection. The possible causes of MP infection are as follows: the Foshan region in China has a subtropical climate with higher temperature and humidity, so MP activity is enhanced and the climate is beneficial to MP transmission [20,21]; infants were more prone to respiratory virus infection, and injury of respiratory mucosa is conducive to MP adhesion [27]; and with increased alertness to MP-infected infants, the chances of detection of MP have increased in infants.
The present study revealed that the white blood cell count can show a nonspecific variation in patients with bronchiolitis associated with MP. Glader et al. [28] reported that the mean white blood cell counts in patients with bronchiolitis associated with MP were similar to those of children of all ages. In the present study, in patients with MP-associated bronchiolitis, the C-reactive protein level was significantly elevated and the procalcitonin level was slightly elevated. These features resemble those of a bacterial infection and were obviously different from those of RSV-associated bronchiolitis. However, the findings of RSV-associated bronchiolitis were the opposite; CT examination of the chest revealed pulmonary interstitial lesions in both lungs in the majority of patients with bronchiolitis associated with MP. Chest CT showed a general increase in the brightness of both lungs in RSV-associated patients with bronchiolitis. This clinical characteristic helps to distinguish between the 2 types of bronchiolitis. Myocardial injury was the most prominent extrapulmonary complication, which was more common in MP-associated bronchiolitis than in RSV-associated bronchiolitis, and emergent MP-associated bronchiolitis can cause more harm. Several studies revealed that myocardial damage was related to changes in immune function caused by inflammation [29–31], and this is supported by the present study, which found C-reactive protein and procalcitonin levels were elevated in patients with MP-associated bronchiolitis.
A report showed that thrombocytosis is very common (33%) in children with MP infection and may be related to inflammation, and no sex differences were found [32]. In the present study, 39.2% of children with MP infection had thrombocytosis with increased CRP and procalcitonin levels, and no sex differences were detected.
A meta-analysis confirmed prematurity and low birth weight were the important risk factors by estimating odds ratios with 95% confidence intervals [33]. Mansbach et al. [34] reported that younger age was the main risk factor of severe RSV-associated bronchiolitis. The findings of our study are consistent with the results in the above-mentioned research. Our study also showed that prematurity with low birth weight and/or young age were primary risky factors of severe RSV-associated bronchiolitis.
The main clinical manifestations of MP-induced respiratory infections in children are cough and fever [35,36]. The present research showed that cough and fever due to MP-associated bronchiolitis were more severe than that due to RSV-associated bronchiolitis, and azithromycin treatment can shorten the course of MP-associated bronchiolitis. However, treatment of RSV-associated bronchiolitis lacks objective antiviral drugs; therefore, the course is longer than that of MP-associated bronchiolitis.
The major limitation of this study was absence of detection of sputum MP-DNA and absence of asymptomatic control patients. We will perform a more extensive study in the future to address these issues.
Conclusions
Our study indicated that MP was the second most common pathogen (after RSV) causing bronchiolitis. Pulmonary interstitial infiltration was a characteristic of this infection. Azithromycin treatment can shorten the course of MP-associated bronchiolitis. Investigation of the epidemiological characteristics of pediatric MP-associated bronchiolitis can help diagnose and treat the disease correctly.
Figures
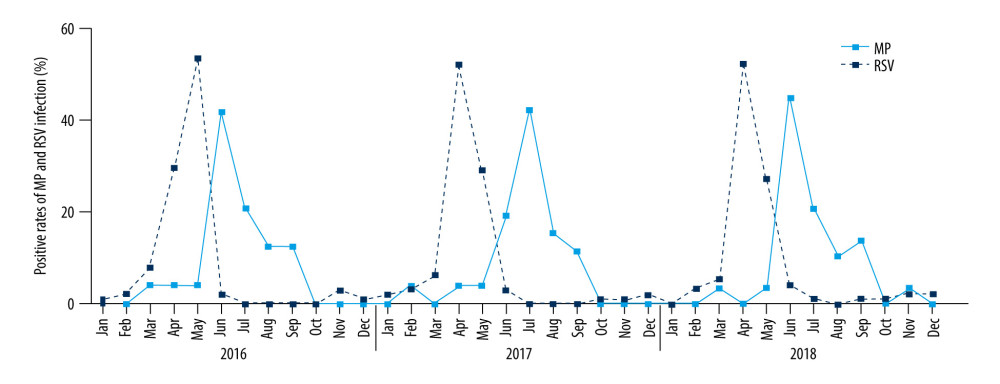 Figure 1. The prevalence distribution of MP-associated bronchiolitis in children between January 2016 and December 2018. The peaks of MP infection occurred between June and July of any particular year, and they were the lowest during December to February. The peaks of RSV infection occurred during April and May of each year, and they were lowest from July to October.
