20 November 2023: Laboratory Research
Evaluation of the Effects of Digital Manufacturing, Preparation Taper, Cement Type, and Aging on the Color Stability of Anterior Provisional Crowns Using Colorimetry
Mohammed E. SayedDOI: 10.12659/MSMBR.941919
Med Sci Monit Basic Res 2023; 29:e941919
Abstract
BACKGROUND: Replicating the 3-dimensional (3D) color of natural teeth in artificial substitutes is challenging. Fixed dental prosthodontics require aesthetic, color-stable provisional restorations. Recent milling and 3D printing digital manufacturing techniques offer improved outcomes. This study assesses color stability in various digital manufacturing methods, tapers, and aging effects on anterior provisional resin restorations.
MATERIAL AND METHODS: Two all-ceramic tooth preparations on typodont teeth with 10° and 20° tapers were converted into experimental dies. Forty temporary crowns were manufactured using 3D printing and computer-aided design/computer-aided manufacturing (milling). Within these 2 groups, 10 crowns were cemented using a regular and clear provisional cement. All samples were thermocycled to simulate clinical use of 6 months. Color difference formula (CIEDE2000) indicated changes between before and after cementation (ΔE00[I]) and between after cementation and after thermocycling (ΔE00[II]). The color change was considered significant in terms of clinically perceptible (ΔE00 ≤0.62) and acceptable (ΔE00 ≤2.62) changes. One-way ANOVA (P value of less than 0.05) calculated overall differences, which were established using a Fisher post hoc test.
RESULTS: Crowns cemented with clear cement showed fewer color changes irrespective of the manufacturing technique or taper. Notably, only the 10° 3D-printed crown with clear cement had an imperceptible color change at the pre-/post-cementation phase. Meanwhile, the 10° and 20° milled crowns with regular cement exhibited unacceptable color changes after thermocycling.
CONCLUSIONS: For long‑term temporization in the aesthetic zone, properly optimized 3D-printed provisional restorations cemented with clear cement had better color stability.
Keywords: Computer-Aided Design, Crowns, Dental Implants, Dental Restoration, Temporary, Printing, Three-Dimensional, Prosthesis Coloring
Background
Replicating the 3-dimensional color attributes of natural teeth, including the fluorescence, opalescence, and metamerism, with an artificial substitute is a clinically challenging step [1]. Such shade perception generally develops with experience and practical training [2]. Fixed dental prosthodontics, including implant-supported restorations, require time-bound provisional restorations, the aesthetic appearance of which is fundamental to meet patient expectations [3]. The color stability of long-term provisional restorations is desirable, as color change indicates either aging or spoiled material [4]. All provisional restorations, in addition to performing tooth function, aid in determining the therapeutic effectiveness of the treatment chosen [5], with special examples being complete occlusal rehabilitation [6], anterior teeth crown lengthening [7], bone augmentation, and progressive implant loading [5]. In implants, provisional restorations correspondingly augment abutments and periodontium and guide tissue healing to produce a suitable emergence profile [8]. Color aesthetics, especially translucency, is highly influenced by the underlying supporting structure (natural tooth, implant abutment, and cast core) [9,10]. Food and Drug Administration-approved provisional materials [bisacryl and light cure composite resin, polyethyl methacrylate and polymethyl methacrylate (PMMA)] [11], have been used with different techniques: direct, indirect, and indirect-direct. PMMA, a commonly used provisional restoration, still exhibits exothermic polymerization, marginal inaccuracy, and degrading resin matrix [12]. Digital manufacture implicates cohesive production using computer organization. Introduction of additive (milling) and subtractive [3-dimensional (3D) printing] with subsequent novel provisional materials, including composites, polymer resins as polyether ether ketone, and PMMA, have reduced many of the drawbacks associated with conventional provisional fabrication techniques and materials [13]. The economic unsustainability of computer-assisted design and computer-assisted machining (CAD/CAM) clinical armamentarium has led to the development of affordable 3D-printing machines in private clinics and dental laboratories [14]. Milled provisional restorations have been reported with improved mechanical properties, while additive provisional restorations report accuracy (occlusal anatomy replication), faster technology (15–20 min), [15] and reduced cost.
