07 February 2023: Human Study
A Prospective Study of 73 Patients to Compare Forward Head Angle, Forward Shoulder Angle, Maximal Inspiratory Pressure, and Self-Reported Breathing-Related Symptoms Before and After Open-Heart Surgery
Bussakorn Thanasarn12BCEF, Wittawat Pibul3BEF, Chitima Kulchanarat4BE, Dusarkorn Piathip5BE, Kornanong Yuenyongchaiwat16ACDEFG*DOI: 10.12659/MSMBR.938802
Med Sci Monit Basic Res 2023; 29:e938802
Abstract
BACKGROUND: Patients who undergo open-heart surgery often experience widespread musculoskeletal and pulmonary complications. These can interfere with their functioning, resulting in soft tissue changes, worsening postural changes, and poor respiratory performance. Therefore, the prospective study aimed to compare forward head angle (FHA) and forward shoulder angle (FSA), maximal inspiratory pressure (MIP), and self-reported breathing dysfunction before and after open-heart surgery.
MATERIAL AND METHODS: In a prospective observational study of 106 patients, men and women scheduled for open-heart surgery were enrolled. Prior to surgery and before discharge from the hospital, all patients were required to assess FHA and FSA using 2-dimensional motion analysis software, MIP using a respiratory pressure meter, and breathing dysfunction using the 25-item Self Evaluation of Breathing Questionnaire (SEBQ). Paired t test was used to compare differences between before and after surgery. To evaluate associations, logistic regression analysis was performed.
RESULTS: Of the 106 patients recruited, 73 completed the study. FHA (-Δ6.55±4.77, P<0.001), FSA (-Δ4.82±7.29, P<0.001), and MIP (-Δ14.07±17.02 cmH₂O, P<0.001) values were decreased prior to discharge from the hospital compared with values before surgery. Regression analysis found that decreased MIP after median sternotomy was associated with an increase in FHA and breathing dysfunction in patients after open-heart surgery.
CONCLUSIONS: After open-heart surgery, increased FHA and breathing dysfunction (SEBQ) were associated with reduced MIP, which may be associated with poor respiratory performance after surgery. Therefore, postoperative physiotherapy in this patient group should aim to improve postural changes.
Keywords: Posture, Respiratory Muscles, Thoracic Surgery, Male, Humans, Female, Shoulder, Prospective Studies, self report, Maximal Respiratory Pressures, Cardiac Surgical Procedures
Background
After open-heart surgery, patients with median sternotomy are recommended to restrict upper limb movements that stretch the sternum, including raising their arms above the head, shoulder abduction greater than 90°, or shoulder extension [1]. This restriction of upper body movement is usually instructed for 8 to 12 weeks after surgery to prevent sternal instability [2]. As a result of these limitations and incision wounds, tenderness around the chest wall and pain at the surgical wound have been noted, which might restrict upper body activity. Further, inappropriate posture in patients who have undergone open-heart surgery, such as forward head posture and rounded shoulder, may be caused from the incision wound or muscle imbalance [3,4]. These factors can lead to an inability to perform activities in daily life, cause chronic pain, and adversely affect the respiratory system due to increased muscle tightness.
A previous study found that the neck and thoracic muscles are related to the function of the shoulder and scapula muscles, because they attach to the cervical and thoracic spine [5]. Generally, these muscles work in coordination with each other; poor muscle coordination causes increased musculoskeletal disorders [5]. Additionally, inappropriate posture, such as forward head posture, greatly affects the muscles surrounding the neck and changes in the thoracic vertebrae, which simultaneously results in modification of the ribcage [6]. All of these changes affect the intercostal muscles, including the diaphragm muscle, which is located on the lowest costal bone. Therefore, this might result in both labored and quiet breathing alterations.
Forward head posture causes muscle imbalance and thoracic restriction, which results in a limitation of ribcage expansion [6,7]. Accordingly, lung volume is reduced [6,7]. Han et al reported that people with forward head posture showed a reduction in pulmonary function compared with normal controls [8]. In addition, forward head posture is related to weakness of respiratory muscles in people with neck pain [9]. Therefore, these might be the cause of long-term musculoskeletal and respiratory problems that interfere with the patient’s daily life. Furthermore, several studies have reported changes in patients’ respiratory muscle strength when comparing before and after heart surgery [10,11]. Measuring maximal inspiratory pressure is a simple way of determining inspiratory muscle strength [12,13]. An individual’s ability to generate a tensile force by measuring upper airway pressure (mouth or nose) during a maximal inspiratory effort can be used to evaluate inspiratory muscle strength [12,13].
In addition, open-heart surgery can affect posture and breathing and delay recovery [14]. There are several measurements to assess symptoms of dysfunctional breathing [15]. The 25-item Self Evaluation of Breathing Questionnaire (SEBQ) was developed by Mitchell et al for evaluation of dysfunctional breathing or breathing discomfort [15]. The SEBQ has a high intraclass correlation coefficient and internal consistency (Cronbach’s alpha=0.93) [15].
The Kinovea 2-dimensional (2D) motion analysis software can be used to measure kinematic parameters [16]. The validity and reliability of the Kinovea 2D are acceptable for measuring the distance up to 5 m from the object and at different in angles of 90° to 45° [16]. However, few studies have been conducted to perform clinical or objective assessments for musculoskeletal and respiratory problems in patients who have undergone open-heart surgery. Therefore, this prospective study of 73 patients aimed to compare forward head angle using 2D motion analysis software, maximal inspiratory pressure using a respiratory pressure meter to assess inspiratory muscle strength, and self-reported breathing-related symptoms using the 25-item SEBQ before and after open heart surgery.
Material and Methods
ETHICS STATEMENT:
The study was approved by the Ethics Human Committee of Thammasat University and Rajavithi Hospital. This study was conducted in accordance with the principles of the Declaration of Helsinki, the Belmont Report, Council for International Organizations of Medical Sciences guidelines, and International Conference on Harmonization-Good Clinical Practice (ICH-GCP). The clinical trial registration no. is TCTR20210701007.
PATIENT SELECTION:
Based upon data from the heart operation unit in 2020, a total number of 155 patients underwent open-heart surgery and 112 patients were recruited. However, to account for any dropouts, 123 patients were enrolled. This prospective observational study was designed in 2 hospital centers, Thammasat University Hospital and Rajavithi Hospital.
All individuals who were scheduled to undergo open-heart surgery procedures via median sternotomy and were ≥18 years old were included.
The exclusion criteria were as follows: patients who underwent emergency surgery or had a history of aortic dissection or aneurysm, cervical or thoracic injury, cerebrovascular accident with upper limb dysfunction, psychiatric disorders, previous surgery via median sternotomy, or thoracotomy. Furthermore, patients with exacerbated chronic obstructive pulmonary disease or asthma within 24 to 72 h prior to the test who had a high temperature (>37.5°C), uncontrolled atrial or ventricular arrhythmias, uncontrolled sinus tachycardia (>120 beats/min), resting systolic blood pressure >180 mmHg and/or resting diastolic blood pressure >120 mmHg [17], recent chest pain within 8 h prior to the test, inability to stand alone, or pregnancy were also excluded.
