10 January 2023: Human Study
Prevalence and Associated Factors of Depression Among Frontline Nurses in Wuhan 6 Months After the Outbreak of COVID-19: A Cross-Sectional Study
Huan LiuDOI: 10.12659/MSMBR.938633
Med Sci Monit Basic Res 2023; 29:e938633
Abstract
BACKGROUND: Due to the COVID-19 pandemic, frontline nurses have experienced psychological problems. However, the depression of frontline nurses in Wuhan 6 months after the outbreak of COVID-19 has not been studied adequately. The purpose of this study was to investigate the depression of frontline nurses in Wuhan 6 months after the COVID-19 outbreak and to analyze possible risk and protective factors.
MATERIAL AND METHODS: Data were collected through Wenjuanxing from 612 frontline nurses in Wuhan national COVID-19-designated hospitals between July 27, 2020, and August 12, 2020. The levels of depression, family functioning, and psychological resilience were assessed among frontline nurses in Wuhan with a depression scale, family function scale, and 10-item psychological resilience scale, respectively. The factors associated with depressive symptoms were identified using the chi-square test and binary logistic regression analysis.
RESULTS: A total of 126 respondents were included in the study. The overall prevalence of depression was 25.2%. The need for mental health services was a potential risk factor for depressive symptoms, while family functioning and psychological resilience were potential protective factors. The COVID-19 pandemic poses a major challenge to the depressive symptoms of frontline nursing in Wuhan, highlighting the need for all frontline nurses in Wuhan to be screened for depression regularly for timely intervention.
CONCLUSIONS: To mitigate the impact of the pandemic on depression, psychological interventions for frontline nurses need to be implemented to preserve their mental health.
Keywords: COVID-19, Depression, Disease Outbreaks, Risk Factors, Humans, Cross-Sectional Studies, Pandemics, Prevalence
Background
The global COVID-19 pandemic has caused great suffering and challenges around the world. The WHO declared the virus a public health emergency of international concern on January 30, 2020, and a worldwide pandemic on March 11, 2020 [1]. Wuhan was the first city in China to report cases of COVID-19 and to be severely affected by the COVID-19 outbreak. The Chinese government adopted emergency management steps to prevent the spread of COVID-19. On January 22, 2020, Wuhan city was locked down. As of March 27, 2020, about 60.8% of COVID-19 confirmed cases were located in Wuhan [2]. During the epidemic period, the frontline nurses undertook high-intensity work, not only performing therapeutic work for patients, but also undertaking patients’ psychosocial care [3]. The nursing staff in Wuhan have close contact with a large number of COVID-19 patients, undertake an enormous amount of nursing work, and experience isolation and discrimination, with frontline nurses in Wuhan more likely to suffer from depression during the COVID-19 pandemic [4]. A study found that frontline anti-epidemic medical staff have high symptoms of anxiety and depression [5]. Therefore, we can infer that frontline medical staff members in Wuhan were more vulnerable to depression after the COVID-19 pandemic.
It is well established that the outbreak of emerging infectious disease has a negative psychological impact on frontline medical staff, which has become a very prominent public health problem. Previous studies have shown that during the COVID-19 pandemic, many medical staff, especially frontline medical staff, had severe depression, which seriously threatened the health of medical staff and led to decreased work efficiency [6]. Previous studies confirmed that medical staff experienced higher levels of depressive symptoms 1 year after the SARS-CoV-2 outbreak, indicating that the impacts on mental health were prolonged [7]. After the pandemic, the frontline nurses who dealt with COVID-19 had a psychological burden, further increasing psychological problems, such as depression [8]. Therefore, there is a need for more studies on the depression of frontline nurses after the COVID-19 outbreak.
Psychological resilience refers to a person’s ability to cope with stress; it can prevent the mental health symptoms after exposure to stressors [9]. Previous studies have shown that family support may be the most important source of social support in China, and good family functioning helps reduce depression symptoms during the COVID-19 epidemic [10]. After the COVID-19 pandemic, it is particularly important to assess the association between resilience, family functioning, and depression, because it can provide a reference for frontline nurses to develop depression prevention and intervention strategies.