Optical properties influencing color stability have been studied for both CAD/CAM and 3D-printed denture bases and provisional resins. Al Dwairi et al investigated 3 brands of printed resin against heat-cured PMMA resin and concluded that one of the printed resins, Asiga Dentamodel, had lowest surface roughness (0.19±0.03 μm) [16]. Di Fiora et al examined bacterial adhesion on heat-polymerized PMMA, CAD/CAM-milled, and 3D-printed PMMA, with CAD/CAM specimens showing the lowest bacterial adhesion before and after polishing [17]. The color stability of milled PMMA denture base resins is also substantially supported by recent studies [18,19]. Elagra et al reported that milled provisional PMMA resin had superior color stability after 7 days [20]. Song et al reported that milled and printed provisional PMMA resins have color stability for 8 weeks, after which they deteriorate rapidly [21]. Tahayeri A et al stressed the significance of 3D printer optimization and calibration in terms of printer orientation and print thickness for most desirable properties [15]. Resin inks also require light optimization in 3D printing, with darker inks set to higher light intensity to cure greater depths than a fully translucent material. Such critical determinants are seen lacking in studies that compare milled PMMA with 3D-printed resin, with most being performed at built-in programmed parameters. Milled PMMA provisional resins have also been subsequently reported to have less porosity [22], less water sorption and solubility [23], and more surface hardness [24], which make them more suitable for long-term provisional restorations and worthy of further investigation in the light of recent evidence.
The clinical color matching (shade selection) process seems to have been misinterpreted and misrepresented. The process starts at the beginning of treatment, which is conveyed to the laboratory technician at a later stage, the try-in. The technician then fabricates the definitive shade accordingly. After the shade selection stage, 2 significant factors will further influence the selected shade. The definitive cement color and thickness influence the color in laminates [25], fixed partial dentures [26], and implant abutments [27], which led to the development of translucent cements. Many dental cements are available commercially, but clinically they are broadly classified as provisional (temporary) and definitive (permanent) cements, with each group having a wide variety of sub-classes. Highly translucent cement shows less influence on the original restoration color [26]. Despite the recommended cement thickness of 25 to 40 μm for provisional/definitive restorations, the earlier milled provisional restorations (CEREC) have reported higher gaps of 47 to 193 μm [27], and continue to be in the range of 110 to 125 μm in present-day provisional resins [28]. Anterior provisional restorations must be translucent for a life-like appearance. Milled polymer provisional restorations with a thickness of 1 mm have variable translucency under different lights (visible and blue) [29]. Since translucency decreases with increased restoration thickness [30], it can be difficult to mask the underlying color of implant abutments merely by adjusting thickness. 3D-printed resins inherit high translucency due to their lower viscosity requirement (filler size/content and photo initiators) [9,31] which makes them ideal for long-term provisional restorations in implant prostheses. Another significant factor for color stability is aging in dry/aqueous environments. Therefore, to redefine durable provisional restorations, these 2 factors need to be considered during any experimental research. Most research avoids confounding variables, which is not the case clinically, where all factors contribute to the final outcome.
In this study, we aimed to evaluate the effects of 2 digital manufacturing techniques (milled and 3D-printed), preparation taper (10° and 20°), provisional (temporary) regular and clear cement, and aging (5000 thermal cycles representing 6 months of aging) on the color stability of anterior provisional resin restorations using colorimetry. The objectives were to identify the most suitable provisional long-term PMMA resin restoration for conventional fixed dental prosthodontics, including implant-supported restorations. The 2 different tapers would provide 2 different thicknesses of the temporary crowns that are applicable to implanting provisional restorations. We hypothesized that there would be significant differences between the investigated variables, with the null hypothesis stating that there would be no influence of these variables on color changes.