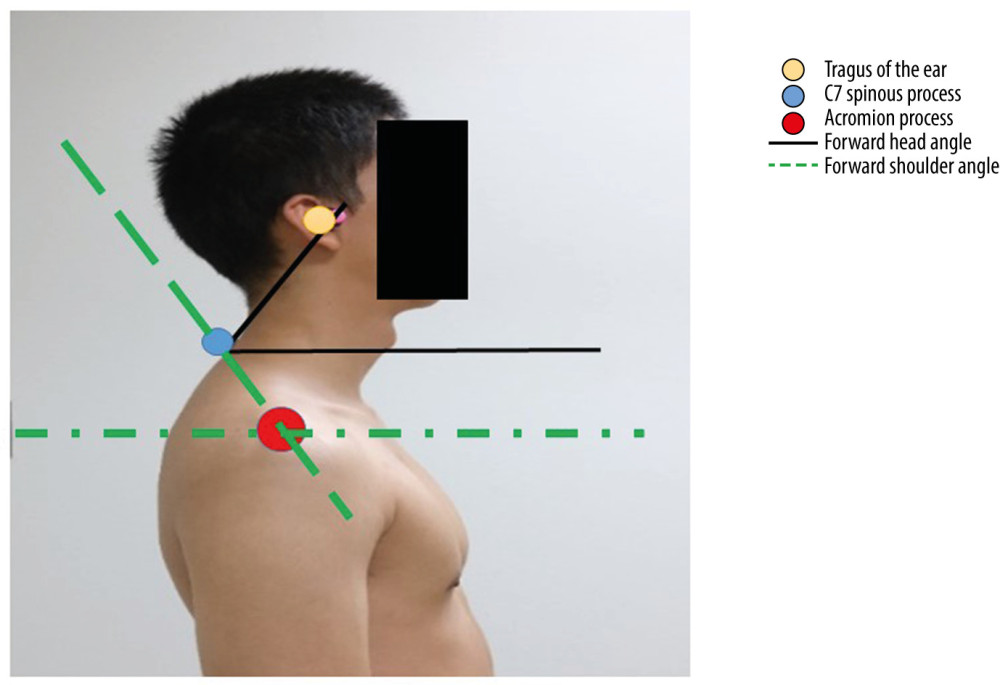
FORWARD HEAD ANGLE AND FORWARD SHOULDER ANGLE USING 2D MOTION ANALYSIS SOFTWARE:
A 2D motion analysis program, Kinovea, was used to assess the forward head angle and forward shoulder angle. While the patients were standing, a digital camera (X100V; Fujifilm) was placed at a distance of 1.5 m from the patient. The height of the camera was adjusted to the level of each patient’s shoulder [18]. In addition, body markers were placed over each landmark, including the tragus of the ear, spinous process of the C7 vertebra, and acromion process. The plumb line was defined by the true vertical line in the digital images [18].
The photograph was taken at the patient’s dominant side from the lateral view while the patient was in the standing position. Prior to taking a photograph, the patients were requested to move their head and neck for full flexion and extension, and then gradually turn into a natural position. Patients were asked to focus on the target at the level of their eyes. Finally, the forward head angle and forward shoulder angle were calculated using the Kinovea program, version 0.8.15. The intra-rater reliability (ICC) was 0.66 with a standard error of the mean=3.54, and the inter-rater reliability (ICC) was 0.87 with standard error of the mean=1.85. Forward head angle was defined as the angle formed at the intersection of a horizontal line through the C7 spinous process and a line of the C7 spinous process to the tragus of the ear. A cutoff point of <50° was defined as forward head posture [18]. The forward shoulder angle was identified as the angle formed at the intersection of a horizontal line through the acromion process and a line of the acromion process to the C7 spinous process (Figure 1).
MAXIMAL INSPIRATORY PRESSURE USING A RESPIRATORY PRESSURE METER:
The maximal inspiratory pressure was measured using a respiratory pressure meter (MicroRPM; CareFusion, United Kingdom). The participants were required to exhale until they began residual volume and then fully inhale through the mouthpiece [12]. Each inspiratory maximum pressure measurement was held for at least 1.5 s and repeated 3 times. The maximum measured value, with a difference of no more than 20% for each measurement, was recorded [12]. The values were recorded and analyzed.
THE 25-ITEM SEBQ:
The SEBQ is an assessment model developed for the qualitative and quantitative assessment of uncomfortable respiratory sensations and self-perception of breathing [15]. The SEBQ consists of 25 questions, with each having a score of 0 to 4 from 4 answer levels [15]. A score of 0 represents never/not true at all, 1 represents occasionally/a bit true, 2 represents frequently/mostly true, and 3 represents very frequently/very true [15]. The SEBQ was found to have a high level of test-retest reliability [15], with a cut-off point ≥25 defined as dysfunctional breathing [19].
PAIN SCALE:
The numerical rating scale was used to indicate the degree of pain sensation, which consists of integers ranging from 0 to 10, with 0 representing “no pain” and 10 representing “worst imaginable pain”. Patients were asked to select a single number that best represented their pain severity.
Changes in forward head angle, forward shoulder angle, and maximal inspiratory pressure were reassessed within 72 h prior to discharge from the hospital. The numerical rating scale and SEBQ scores were also recorded before discharge.
STATISTICAL ANALYSIS:
Descriptive statistics were used to describe the sample characteristics. Paired
Results
PATIENTS STUDIED:
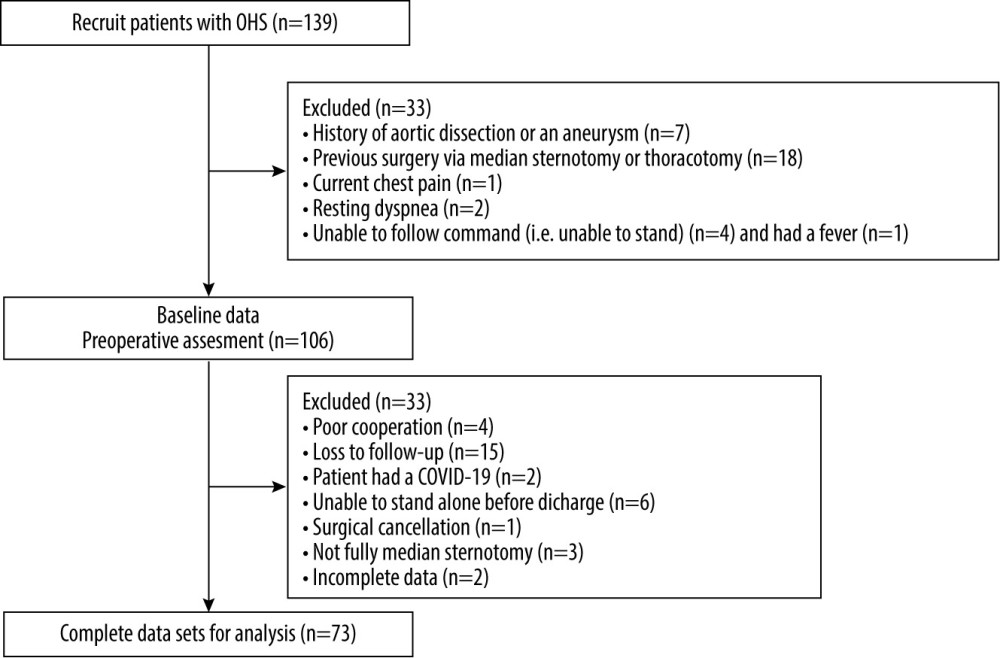
A total of 139 patients were evaluated for eligibility; however, 33 participants were excluded because they failed to meet the inclusion criteria. A total of 106 patients were recruited in the study, and 33 patients were excluded because of COVID-19, inability to stand alone before discharge, cancellation of the operation, or incomplete data (Figure 2).