Taken together, the psychological impact of the COVID-19 pandemic might have long-term adverse effects [11]. Depression problems of frontline nurses continue to pose a challenge and have aroused widespread concern among government officials and hospital administrators. However, to date, few studies have investigated the depression of nurses 6 months after the COVID-19 outbreak. Owing to the lack of existing research, this study aimed to evaluate the current status of depression of Chinese frontline nurses treating patients with COVID-19 and its correlation with family functioning and psychological resilience. We hope that the results of this survey provide support for the more targeted intervention strategies of Wuhan frontline nurses’ depression after the COVID-19 pandemic.
Material and Methods
DESIGN AND PARTICIPANTS:
A web-based cross-sectional study was conducted from July 27, 2020, to August 12, 2020, approximately 6 months after the Chinese government officially announced the COVID-19 outbreak (January 20, 2020). All frontline nurses in Wuhan using WeChat or other social software could participate in this survey and fill in the questionnaire by scanning the QR code of the electronic questionnaire or clicking the electronic link. The participants’ IP addresses were real and valid in Wuhan, and ensured that each IP address could fill out the questionnaire only once.
MEASUREMENTS:
Sociodemographic information mainly included the basic information of the participants, such as sex, age, technical title, need for psychological services or not, fear of COVID-19 or not, psychological resilience, and family functioning.
Depression was measured using the patient health questionnaire (PHQ-2), a self-reported instrument to assess the depression symptoms of respondents. Items were rated on a 4-point Likert scale (0=not at all to 3=nearly every day), higher scores indicated more severe depression. The total score of the PHQ-2 ranged from 0 to 6. In our study, PHQ-2 scores ≥3 points indicated depressive symptoms [12].
The 10-item Connor-Davidson Resilience Scale (CD-RISC-10) is a psychological scale used to assess one’s ability to cope with bad experiences [9]. Each item was divided into a 5-point degree of the scale (0=not true at all to 4=true nearly all the time) in relation to the past month. Scores for the 10 items were summed to obtain a CD-RISC-10 total score, ranging from 0 to 40. Higher scores indicated higher resilience. The CD-RISC-10 sum scores were divided into “high resilience” and “low resilience” groups, with a cut-off score of 30 or higher.