Material and Methods
ETHICS:
The research protocol was approved by the research board unit at the College of Dentistry, Jazan University (Reference number: CODJU-2207F). All materials used during this study has been approved by the Saudi Food and Drug Authority under its various regulations.
STUDY DESIGN:
This in vitro study followed a comparative experimental design and was conducted in the first and second quarter of 2023. The study involved 2 distinct stages. The first stage was exclusively dedicated to fabrication of sample specimens for the study, including the planned interventions of tooth preparation taper, milled and 3D-printed manufacturing, cementation, and aging. The second stage involved measuring color values and was interspersed between various aspects of the first stage, at before cementation/after cementation and after cementation/after aging.
OPERATIONAL DEFINITIONS:
For this research project, certain scientific terms were defined exclusively for the context of the study. The word “shade” used in the study description meant a particular hue: the basic color of an object, or any of its variations, such as yellowish shade of blue color. The word “chroma” indicated the intensity of a particular hue, while the word “value” was applied to the relative brightness (white) or darkness (black) of color. The term “preparation taper” identified the total ratio of differences in the diameters of different sections of a prepared tooth between various sections, which was also identified by the convergence angle from the basal surface.
SAMPLE PREPARATION, SELECTION, AND GROUPING:
The sample size estimation was determined by calculating the assumption of 80% study power and 5% alpha error, which determined that for each group the minimum sample size should be 10 per group, which was increased to 11; the extra specimen would replace any specimens with a laboratory processing error [32].
FABRICATION OF MODELS AND PROVISIONAL CROWNS:
A detailed description of the experimental materials used in this study is presented in Table 1. Figure 1 presents the flowchart for study methods and group distribution. Two standard maxillary (right central incisor) prefabricated typodont teeth (Practicon, Greenville, NC, USA) were mounted on their respective typodont bases, with teeth of acrylic and soft tissues of silicone rubber. A polyvinylsiloxane (Lab-Putty, Cotene/Whaledent AG, Switzerland) index was then adapted over the unprepared typodont teeth with extensions over the adjacent teeth. This was used to verify the dimensions of the reduction using a graduated periodontal probe (millimeters) once tooth preparation was accomplished [33]. A tooth preparation for receiving an all-ceramic crown was then performed on each experimental tooth using a diamond bur (Flat end, 6856 314 016, Komet, Germany) on a high-speed air driven handpiece (KaVo do Brasil Ind. Com. Ltda., Joinville, SC, Brazil), which in turn was fixed to a dental cast surveyor (A3005 Surveyor Type A; Dentalfarm). The amount of tooth reduction included a 2-mm incisal reduction, 1. 2 to 1. 4-mm biplanar (facial and lingual) axial reduction, and 1-mm shoulder width. The different tapers were incorporated using the reciprocal (10° and 20°) of the taper within the cutting bur, with the bur held parallel to the tooth surface (labial, lingual, and proximal). The prepared teeth were then finished for sharp line and point angles followed by scanning with a benchtop scanner (3Shape A/S Holmens Kanal 7 1060 Copenhagen/Denmark). The scanned data were transferred by software (Asiga Composer software), which produced the 2 master dies (10° and 20°) (Figure 2A–2D) using polyetherimide resin (Asiga Dentamodel Alexandria, Australia). The dies were subjected to an accuracy check with the help of a digital protractor and verified under the stereomicroscope (Amscope, CA, USA). After verifying the parameters for tooth preparation and desired taper, each die was further scanned using the benchtop scanner to generate a standard tessellation language (STL) file for respective prototyping (milled and 3D printing). At this stage, 40 working models were assigned to each manufacturing group (milled and 3D printing) under 2 subgroups of 10° and 20° taper, with 20 in each group (Figure 2A–2D). In both groups, the crowns were designed to have a uniform cement space of 30 μm. A loop was also designed at the incisal edge which would help standardize the specimen positions during color measurement within the calibration box and prevent contamination of the labial surface during handling. Color measurement was done for each coded crown, which served as the baseline (control) to subsequent color measurements (before cementation).