Details of the clinical and characteristic data of the study population are shown in Table 1. The mean age of patients who had undergone open-heart surgery was 61.29 years, with functional class I–II; the study population included 47 men (64.4%) and 26 women (35.6%), with mean body mass index of 25.21 kg/m2. The mean wound pain score was 3.48±1.83. The average duration of hospitalization was 7.77±3.54 days, with no statistically significant difference between coronary artery disease, valvular heart disease, and combination groups in forward head angle, forward shoulder angle, maximal inspiratory pressure, and SBEQ.
COMPARISON OF FORWARD HEAD ANGLE, FORWARD SHOULDER ANGLE, MAXIMAL INSPIRATORY PRESSURE AND SEBQ BEFORE AND AFTER SURGERY:
A comparison of the forward head angle, forward shoulder angle, maximal inspiratory pressure, and SEBQ before and after surgery is presented in Table 2. The comparison shows that the mean values of the forward head angle, forward shoulder angle, and maximal inspiratory pressure significantly decreased from before and after surgery, but the SEBQ score did not.
ASSOCIATION BETWEEN FORWARD HEAD ANGLE, FORWARD SHOULDER ANGLE, MAXIMAL INSPIRATORY PRESSURE, AND SEBQ:
In addition, a significant positive correlation was found between maximal inspiratory pressure values and forward head angle in patients postoperatively (
Regression analysis showed that postoperative maximal inspiratory pressure values were positively associated with forward head posture and negatively associated with SEBQ in patients after open-heart surgery. Therefore, a reduction in maximal inspiratory pressure in patients after open-heart surgery was predicted by a model that included postoperative forward head posture and SEBQ scores, accounting for 14.5% of the variance (Table 3).
Discussion
In this study, we aimed to examine the changes in forward head posture and rounded shoulder in patients before and after open-heart surgery. We also studied the relationship between respiratory performance and changes in forward head posture and rounded shoulder after open-heart surgery. The study revealed that changes in posture and inspiratory muscle strength were observed after surgery. In addition, a decrease in maximal inspiratory pressure was predicted by postoperative forward head angle and SEBQ.
In this study, the mean values of forward head angle and forward shoulder angle were significantly decreased postoperatively compared with preoperatively. Similarly, a previous study found changes in posture and postural abnormalities in patients who underwent coronary artery bypass graft surgery [20]. Patients with median sternotomy frequently experience thoracic musculoskeletal symptoms that can impede their ability to function [4].
Poor posture, such as a slouched posture, has been reported after cardiac surgery. Furthermore, post-sternotomy pain syndrome, which refers to discomfort after cardiac surgery that persists for at least 2 months [21], later leads to muscle tension. Pain intensity is a factor that might lead to forward head posture and rounded shoulders. In this study, a maximal pain intensity of 3.48±1.83 was observed in the area at median sternotomy before discharge from the hospital after an average of 7 days. Pain at the anterior chest wall might be due to acute postoperative pain caused by tissue damage (eg, the skin, subcutaneous tissue, fascia, bone, and cartilage). In addition to nociceptive stimulation from direct tissue injury, the inflammatory response leads to peripheral and central sensitization in the pain experience, which might lead to pain at median sternotomy [22,23]. However, pain intensity in patients after open-heart surgery gradually decreases from day to day, such as in the early postoperative periods (within the first 24 h) to the removal of drains to getting out of the bed, or from days 1, 3, and 5 postoperatively [24]. Mueller et al reported that maximal pain intensity was higher on postoperative days 1 and 2 and lower on postoperative days 3 and 7 [25]. In addition, 12 weeks after surgery, pain intensity returned to that before the heart surgery [23,26].
Another potential cause of the measured increase in forward head posture and rounded shoulder is kinesiophobia, which is characterized by fears of movement, general activity, and any physical or mental discomfort [27]. Patients who underwent open-heart surgery via median sternotomy had high scores for kinesiophobia (ie, high fear of movement) after surgery [28]. In addition, restriction of upper limb movement might contribute to kinesiophobia after cardiac surgery [28]. As a result, this can cause worsening of posture and lead to soft tissue changes. Thus, the body may compensate by moving the head forward and shifting the center of gravity, resulting in an increased forward head posture [29]. However, kinesiophobia was not recorded in the present study; therefore, future studies are needed for further exploration.
Moreover, posture abnormalities for long periods can be a risk factor for developing upper crossed syndrome and decreased respiratory muscle strength [3,9,30]. After surgery, the antigravity muscles are weakened, which reduces the ability to maintain body posture [3,30]. Therefore, to correct body alignment, patients tend to maintain their posture by moving their heads forward. A decrease in the forward head angle causes an increase in the torque of the cervical extensor muscles, whose strong isometric contraction is necessary to counteract the force of gravity [30]. This can be explained using the cog-wheel model, in which, while the body is in a slumped sitting position, changes in posture and function of the lumbopelvic, thoracic, and head and neck muscles are interrelated [31]. In the slumped sitting position, the posterior tilt of the pelvis is comparable to the counterclockwise rotation of a cog [31]. Consequently, the thoracic spine rotates in a clockwise direction, resulting in increased thoracic kyphosis, therefore affecting the cervical spine to rotate counterclockwise, causing a forward head and neck [31].
Regarding postoperative angle change, the study also discovered a significant reduction in maximal inspiratory pressure in the postoperative period. The decrease in respiratory muscle strength is associated with intraoperative factors (eg, type of surgery, general anesthesia, medication of heart, cardiovascular bypass, and ventilator use) and postoperative pain [11]. Injury of the phrenic nerve, which is the main breathing muscle, can occur during cardiac surgery because of the position of the phrenic nerve running from the neck to the upper thorax through the mediastinum to the parietal pleura and fibrous pericardium [32]. In addition, sternal retraction during median sternotomy can cause costovertebral joint strain after surgery [33]. The costovertebral joint plays an important role in stabilization, load bearing, and protection of the thoracic spine, which is also important for chest wall movement during breathing [34]. Therefore, resection of pericardial tissue and the surgical procedure can result in injury to the phrenic nerve and joint mobility. Furthermore, in patients after coronary artery bypass graft, changes in blood cortisol and C-reactive protein levels were associated with changes in circulatory factors affecting muscle protein synthesis [35]. Hypercortisolemia causes skeletal muscle wasting through a combination of increased protein breakdown and C-reactive protein levels that impair skeletal muscle protein synthesis [35]. This may be a cause of the decreased strength of the respiratory muscles in patients after heart surgery.