Figure 1. The prevalence distribution of MP-associated bronchiolitis in children between January 2016 and December 2018. The peaks of MP infection occurred between June and July of any particular year, and they were the lowest during December to February. The peaks of RSV infection occurred during April and May of each year, and they were lowest from July to October. 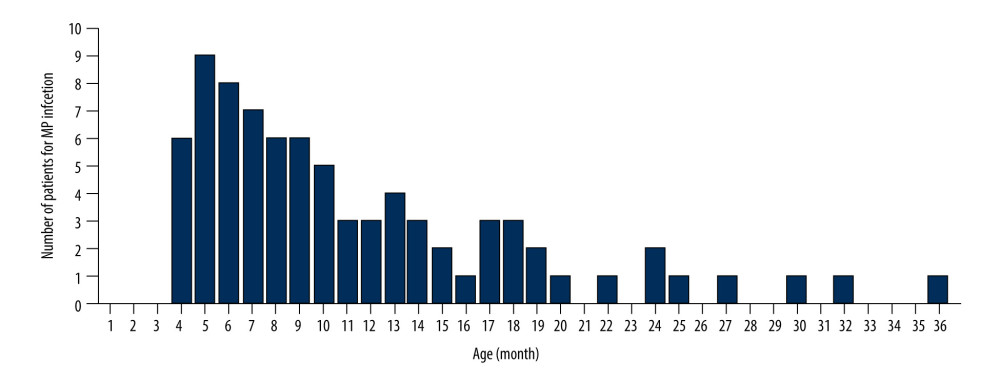 Figure 2. The prevalence and age distribution of MP-associated bronchiolitis in children between January 2016 and December 2018. The number of patients with MP infection in the age groups 4–5 months and 6–12 months was significantly higher than that of the other age groups.
Figure 2. The prevalence and age distribution of MP-associated bronchiolitis in children between January 2016 and December 2018. The number of patients with MP infection in the age groups 4–5 months and 6–12 months was significantly higher than that of the other age groups. 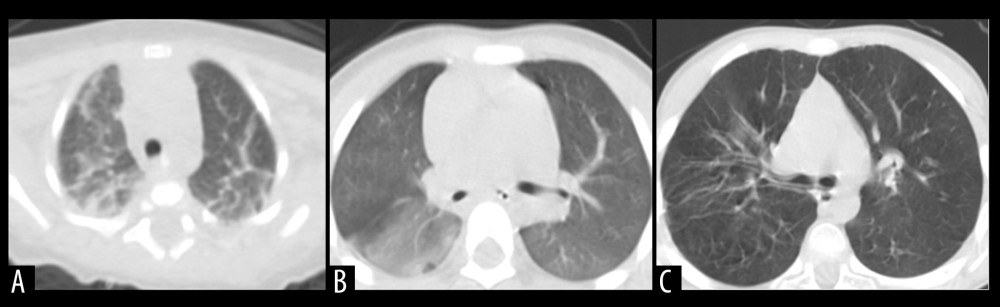 Figure 3. Radiographic characteristics of representative patients. (A) A patient with MP-associated bronchiolitis. Messy, reticular, high-density shadows, with lamellar shadows were found on chest CT. (B) A patient with MP-associated bronchiolitis. Markings accompanied by a misty fuzziness on chest CT. (C) A patient with RSV-associated bronchiolitis. Chest CT shows increased brightness in the bilateral lungs.