CAD/CAM-MILLED PROVISIONAL CROWN FABRICATION: For generating the STL files for milled crowns, the respective die was first powdered using the scan spray (VITA CEREC; Bad Sackingen, Germany) with the aid of a propellant that offered an even, thin powder layer. The provisional crowns were then designed using software (EXOCAD, GmbH, Darmstadt, Hessen, Germany). PMMA resin disks (Whitepeaks Dental Solutions GmbH Wesel, Germany) of standard size (98/14) and shade A2 were used for fabrication of all specimens in this group (n=40). High speed steel tools, 1 mm and 2 mm wide, high shear, and 5° edge rake angle/2° clearance angle, were used to mill the provisional crowns under wet conditions, as recommended by the manufacturer. Any sample with a visible crack or other defect was discarded and replaced with a new one. The finishing of the provisional crowns was accomplished using the recommended manufacturer kit (K0330 PMMA: Adjusting, Finishing & Polishing, KP, Brasseler USA). Polishing of each specimen was done with an automatic polisher (Spectrum System 1000-SS1000; LECO Corp, St. Joseph, MI, USA) using a mixture of pumice and water slurry (Pumice fine; Benco Dental) as per recommendations for 90 s, followed by fine polish using paste (Fabulustre; Grobet USA) [34]. The final thickness of the crown was measured (1.5±0.04 mm) with digital callipers, followed by ultrasonic cleaning (Eltrosonic Ultra Cleaner 07–08; Eltrosonic GmbH) for 10 min before drying in open air.
3D-PRINTED PROVISIONAL CROWNS: The provisional crowns in the 3D-printed groups were printed using a digital light processing 3D printer (Asiga Pty Ltd. Alexandria, Australia) and 3D print resin (Asiga DentaTooth, Alexandria, Australia; shade A2). The printer was first optimized for different parameters, namely resolution (62-μm pixel size), accuracy and precision, build volume (X, Y, Z=119×67×76 mm; 4.68×2.63×3 inches), and surface finish, according to the recommended method [21]. Printing accuracy was established by comparing printed sample dimensions against CAD dimensions using a calibrated digital calliper (±0.1 mm; zeroing/re-zeroing of caliper to set zero) for length, thickness, and width of a test sample of rectangular block. The light intensity for polymerizing the resin ink was determined as a wavelength of 385 nm using a power meter (Molectron Coherent, Santa Clara, CA) that was placed inside the printing chamber. For printing the provisional crowns using PMMA resin ink, the printing layer thickness was set to 100 μm using the resin parameter “white’ for provisional restoration samples. The curing of the resin was accomplished using a post-curing lightbox (NK Optik Otoflash G171), as recommended and provided by the manufacturer, for 2000 flashes twice. Each sample was washed in fresh water at room temperature for 60 min. The finishing and polishing were done as per manufacturer’s recommendations, which specify using routine finishing/polishing procedures. To minimize the effect of finishing/polishing a common finishing/polishing protocol was followed, as mentioned above.
SUBGROUPING BASED ON THE CEMENTATION OF CROWNS AND THERMOCYCLING:
The provisional crowns in each digitally manufactured group (milled and 3D printed; 10° and 20° taper) were further subdivided into 4 subgroups based on the provisional non-eugenol (Temp-Bond) cement used: regular (conventional) cement and clear cement. All together, this division yielded 8 subgroups: 10° milled regular (group 1MR); 20° milled regular (group 2MR); 10° milled clear (group 1MC); 20° milled clear (group 2MC); 10° 3D-printed regular (group 1PR); 20° 3D-printed regular (group 2PR); 10° 3D-printed clear (group 1PC); and 20° 3D-printed clear (group 2PC) (Table 2). Each crown was first subjected to quality control for fit and stability on their respective dies. This was performed by a team of prosthodontists who were blinded to the study outcome. Any specimens that were loose and had marginal discrepancy were rejected and remade. The provisional cement for each subgroup was injected into the respective crowns using the Automix syringe system, as provided by the manufacturer, and removal of excess cement was done with a scalier tip and cotton pellet. Each crown was subjected to a standard load of 5.0 newton (N) [35]. The second color measurement was performed at this stage, after cementation, which was compared with the earlier measurements before cementation. Following the second color measurement, all the specimens were subjected to thermocycling between 5° and 55°, with a dwell time of 10 s and 5000 thermal cycles to represent 6 months of oral usage [36]. The final color measurement was performed after thermocycling was completed.