Furthermore, the results of this study revealed a significant positive correlation between maximal inspiratory pressure and forward head angle after open-heart surgery. Zafar et al [36] found that head and neck posture changed respiratory function, with decreased diaphragmatic muscle strength. This indicates that head posture can have a significant effect on respiratory function, and forward head posture can result in a change in muscle length tension [36]. The sternocleidomastoid, upper trapezius, and other neck muscles are not in optimal resting positions, because of shortening. Therefore, weakening of the sternocleidomastoid, scalene, and trapezius muscles is associated with a decrease in respiratory muscle strength [6,36]. Forward head posture increases the activities of the sternocleidomastoid and anterior scalene muscles during breathing and decreases forced vital capacity and the functioning of the respiratory system [37]. Forward head posture results in a change in muscle length-tension that is associated with the generating force of the respiratory muscles, such as the sternocleidomastoid and anterior scalene muscles [37]. According to the American Thoracic Society/European Respiratory Society, vital lung volume is limited by the weakening of inspiratory and expiratory muscles, which are directly affected by the loss of muscle force [12]. Kahlaee et al [38] also found that respiratory muscles were associated with cervical musculoskeletal dysfunction, including neck pain intensity, kinesiophobia, neck muscle strength, and forward head posture. Therefore, changes in forward head posture affects maximal inspiratory pressure among patients after open-heart surgery, and increases in forward head posture reduce maximal inspiratory pressure.
Additionally, we found an association between SEBQ scores and maximal inspiratory pressure in the present study. However, the SEBQ scores were not significantly different before and after surgery. The SEBQ is a subjective method used to assess the quality and quantity of uncomfortable respiratory sensations as well as a person’s perception of breathing [15]. As mentioned previously, the SEBQ self-measurement may be a risk factor for self-bias in the assessment [39,40]. Under normal breathing conditions, the diaphragm and external intercostal muscles perform the primary function of inspiration [40]. During labored breathing, the sternocleidomastoids, scalene, pectoralis major and minor, and internal intercostal muscles are the main inspiratory muscles. As a result, any stress on this structure will directly impact other elements, affecting the breathing mechanism and leading to dysfunctional breathing [40].
This study had some limitations. Short-term outcomes were examined only before surgery and discharge from the hospital (ie, postoperative day 7). Therefore, we did not explore the long-term effects of the angle on musculoskeletal and respiratory systems. Additionally, the relatively small number of patients in the study due to the COVID-19 pandemic meant that the relationship between the variables was unclear. However, although the sample size was relatively small, the study had sufficient power to determine the effects (retrospective statistical power, 0.95). For example, for the comparison between forward head angle before and after surgery, the retrospective statistical power was 0.95 (2-tailed alpha=0.05), and for the comparison between forward shoulder angle before and after surgery, the retrospective statistical power was 0.95 (2-tailed alpha=0.05).
Conclusions
After open-heart surgery, increased forward head posture and forward head angle was associated with reduced maximal inspiratory pressure, which may be associated with poor respiratory performance after surgery. Therefore, postoperative physiotherapy in this patient group should aim to improve postural changes.
Tables
Table 1. Clinical and characteristic data of the patients with open-heart surgery.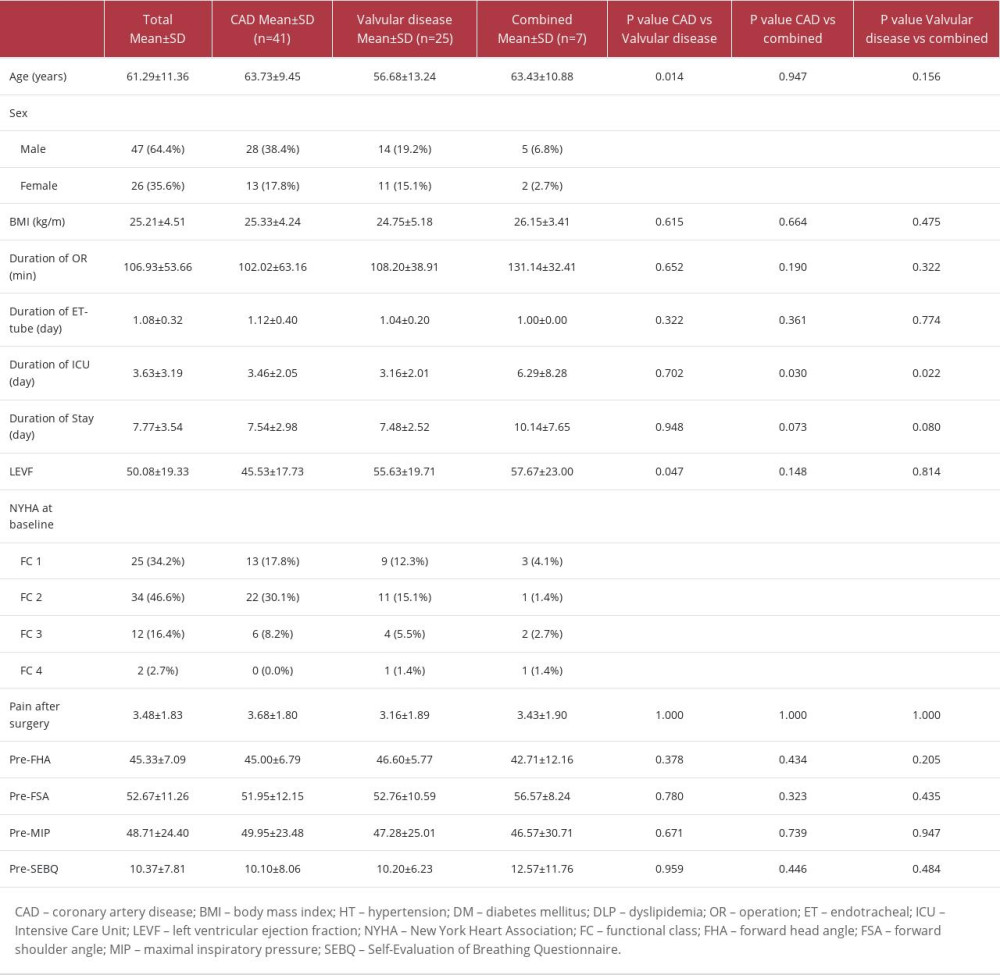 Table 2. Comparison of the mean value for forward head angle, forward shoulder angle, maximal inspiratory pressure, and SEBQ between pre- and postoperative (n=73).