Family functioning was assessed using the Family APGAR index [13], which includes 5 items, dealing with degree of adaptation, partnership, growth, affection, and resolve, and each item has a score of 0 to 2. The total score ranges from 0 to 10, with higher scores indicating better family functioning. A score of 0 and ≤3 is classified as severe family dysfunction, ≥4 and ≤6 as moderate family dysfunction, and ≥7 as good family functioning. In this research, Cronbach’s α of the scale was 0.834.
STATISTICAL ANALYSIS:
Excel data were derived from the website of the “Questionnaire Star”, and data analysis was performed using SPSS version 17.0 (IBM Corp, Armonk, NY, USA). Chi-square tests were used to compare the difference between the depressed group and the non-depressed group. A binary logistic regression analysis was used to determine the associated factors of depression. Variables with
Results
DEPRESSION STATUS AND SOCIODEMOGRAPHIC PROFILE OF FRONTLINE NURSES:
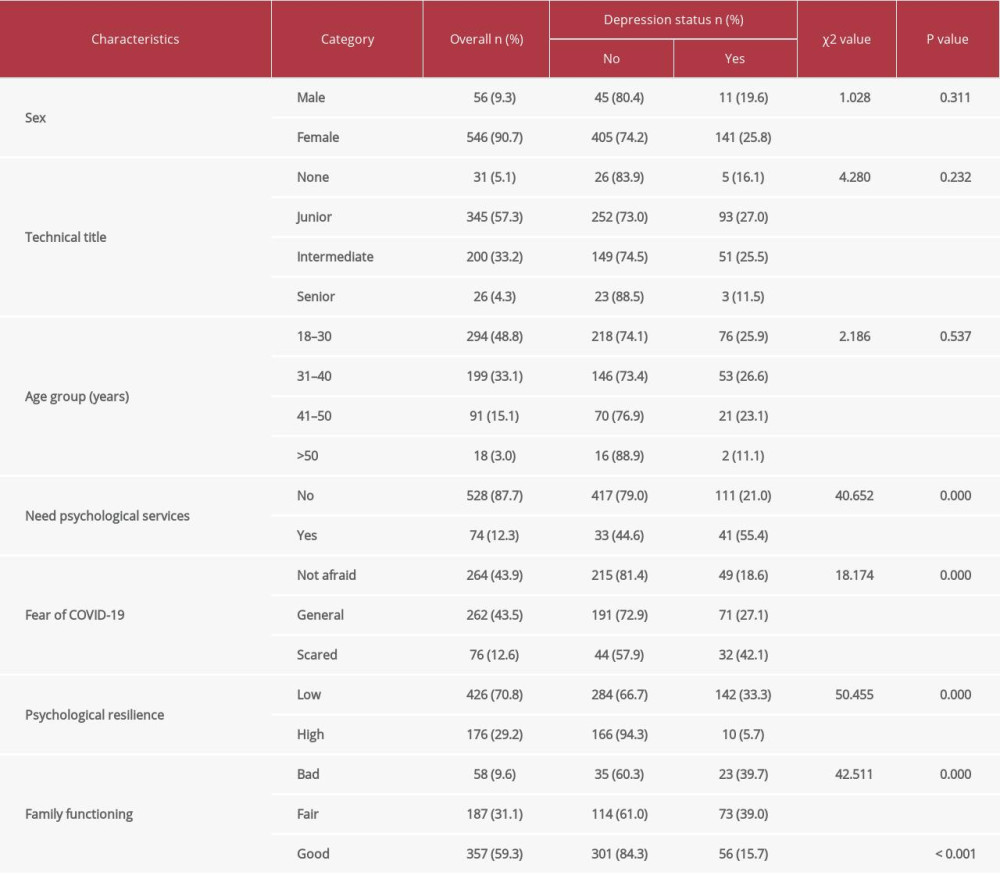
The demographic details of the participants are represented in Table 1. A total of 612 frontline nurses participated in the study, among which 56 (9.3%) were men and 546 (90.7%) were women. Depression was identified in 152 of the 612 frontline nurses, with a prevalence rate of 25.2%. The prevalence of depression was significantly different among the frontline nurses with different levels of fear of COVID-19, psychological resilience, and family functioning (all P<0.0001). Need for psychological services was associated with increased prevalence of depression (P<0.05), whereas sex, technical title, and age group had no significant effect on depression (P>0.05; Table 1).
RISK FACTORS ASSOCIATED WITH DEPRESSIVE SYMPTOMS:
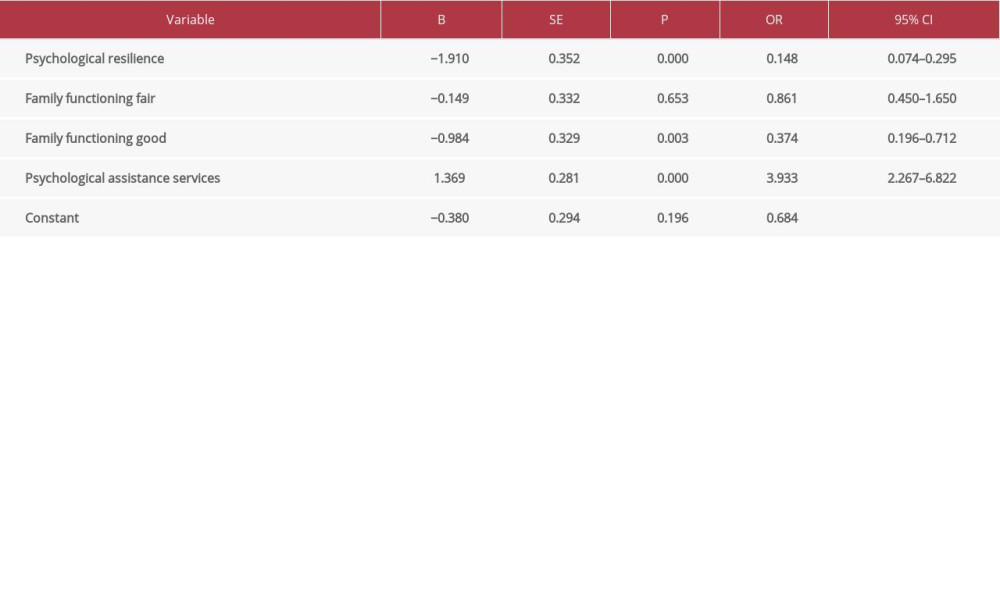
In the binary logistic regression analysis (Table 2), those who reported higher psychological resilience, compared with those with lower psychological resilience, showed a decreased risk of depression symptoms (OR=0.148, 95% CI: 0.074–0.295). Fair (OR=0.861, 95% CI: 0.450–1.650) and moderate (OR =0.374, 95% CI: 0.196–0.712) levels of family functioning were associated with a lower risk of depression than a bad level of family functioning. Compared with nurses who did not need psychological services, nurses who needed psychological services had a higher risk of depressive symptoms (OR=3.933, 95% CI: 2.267–6.822).