MEASURES, DATA COLLECTION, EVALUATION, AND ANALYSIS:
All experimental specimens underwent color measurement with a colorimeter (Hangzhou CHNSpec Technology Co Ltd., Hangzhou, China). The influence of external light or room illuminants on the color measurement was nullified by measuring in a calibration box (0 calibration standard), with the box having a white background [37]. The influence of the changing positions of colorimeter was overcome by using a custom-made silicone index (Speedex, Coltène, Switzerland) that conformed to the opening of the colorimeter tip diameter. The colorimeter used had specifications of a 5-mm diameter tip, 94.65% accuracy, and 0.872 to 0.914 repeatability upon pilot testing with a vita ceramic shade (A2) tab. For each set of measurements, the calorimeter was first calibrated to its tool, which was provided by the manufacturer, and following the manufacturer’s instructions. The shade of each experimental specimen was measured at the middle third of the crown. A uniform position for each specimen was ensured by using gradations on an external index that would help position each sample in the same place using the loop within each specimen.
For each sample, the color measurement included values corresponding to CIELAB metric parameters; L* (value) indicates light or dark; 100/0 = completely white/completely black; C* (chroma) indicates red-green, and H* (hue) indicates yellow-blue chromatic coordinates, with each coordinate designated a positive (+) and a negative sign (−), which in turn denoted the direction of the examined color: C* = green (− C), and red (+ C) axis, and H* = blue (−H), and yellow (+H) axis [38]. The color measurements were recorded by a single double-blinded operator in temperature- and humidity-controlled conditions during daytime, as pre-cementation, post-cementation, and post-thermocycling, and each measurement was repeated 3 times for each specimen, with the final measurement being the average of the 3 repeated measurements.
STATISTICAL ANALYSIS:
Differences in color between pre-cementation, post-cementation, and post-thermocycling measurements were determined using the CIEDE2000 (DE00 or ΔE) formula (95% confidence interval) [38]:
where ΔL*, ΔC*, and ΔH* represent CIELAB metric differences in value, chroma, and hue (pre-cementation vs post-cementation vs post-thermocycling), respectively, SL, SC, and SH denote the weighting functions for each metric (value, chroma, and hue), and KL, KC, and KH are parametric factor values that need to be adjusted according to viewing parameters (texture, background) for value, chroma, and hue components. ΔR denotes an interaction between chroma and hue differences. The values used for the parametric factor (KL, KC, and KH) in this study were set to 1, while the interaction between hue and chroma differences Rt were set to 0. This study used the CIEDE2000 value evaluation in terms of perceptibility and acceptability. Color difference (DE00 or ΔE00) was considered to be significant if the ΔE00 value was above 0.62 (clinically 50: 50% perceptibility threshold) and ΔE00 value was above 2.62 (clinical 50: 50% acceptability threshold) [39]. Changes in color were thus considered to be significant for perceptibility and acceptability by selecting the resin and evaluating its clinical performance [40]. All calculations using the formula were performed manually and entered into the Microsoft Excel sheet. The color difference ΔE00(I) indicates the differences between pre-cementation and post-cementation measurements, while ΔE00(II) indicates the difference between post-cementation and post-thermocycling measurements. Means and standard deviations for each group specimen (n=10) were calculated using SPSS for Windows Version 25 (IBM Corp., Armonk, NY, USA). Normality tests for data distribution was performed using the Shapiro-Wilk test. The differences in means between the 2 time intervals (pre-cementation and post-cementation) and (post-cementation and post-thermocycling) of the study groups were calculated using one-way ANOVA. Post hoc least significant different was used for individual group comparison of ΔE00(I) and ΔE00(II). A P value of <0.05 was considered to be statistically significant for differences between the groups.