Table 2. Comparison of the mean value for forward head angle, forward shoulder angle, maximal inspiratory pressure, and SEBQ between pre- and postoperative (n=73).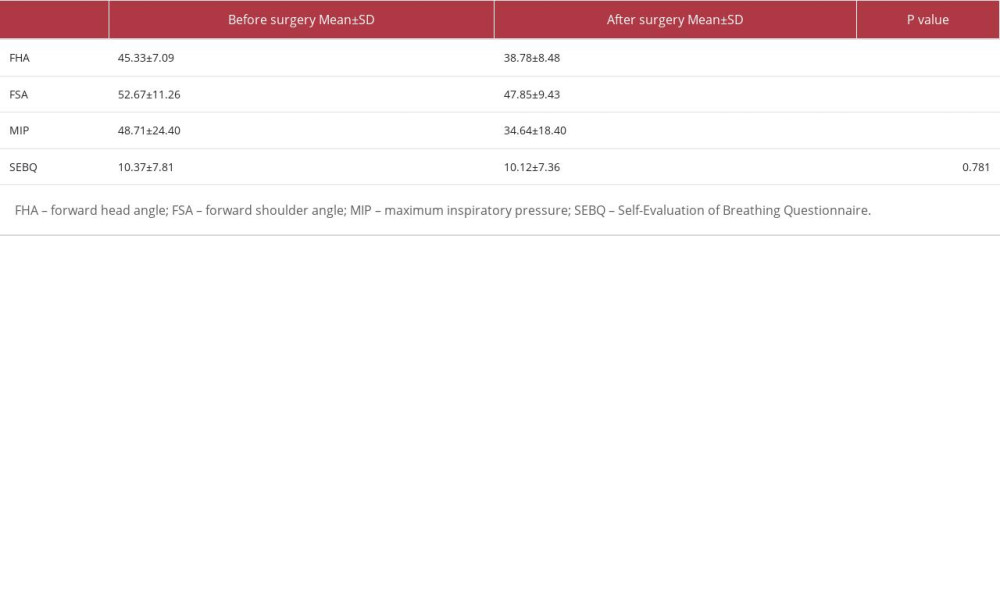 Table 3. Regression analysis predicting inspiratory muscle strength in patients after open-heart surgery (n=73).
Table 3. Regression analysis predicting inspiratory muscle strength in patients after open-heart surgery (n=73).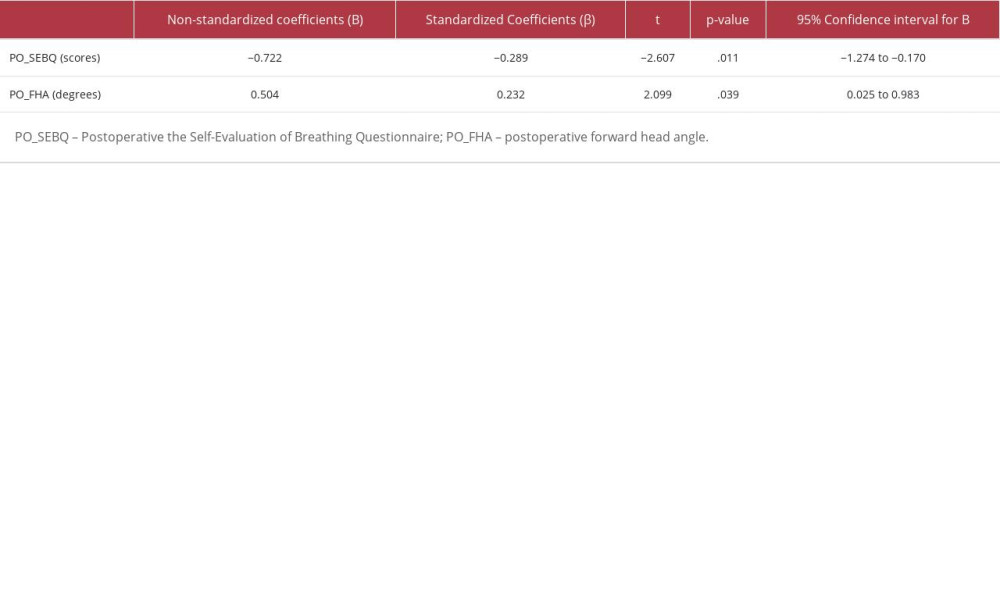
References
1. Mousavi S, Vasaghi-Gharamaleki B, Mirza-Mohammad K, Khosravian-Arab T, The prevalence and characteristics of shoulder pain in female patients with coronary artery bypass graft (CABG): Journal of Rehabilitation Science & Research, 2017; 4(1); 10-14
2. Riebe D, Ehrman JK, Liguori G, Magal MAmerican College of Sports Medicine: ACSM’s guidelines for exercise testing and prescription, 2018, Philadelphia, Lippincott Williams & Wilkins
3. Abolahrari S, Rojhani-Shirazi F, Rezayi A, Comparison of head, neck, and upper trunk postures between patients who have undergone coronary artery bypass grafting and healthy subjects: A pilot study: Journal of Rehabilitation Science & Research, 2020; 7(4); 167-72
4. LaPier TK, Schenk R, Thoracic musculoskeletal considerations following open heart surgery: Cardiopulm Phys Ther J, 2002; 13(2); 16
5. Sahrmann S, Azevedo DC, Dillen LV, Diagnosis and treatment of movement impairment syndromes: Braz J Phys Ther, 2017; 21(6); 391-99
6. Triangto K, Widjanantie SC, Nusdwinuringtyas N, Biomechanical impacts of forward head posture on the respiratory function: Indonesian Journal of Physical Medicine and Rehabilitation, 2019; 8(2); 50-64
7. Koseki T, Kakizaki F, Hayashi S, Effect of forward head posture on thoracic shape and respiratory function: J Phys Ther Sci, 2019; 31(1); 63-68
8. Han J, Park S, Kim Y, Effects of forward head posture on forced vital capacity and respiratory muscles activity: J Phys Ther Sci, 2016; 28(1); 128-31
9. Solakoğlu Ö, Yalçın P, Dinçer G, The effects of forward head posture on expiratory muscle strength in chronic neck pain patients: A cross-sectional study: Turk J Phys Med Rehabil, 2020; 66(2); 161-68
10. de Menezes TC, Bassi D, Cavalcanti RC, Comparisons and correlations of pain intensity and respiratory and peripheral muscle strength in the pre- and postoperative periods of cardiac surgery: Rev Bras Ter Intensiva, 2018; 30(4); 479-86
11. Pongpanit K, Kulchanarat C, Buranapuntalug S, Yuenyongchaiwat K, Correlation between change in respiratory muscle strength and cough ability in patients submitted to open-heart surgery: East J Med, 2019; 24(4); 401-4
12. American Thoracic Society/European Respiratory Society, ATS/ERS Statement on respiratory muscle testing: Am J Respir Crit Care Med, 2002; 166(4); 518-624
13. Caruso P, Albuquerque AL, Santana PV, Diagnostic methods to assess inspiratory and expiratory muscle strength: J Bras Pneumol, 2015; 41(2); 110-23
14. Howell S, Hill JD, Chest physical therapy procedures in open heart surgery: Phys Ther, 1978; 58(10); 1205-14
15. Courtney R, Dixhoorn JV, Questionnaires and manual methods for assessing breathing dysfunction: Recognizing and treating breathing disorders: a multidisciplinary approach, 2014; 137-46, Philadelphia, Elsevier
16. Puig-Diví A, Escalona-Marfil C, Padullés-Riu JM, Validity and reliability of the Kinovea program in obtaining angles and distances using coordinates in 4 perspectives: PLoS One, 2019; 14(6); e0216448
17. Whelton PK, Carey RM, Aronow WS, 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines: Hypertension, 2018; 71(6); 1269-324
18. Ruivo RM, Pezarat-Correia P, Carita AI, Intrarater and interrater reliability of photographic measurement of upper-body standing posture of adolescents: J Manipulative Physiol Ther, 2015; 38(1); 74-80