Figure 3. Radiographic characteristics of representative patients. (A) A patient with MP-associated bronchiolitis. Messy, reticular, high-density shadows, with lamellar shadows were found on chest CT. (B) A patient with MP-associated bronchiolitis. Markings accompanied by a misty fuzziness on chest CT. (C) A patient with RSV-associated bronchiolitis. Chest CT shows increased brightness in the bilateral lungs. References
1. O’Brien S, Borland ML, Cotterell E, Australasian bronchiolitis guideline: J Paediatr Child Health, 2019; 55; 42-53
2. Ozkaya-Parlakay A, Gulhan B, Bedir-Demirdag T, Viral etiology of bronchiolitis among pediatric patients: Pediatr Infect Dis J, 2019; 38; e233
3. Waites KB, Xiao L, Liu Y: Clin Microbiol Rev, 2017; 30; 747-809
4. Li CM, Gu L, Yin SJ: J Int Med Res, 2013; 41; 1716-23
5. Søndergaard MJ, Friis MB, Hansen DS: PLoS One, 2018; 13; e0195288
6. Yamazaki T, Kenri T: Front Microbiol, 2016; 7; 693
7. Yan C, Sun H, Zhao H: J Clin Microbiol, 2016; 54; 1400-1
8. Jacobs E, Ehrhardt I, Dumke R: Int J Med Microbiol, 2015; 305; 705-8
9. Wang X, Zhong LJ, Chen ZM: World J Pediatr, 2018; 14; 344-49
10. Kutty PK, Jain S, Taylor TH: Clin Infect Dis, 2019; 68; 5-12
11. Watanabe H, Uruma T, Nakamura H: Allergy Asthma Proc, 2014; 35; 204-10
12. Hu YM, Jiang ZF, Bronchiolitis: Zhu Futang Practical Pediatrics, 2003; 1199-206, Beijing, Peoples Health Publishing House
13. Shin EJ, Kim Y, Jeong JY, The changes of prevalence and etiology of pediatric pneumonia from National Emergency Department Information System in Korea, between 2007 and 2014: Korean J Pediatr, 2018; 61; 291-300
14. Liu WK, Liu Q, Chen DH, Epidemiology of acute respiratory infections in children in Guangzhou: A three-year study: PLoS One, 2014; 9; e96674
15. Jain S, Williams DJ, Arnold SR, Community-acquired pneumonia requiring hospitalization among U.S. children: N Engl J Med, 2015; 372; 835-45
16. Xue G, Li M, Wang N: PLoS One, 2018; 13; e0198557
17. Ranjbar R, Halaji M: J Med Microbiol, 2019; 68; 1614-21
18. Eun BW, Kim NH, Choi EH: J Infect, 2008; 56; 326-31
19. Ji W, Chen ZR, Zhou WFEtiology of acute respiratory tract infection in hospitalized children in Suzhou from 2005 to 2011: Zhonghua Yu Fang Yi Xue Za Zhi, 2013; 47; 497-503 [in Chinese]
20. Chen Z, Ji W, Wang Y: Ital J Pediatr, 2013; 39; 34
21. Tian DD, Jiang R, Chen XJ, Meteorological factors on the incidence of MP and RSV pneumonia in children: PLoS One, 2017; 12; e0173409
22. Defilippi A, Silvestri M, Tacchella A: Respir Med, 2008; 102; 1762-68
23. Hadi N, Kashef S, Moazzen M: Braz J Infect Dis, 2011; 15; 97-101
24. Sidal M, Kilic A, Unuvar E: J Trop Pediatr, 2007; 53; 225-31
25. Foy HM, Kenny GE, Cooney MK: J Infect Dis, 1979; 139; 681-87