Discussion
To the best of our knowledge, this is the first study to report the prevalence of depression among frontline nurses in Wuhan 6 months after the start of the COVID-19 pandemic. Our results revealed that the overall prevalence of depression among nurses was 25.2% 6 months after the COVID-19 outbreak, which suggests that more than a quarter of the nurses had depression. The depression prevalence is slightly lower than the sample of 994 medical and nursing staff working in Wuhan (36.9%) during the COVID-19 outbreak [14], but the present study also shows that the impact of the COVID-19 pandemic on depression has persisted. Therefore, frontline nurses in Wuhan were under huge mental distress, and it is necessary to provide mental health support for them [15]. A study showed that the cCBT program developed by Zhifen Liu was an effective nonpharmacological treatment for depressive symptoms of COVID-19 patients [16].
Our results showed high depressive symptoms among frontline nurses in Wuhan with low resilience and lower depressive symptoms among those with high resilience scores. Similar to previous studies, there was a negative correlation between depressive symptoms and psychological resilience [17]. The possible explanation is that frontline nurses with higher resilience levels would be better able to deal psychologically with the pressure brought by COVID-19, as psychological resilience may buffer the adverse effects of demographic characteristics and work factors on their depression after the COVID-19 pandemic [18]. To enhance psychological resilience, the Chinese healthcare providers can intervene with treatment for frontline nurses. Thus, psychological resilience is still a major goal for psychological intervention for frontline nurses in Wuhan after the COVID-19 pandemic.
The results of this study indicated that nursing staff with poor family functioning tended to develop depression symptoms, which is consistent with previous research [10]. According to the isolation policy, nurses who had contact with COVID-19 patients needed to be quarantined for 2 weeks. This policy may have affected the frontline nurses’ relationships with partners, children, and other family members. Frontline nurses with family dysfunction cannot effectively communicate emotions and thoughts with other family members, thus leading to depression [19]. Good family functioning can help individuals obtain external support in adversity and help them build confidence [20]. Therefore, good family functioning can alleviate the various pressures caused by the COVID-19 pandemic. It is necessary for families to provide more support to reduce the impact of frontline work on nurses’ depression during the COVID-19 pandemic.
Our results indicated that the risk of depression in frontline nurses who needed psychological counseling services was higher, which may be related to the continuous suffering from greater psychological pressure of the frontline nurses who need psychological counseling services. Therefore, after the COVID-19 pandemic, frontline nurses should be vigorously encouraged to conduct psychological screening and psychological counseling activities and to relieve psychological problems; online psychological assessment, mental health education, and psychological crisis intervention were fully implemented for frontline nurses to provide ideas for reducing depression [14].
This study has several limitations that must be considered. First, this research was a cross-sectional study; therefore, we were unable to assess the relationship between cause and effect. Second, we used a web-based survey with a convenience sample, and therefore selection bias may be inevitable, affecting the accuracy of the research results. Third, a nationwide multicenter cross-sectional study is needed to verify the research results.
Conclusions
In conclusion, the results of the present study indicate that frontline nurses in Wuhan had high rates of depressive symptoms 6 months after the outbreak of COVID-19. Mental health services, family functioning, and psychological resilience are the most important factors affecting depression. The pandemic’s effects on mental wellbeing were serious and will continue; therefore, government officials and hospital administrators should provide adequate support to frontline nurses and reassure them after the COVID-19 pandemic, which could do much to ameliorate depressive symptoms.