19. Kiesel K, Rhodes T, Mueller J, Development of a screening protocol to identify individuals with dysfunctional breathing: Int J Sports Phys Ther, 2017; 12(5); 774-86
20. Kshirasagar P, Doshi J, Parmar S, Prevelence of neck and shoulder posture abnormalities following coronary artery bypass graft surgery: Int J Sports Phys Ther, 2017; 6(2); 801-3
21. Bordoni B, Marelli F, Morabito B, Post-sternotomy pain syndrome following cardiac surgery: Case report: J Pain Res, 2017; 10; 1163-69
22. Huang AP, Sakata RK, Pain after sternotomy-review: Braz J Anesthesiol, 2016; 66; 395-401
23. Zubrzycki M, Liebold A, Skrabal C, Assessment and pathophysiology of pain in cardiac surgery: J Pain Res, 2018; 11; 1599
24. Sasseron AB, Figueiredo LC, Trova K, Does the pain disturb the respiratory function after open heart surgery?: Rev Bras Cir Cardiovasc, 2009; 24; 490-96
25. Mueller XM, Tinguely F, Tevaearai HT, Pain location, distribution, and intensity after cardiac surgery: Chest, 2000; 118(2); 391-96
26. Bellet RN, Lamb RL, Gould TD, Bartlett HJ, Prevalence of neuro-musculoskeletal pain and dysfunction in open-heart surgical patients preoperatively and at 6 and 12 weeks postoperatively: A prospective longitudinal observation study: Pragmat Obs Res, 2017; 8; 211-22
27. Kluszczyńska M, Młynarska A, Mikulakova W, Influence of frailty syndrome on kinesiophobia according to the gender of patients after coronary artery bypass surgery: Healthcare (Basel), 2021; 9(6); 730
28. Katijjahbe MA, Granger CL, Denehy L, Standard restrictive sternal precautions and modified sternal precautions had similar effects in people after cardiac surgery via median sternotomy (‘SMART’Trial): A randomised trial: J Physiother, 2018; 64(2); 97-106
29. Singla D, Veqar Z, Association between forward head, rounded shoulders, and increased thoracic kyphosis: A review of the literature: J Chiropr Med, 2017; 16(3); 220-29
30. Dehdilani M, Gol MK, Hashemzadeh K, Effects of stretching exercises on upper crossed syndrome in women after a coronary artery bypass graft: Crescent Journal of Medical and Biological Sciences, 2019; 6(3); 350-54
31. Liebenson C: Rehabilitation of the Spine: A practitioner’s manual, 2007, Philadelphia, Lippincott Williams & Wilkins
32. Netter FH: Atlas of human anatomy, 2019, Philadelphia, Elsevier
33. Reser D, Caliskan E, Tolboom H, Median sternotomy: Multimedia manual of cardiothoracic surgery: MMCTS, 2015
34. Liebsch V, Wilke HJ, Chapter 3. Basic biomechanics of the thoracic spine and rib cage: Biomechanics of the spine, 2018; 35-50
35. Roncada G, Dendale P, Linsen L, Reduction in pulmonary function after CABG surgery is related to postoperative inflammation and hypercortisolemia: Int J Clin Exp Med, 2015; 8(7); 10938-46
36. Zafar H, Albarrati A, Alghadir AH, Iqbal ZA, Effect of different head-neck postures on the respiratory function in healthy males: Biomed Res Int, 2018; 2018; 4518269
37. Kang JI, Jeong DK, Choi H, Correlation between pulmonary functions and respiratory muscle activity in patients with forward head posture: J Phys Ther Sci, 2018; 30(1); 132-35
38. Kahlaee AH, Ghamkhar L, Arab AM, The association between neck pain and pulmonary function: A systematic review: Am J Phys Med Rehabil, 2017; 96(3); 203-10
39. Ionescu MF, Mani-Babu S, Degani-Costa LH, Cardiopulmonary exercise testing in the assessment of dysfunctional breathing: Front Physiol, 2021; 11; 620955
40. Deshmukh MP, Palekar TJ, Manvikar N, Prevalence of breathing dysfunction in musculoskeletal complaints: A cross sectional study: Int J Health Sci Res, 2022; 12(2); 146-52
Figures
Tables
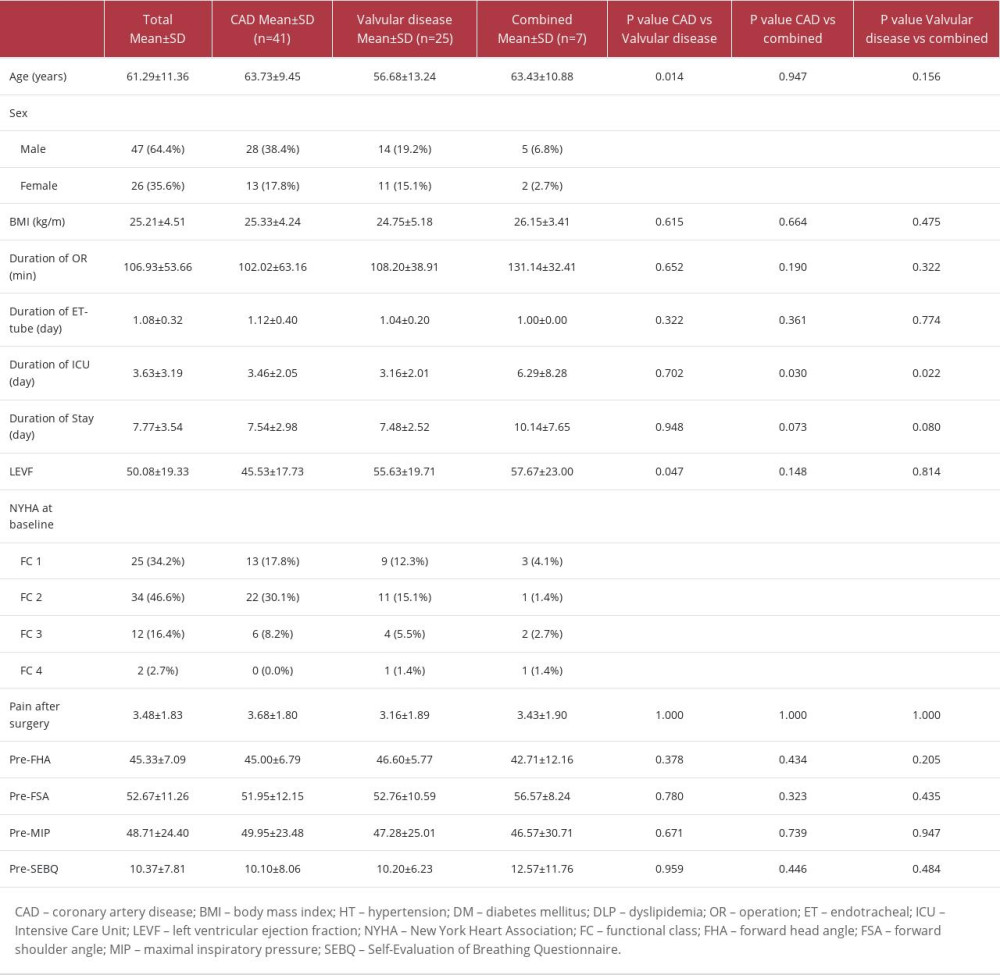 Table 1. Clinical and characteristic data of the patients with open-heart surgery.