26. Nolevaux G, Bessaci-Kabouya K, Villenet NEpidemiological and clinical study of respiratory infections in children hospitalized in a pediatric ward between 1999 and 2005 at the Reims University Hospital]: Arch Pediatr, 2008; 15; 1630-36 [in French]
27. Atkinson TP, Balish MF, Waites KB: FEMS Microbiol Rev, 2008; 32; 956-73
28. Glader B, Kliegman RM, Jenson HB: The anemias Nelson textbook of pediatrics, 2007; 2003-18, Philadelphia, WB Saunders Co
29. Liu X, Wu Y, Zhu J, Totally thoracoscopic repair of atrial septal defect reduces systemic inflammatory reaction and myocardial damage in initial patients: Eur J Med Res, 2014; 19; 13
30. Carrabba N, Valenti R, Migliorini A, Prognostic value of myocardial injury following transcatheter aortic valve implantation: Am J Cardiol, 2013; 111; 1475-81
31. Deng MH, Lin CW, Sun YN: Ann Clin Biochem, 2017; 54; 49-54
32. Youn YS, Lee KY, Hwang JY: BMC Pediatr, 2010; 10; 48
33. Shi T, Balsells E, Wastnedge E, Risk factors for respiratory syncytial virus associated with acute lower respiratory infection in children under five years: Systematic review and meta-analysis: J Glob Health, 2015; 5; 020416
34. Mansbach JM, Piedra PA, Teach SJ, Prospective multicenter study of viral etiology and hospital length of stay in children with severe bronchiolitis: Arch Pediatr Adolesc Med, 2012; 166; 700-6
35. Meyer Sauteur PM, Theiler M, Buettcher M: JAMA Dermatol, 2019; 156; 144-50
36. Xia Y, Wu CK, Tang YYDifferences in the clinical features of pneumonia among children of different ages: Zhongguo Dang Dai Er Ke Za Zhi, 2013; 15; 179-82 [in Chinese]
Figures
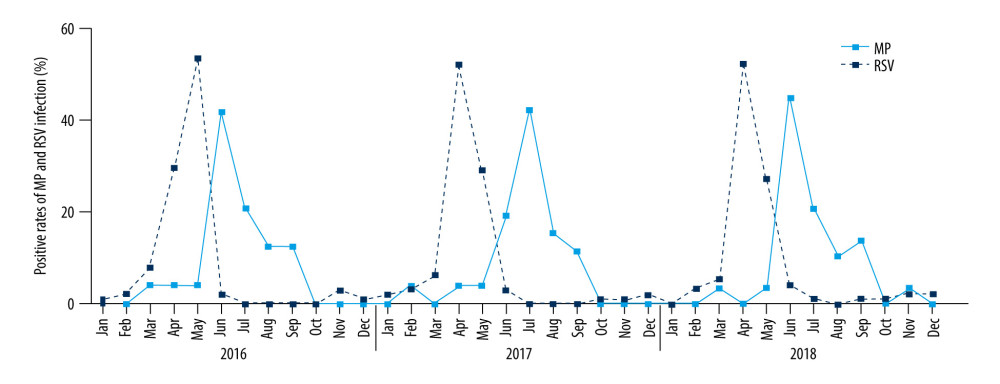 Figure 1. The prevalence distribution of MP-associated bronchiolitis in children between January 2016 and December 2018. The peaks of MP infection occurred between June and July of any particular year, and they were the lowest during December to February. The peaks of RSV infection occurred during April and May of each year, and they were lowest from July to October.
Figure 1. The prevalence distribution of MP-associated bronchiolitis in children between January 2016 and December 2018. The peaks of MP infection occurred between June and July of any particular year, and they were the lowest during December to February. The peaks of RSV infection occurred during April and May of each year, and they were lowest from July to October.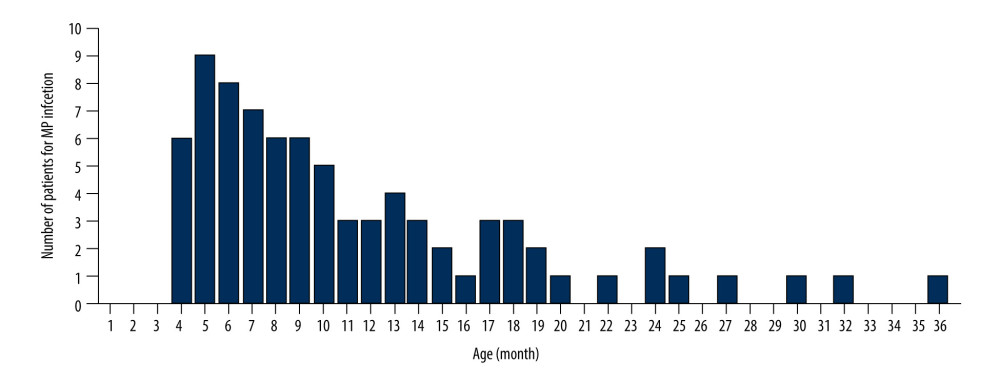 Figure 2. The prevalence and age distribution of MP-associated bronchiolitis in children between January 2016 and December 2018. The number of patients with MP infection in the age groups 4–5 months and 6–12 months was significantly higher than that of the other age groups.