Results
PRE- AND POST-CEMENTATION CHANGES:
The least amount of color change within the set perceptible threshold (0.62±0.01) was observed in group 1PC (0.57±0.29), while all other groups crossed the perceptible threshold (0.62±0.01), with group 1MR (1.47±0.65) and group 2MR (1.30±0.59) showing the highest differences between pre- and post-cementation measurements. Groups 1MC, 2MC, and 2PC had color difference values that were within the perceptible threshold. Descriptive analysis of the color change ΔE00(I) pre- and post-cementation had a 95% confidence interval in the group with upper bounds between 0.78 and 1.93 and lower bounds between 0.36 and 1.00, and the samples were equally distributed. The 95% confidence interval, with upper and lower bound ranges of values, shows the expected number of times the values will fall between the selected percentage if the study was reproduced.
POST-CEMENTATION AND POST-THERMOCYCLING CHANGES:
Table 4 presents the mean scores for color differences ΔE00(II) that were observed among the studied groups between post-cementation and post-thermocycling (6 months of clinical use) measurements. The least clinically perceptible color changes ΔE00(II) were observed in group 1PC (1.31±0.50), while the highest changes were observed in group 1MR (3.67±0.68). Group 1MR (3.67±0.68) and group 2MR (2.97±0.79) showed color changes that were clinically unacceptable (clinical acceptability threshold of 2.62). All groups that were cemented with clear cement showed color differences that were clinically perceptible (0.62) but fell within the acceptable range (2.62). Descriptive analysis of the color change ΔE00(II) between post-cementation and post-thermocycling measurements reported at 95% confidence interval in the group with upper bounds between 1.66 and 4.15 and the lower bounds between 0.10 and 0.25, and the samples were equally distributed. The net amount of color difference changes between ΔE00(I) (the color difference between pre-cementation and post-cementation measurements) and ΔE00(II) (the color difference between post-cementation and post-thermocycling measurements) among each color-coded group in ascending order is shown in Figure 3. Group 1PC showed the least amount of color change from post-cementation to post-thermocycling (0.734±0.519), while group 1MR had the highest changes (2.204±1.55). All groups that were cemented with clear cement showed relatively less color change than the groups cemented with regular cement between the 2 observed time intervals. The differences (between/within) for all the groups were found to be statistically significant at the value of P≤0.05 for both observed color differences (ΔE00(I): pre-cementation/post-cementation; and ΔE00(II): post-cementation/post-thermocycling; Table 5). Post hoc test results (Fisher’s least significant difference test; Table 6) after multiple comparison between the 8 experimental groups at 2 different intervals showed the differences that were observed between the groups. Group 1MR was found to be statistically significantly different from all other groups except group 2MR for ΔE00(I).
Discussion
STRENGTHS AND LIMITATIONS OF THE STUDY:
The study strengths include the simulation of clinical sequence for long-term provisional restorations and a methodology that highlighted the significance of optimization and calibration of 3D printing. The study also included variables that are applicable to both conventional fixed dental prosthodontics and implant-supported provisional restorations. Limitations of the study include the low number of provisional material brands investigated, the use of one brand of cement, and not having investigated the influence of common colorants. However, the authors feel that the role of solutions does not actually reflect the ability of the provisional material and are not fair to manufacturers. Further specialty studies are required to investigate the effect of optimization of 3D printers on various properties of PMMA resin.
Conclusions
In this study, we investigated only few resins, cements, and manufacturing units; therefore, the results of this study cannot be generalized. With experimental conditions similar to those that are presented in this study, the following can be concluded: (1) The color changes ΔE00(I) and ΔE00(II) were higher when Temp-Bond regular non-eugenol cement was used; (2) the color change ΔE00(I) at pre- and post-cementation measurements was higher with 10° milled taper crowns than with 20° milled taper and 3D-printed crowns; milled crowns with either 10° or 20° and cemented with regular provisional cement had color changes that were clinically unacceptable after thermocycling; and (4) for long-term provisional fixed dental prosthodontics with restorations in the anterior region, the 3D-printed PMMA resin is recommended, and for provisional implant abutments, both milled and 3D-printed PMMA provisional resins can be used, provided the luting agent for both is clear cement.