References
1. World Health Organization: Coronavirus Disease (COVID-2019) Situation Reports, 2020, World Health Organization Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/
2. Dong H, Hu R, Lu C, Investigation on the mental health status of pregnant women in China during the pandemic of COVID-19: Arch Gynecol Obstet, 2021; 303(2); 463-69
3. Jiang L, Broome ME, Ning C, The performance and professionalism of nurses in the fight against the new outbreak of COVID-19 epidemic is laudable: Int J Nurs Stud, 2020; 107; 103578
4. Kang L, Li Y, Hu S, The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus: Lancet Psychiatry, 2020; 7(3); e14
5. Zhu J, Sun L, Zhang L, Prevalence and influencing factors of anxiety and depression symptoms in the first-line medical staff fighting against COVID-19 in Gansu: Front Psychiatry, 2020; 11; 386
6. Xiang YT, Yang Y, Li W, Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed: Lancet Psychiatry, 2020; 7(3); 228-29
7. Lee AM, Wong JG, McAlonan GM, Stress and psychological distress among SARS survivors 1 year after outbreak: Can J Psychiatry, 2007; 52(4); 233-40
8. Barello S, Palamenghi L, Graffigna G, Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic: Psychiatry Res, 2020; 290; 113129
9. Connor KM, Davidson JRT, Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC): Depress Anxiety, 2003; 18; 76-82
10. Jiang W, Liu X, Zhang J, Mental health status of Chinese residents during the COVID-19 epidemic: BMC Psychiatry, 2020; 20(1); 580
11. Kapetanos K, Mazeri S, Constantinou D, Exploring the factors associated with the mental health of frontline healthcare workers during the COVID-19 pandemic in Cyprus: PLoS One, 2021; 16(10); e0258475
12. Zhang WR, Wang K, Yin L, Mental Health and psychosocial problems of medical health workers during the COVID-19 epidemic in China: Psychother Psychosom, 2020; 89(4); 242-50
13. Smilkstein G, The family APGAR: A proposal for a family function test and its use by physicians: J Fam Pract, 1978; 6(6); 1231-39
14. Kang L, Ma S, Chen M, Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study: Brain Behav Immun, 2020; 87; 11-17
15. Wang P, Shen X, Jiang Y, Psychological and sleep disturbances among first-line, second-line, and at home medical staff during the COVID-19 pandemic in Shanghai, China: Front Public Health, 2022; 10; 1006610
16. Liu Z, Qiao D, Xu Y, The efficacy of computerized cognitive behavioral therapy for depressive and anxiety symptoms in patients with COVID-19: Randomized controlled trial: J Med Internet Res, 2021; 23(5); e26883
17. Havnen A, Anyan F, Hjemdal O, Resilience moderates negative outcome from stress during the COVID-19 pandemic: A moderated-mediation approach: Int J Environ Res Public Health, 2020; 17(18); 6461
18. Kavi T, Avsec A, Zager Kocjan G, Psychological functioning of Slovene adults during the COVID-19 pandemic: Does resilience matter?: Psychiatr Q, 2020; 92(1); 207-16
19. Hu N, Li Y, He SS, Impact of the family environment on the emotional state of medical staff during the COVID-19 outbreak: The mediating effect of self-efficacy: Front Psychol, 2020; 11; 576515
20. Jiang J, Han P, Huang X, Post-traumatic growth experience of first-line emergency nurses infected with COVID-19 during the epidemic period-A qualitative study in Shanghai, China: Front Public Health, 2022; 10; 1015316
Most Viewed Current Articles
15 Jun 2022 : Clinical Research
Evaluation of Apical Leakage After Root Canal Obturation with Glass Ionomer, Resin, and Zinc Oxide Eugenol ...DOI :10.12659/MSMBR.936675
Med Sci Monit Basic Res 2022; 28:e936675
07 Jul 2022 : Laboratory Research
Cytotoxicity, Apoptosis, Migration Inhibition, and Autophagy-Induced by Crude Ricin from Ricinus communis S...DOI :10.12659/MSMBR.936683
Med Sci Monit Basic Res 2022; 28:e936683
01 Jun 2022 : Laboratory Research
Comparison of Sealing Abilities Among Zinc Oxide Eugenol Root-Canal Filling Cement, Antibacterial Biocerami...DOI :10.12659/MSMBR.936319
Med Sci Monit Basic Res 2022; 28:e936319
08 Dec 2022 : Original article
Use of Estimated Glomerular Filtration Rate and Urine Albumin-to-Creatinine Ratio Based on KDIGO 2012 Guide...DOI :10.12659/MSMBR.938176
Med Sci Monit Basic Res 2022; 28:e938176