Figure 2. The prevalence and age distribution of MP-associated bronchiolitis in children between January 2016 and December 2018. The number of patients with MP infection in the age groups 4–5 months and 6–12 months was significantly higher than that of the other age groups.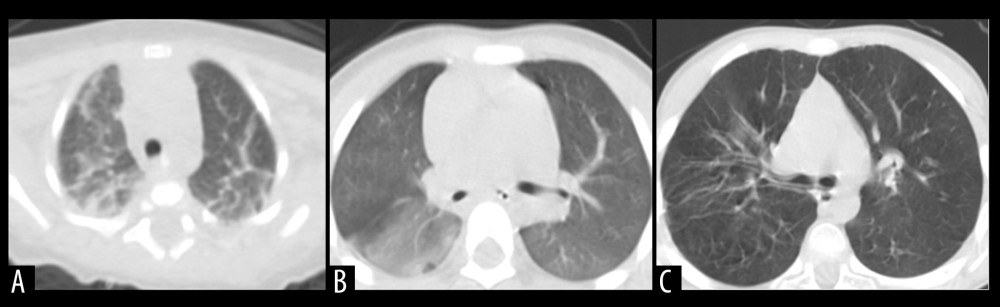 Figure 3. Radiographic characteristics of representative patients. (A) A patient with MP-associated bronchiolitis. Messy, reticular, high-density shadows, with lamellar shadows were found on chest CT. (B) A patient with MP-associated bronchiolitis. Markings accompanied by a misty fuzziness on chest CT. (C) A patient with RSV-associated bronchiolitis. Chest CT shows increased brightness in the bilateral lungs.
Figure 3. Radiographic characteristics of representative patients. (A) A patient with MP-associated bronchiolitis. Messy, reticular, high-density shadows, with lamellar shadows were found on chest CT. (B) A patient with MP-associated bronchiolitis. Markings accompanied by a misty fuzziness on chest CT. (C) A patient with RSV-associated bronchiolitis. Chest CT shows increased brightness in the bilateral lungs. Tables
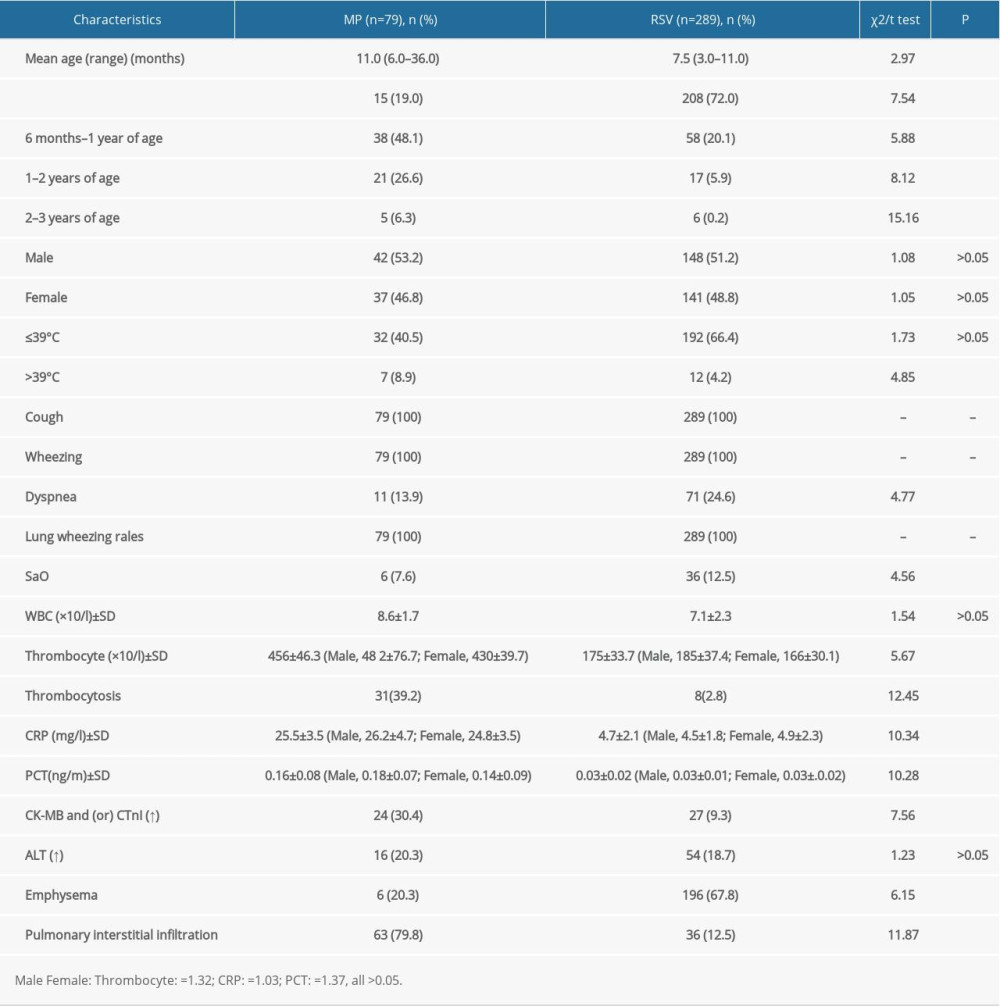 Table 1. Clinical characteristics of patients with bronchiolitis associated with MP or RSV.