Table 1. Clinical and characteristic data of the patients with open-heart surgery.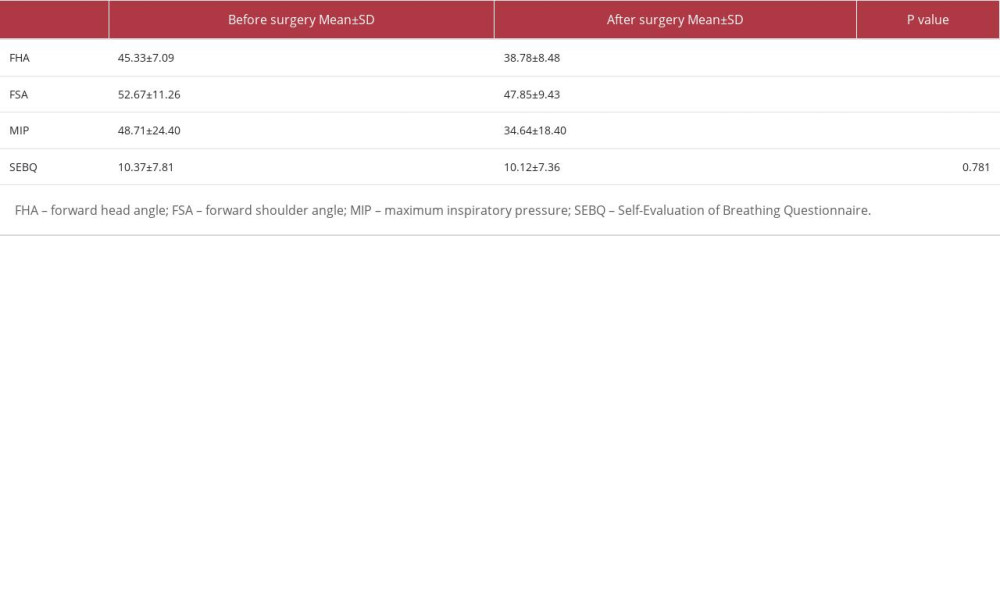 Table 2. Comparison of the mean value for forward head angle, forward shoulder angle, maximal inspiratory pressure, and SEBQ between pre- and postoperative (n=73).
Table 2. Comparison of the mean value for forward head angle, forward shoulder angle, maximal inspiratory pressure, and SEBQ between pre- and postoperative (n=73).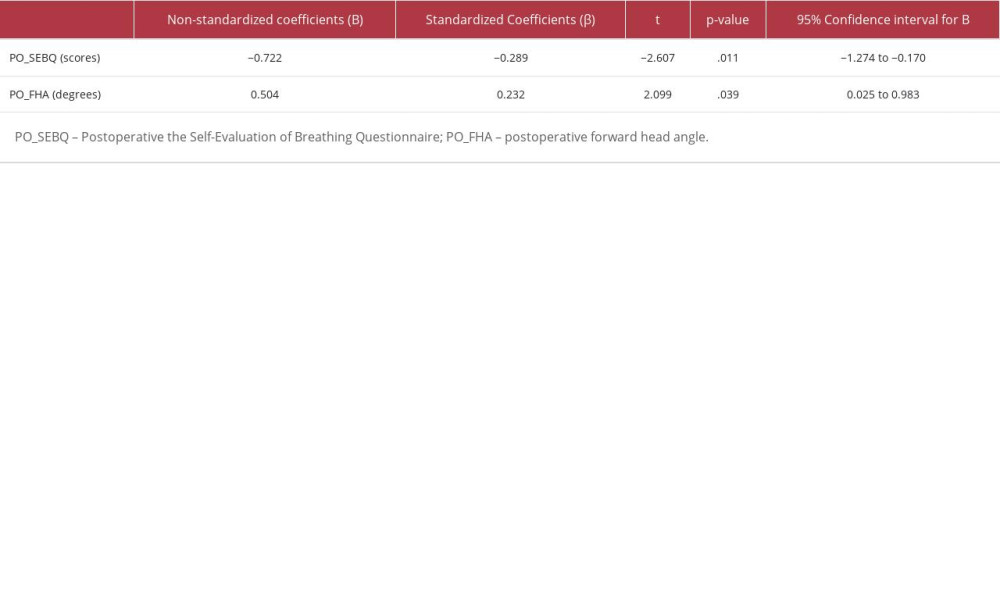 Table 3. Regression analysis predicting inspiratory muscle strength in patients after open-heart surgery (n=73).
Table 3. Regression analysis predicting inspiratory muscle strength in patients after open-heart surgery (n=73).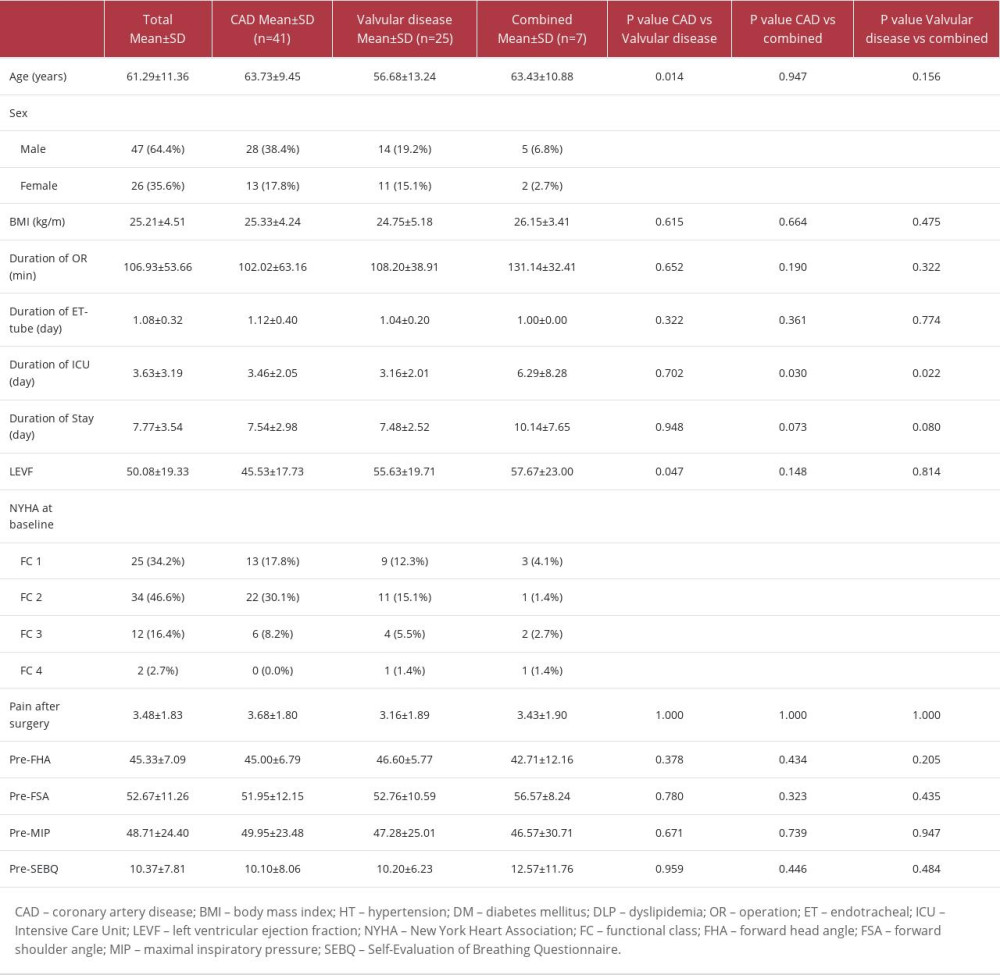 Table 1. Clinical and characteristic data of the patients with open-heart surgery.