Table 1. Clinical characteristics of patients with bronchiolitis associated with MP or RSV.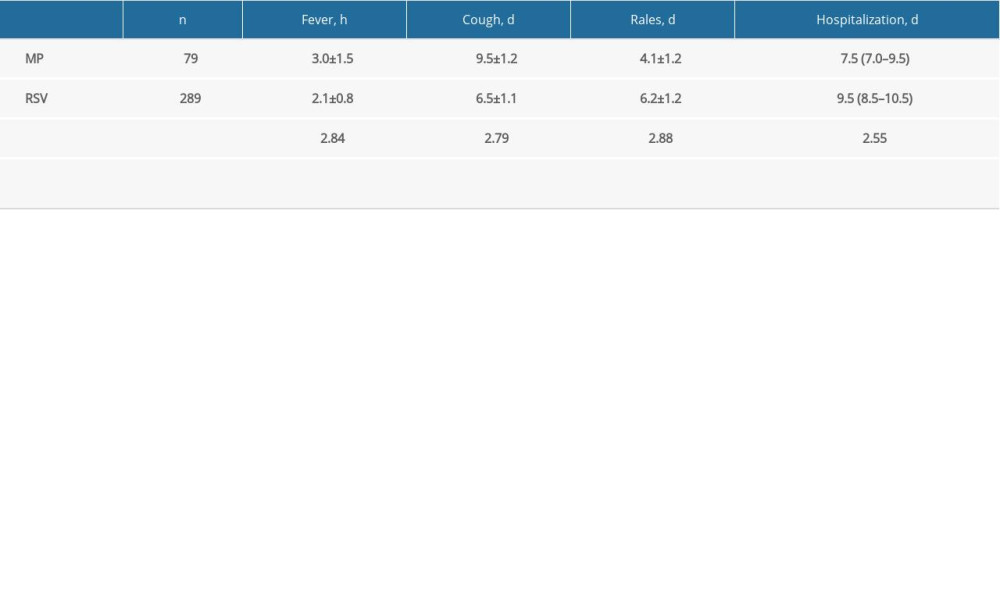 Table 2. Comparison of clinical outcomes of MP- and RSV-associated patients with bronchiolitis.
Table 2. Comparison of clinical outcomes of MP- and RSV-associated patients with bronchiolitis.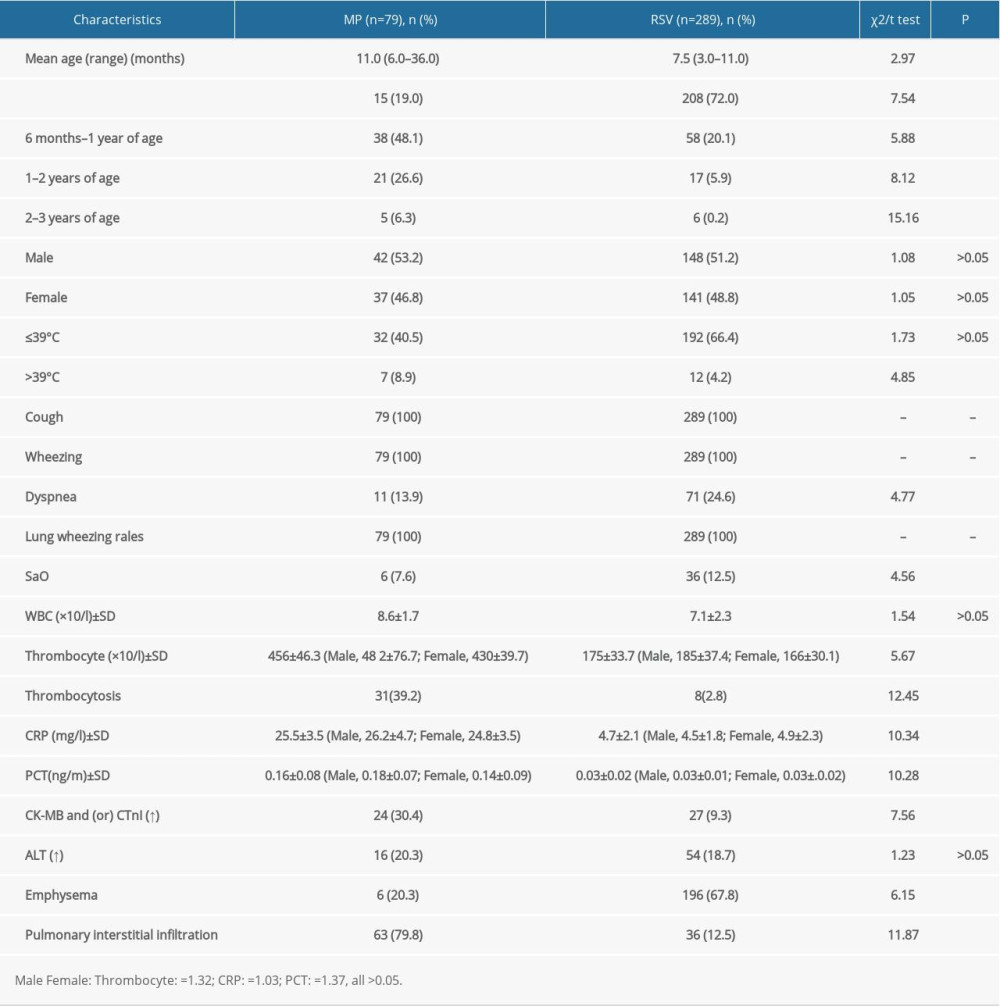 Table 1. Clinical characteristics of patients with bronchiolitis associated with MP or RSV.
Table 1. Clinical characteristics of patients with bronchiolitis associated with MP or RSV.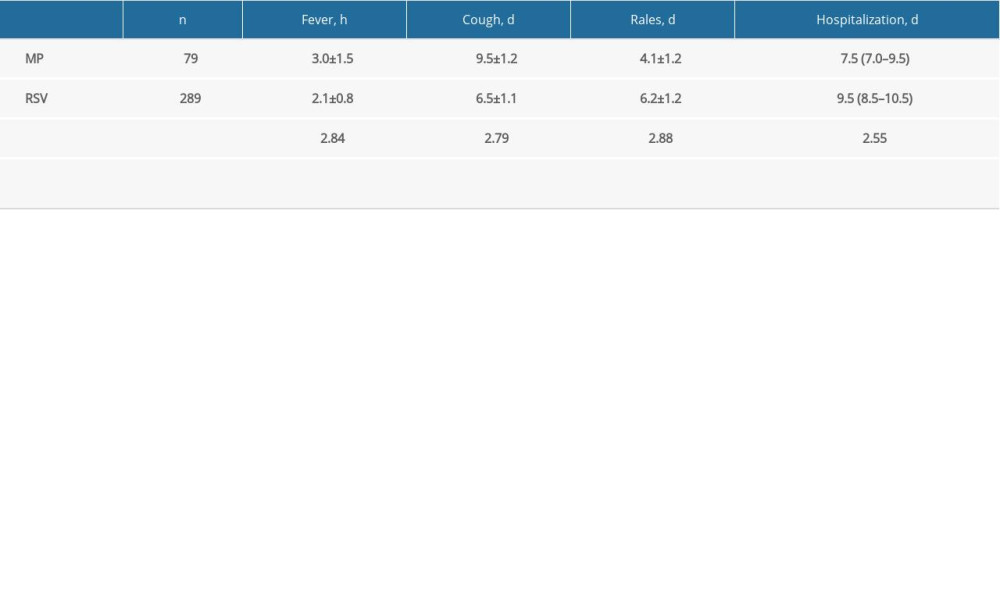 Table 2. Comparison of clinical outcomes of MP- and RSV-associated patients with bronchiolitis.
Table 2. Comparison of clinical outcomes of MP- and RSV-associated patients with bronchiolitis. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