Table 1. Clinical and characteristic data of the patients with open-heart surgery.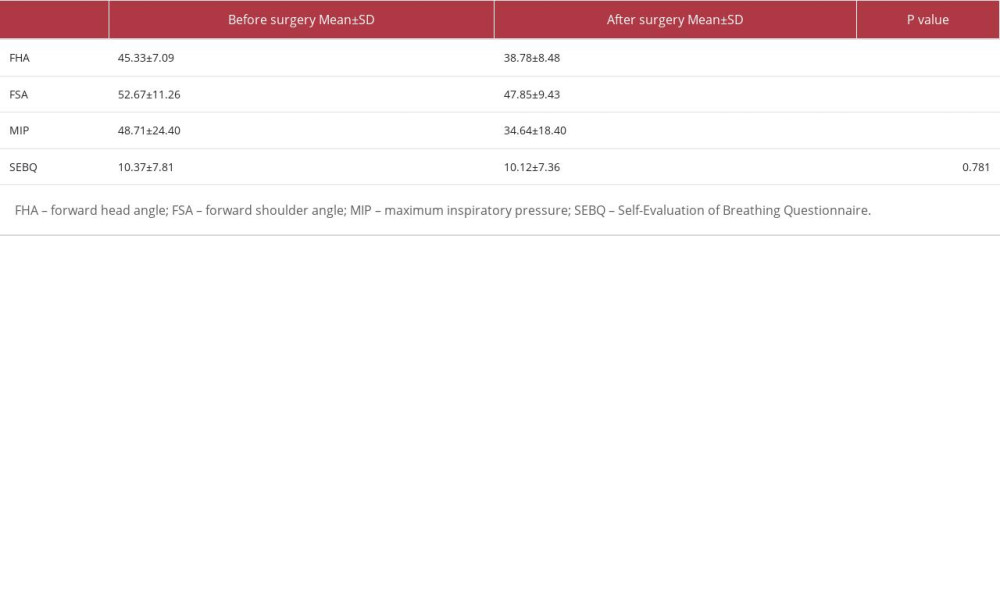 Table 2. Comparison of the mean value for forward head angle, forward shoulder angle, maximal inspiratory pressure, and SEBQ between pre- and postoperative (n=73).
Table 2. Comparison of the mean value for forward head angle, forward shoulder angle, maximal inspiratory pressure, and SEBQ between pre- and postoperative (n=73).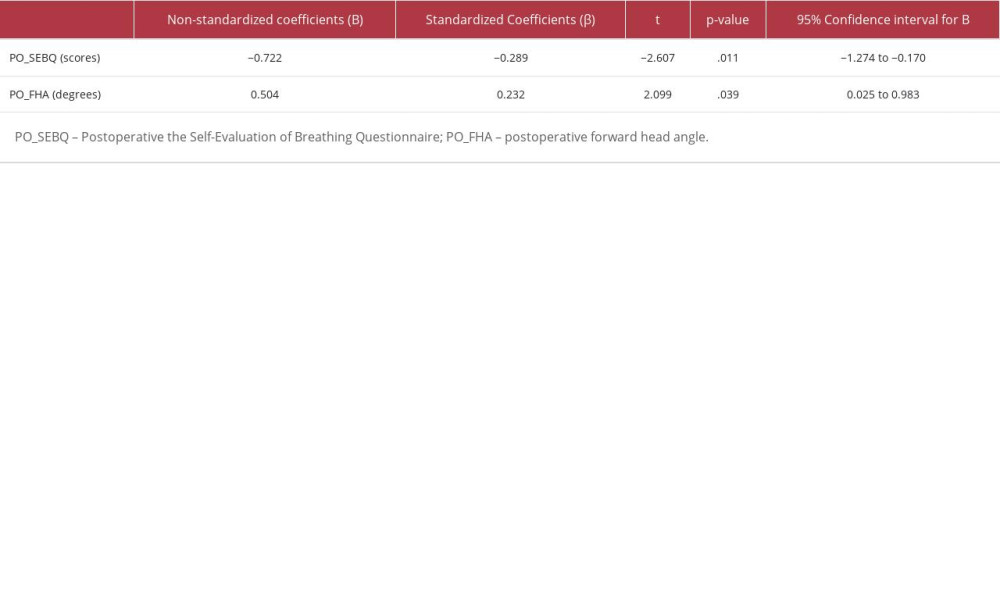 Table 3. Regression analysis predicting inspiratory muscle strength in patients after open-heart surgery (n=73).
Table 3. Regression analysis predicting inspiratory muscle strength in patients after open-heart surgery (n=73). Most Viewed Current Articles
15 Jun 2022 : Clinical Research
Evaluation of Apical Leakage After Root Canal Obturation with Glass Ionomer, Resin, and Zinc Oxide Eugenol ...DOI :10.12659/MSMBR.936675
Med Sci Monit Basic Res 2022; 28:e936675
07 Jul 2022 : Laboratory Research
Cytotoxicity, Apoptosis, Migration Inhibition, and Autophagy-Induced by Crude Ricin from Ricinus communis S...DOI :10.12659/MSMBR.936683
Med Sci Monit Basic Res 2022; 28:e936683
01 Jun 2022 : Laboratory Research
Comparison of Sealing Abilities Among Zinc Oxide Eugenol Root-Canal Filling Cement, Antibacterial Biocerami...DOI :10.12659/MSMBR.936319
Med Sci Monit Basic Res 2022; 28:e936319
08 Dec 2022 : Original article
Use of Estimated Glomerular Filtration Rate and Urine Albumin-to-Creatinine Ratio Based on KDIGO 2012 Guide...DOI :10.12659/MSMBR.938176
Med Sci Monit Basic Res 2022; 28:e938176