Figures
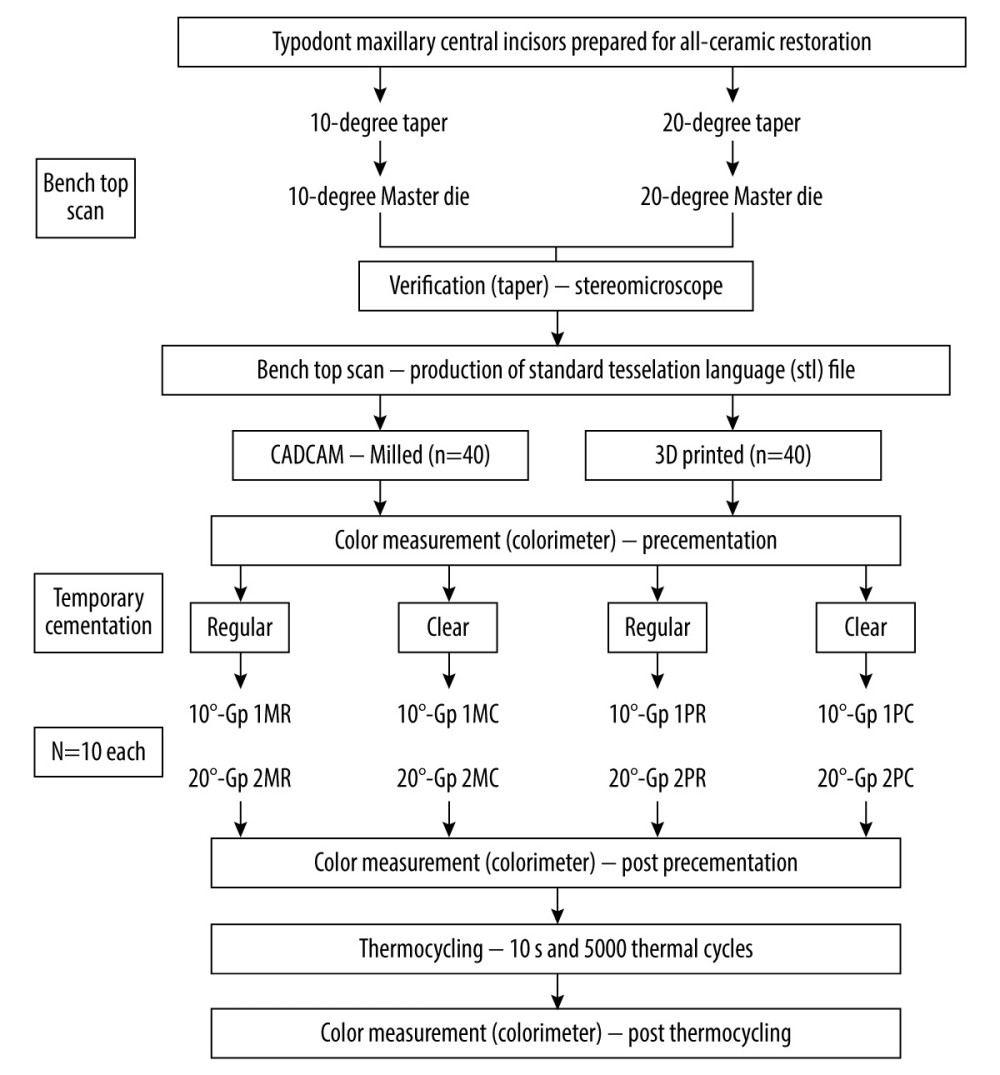 Figure 1. Flowchart showing study sampling and group distribution. Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corp.).
Figure 1. Flowchart showing study sampling and group distribution. Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corp.). 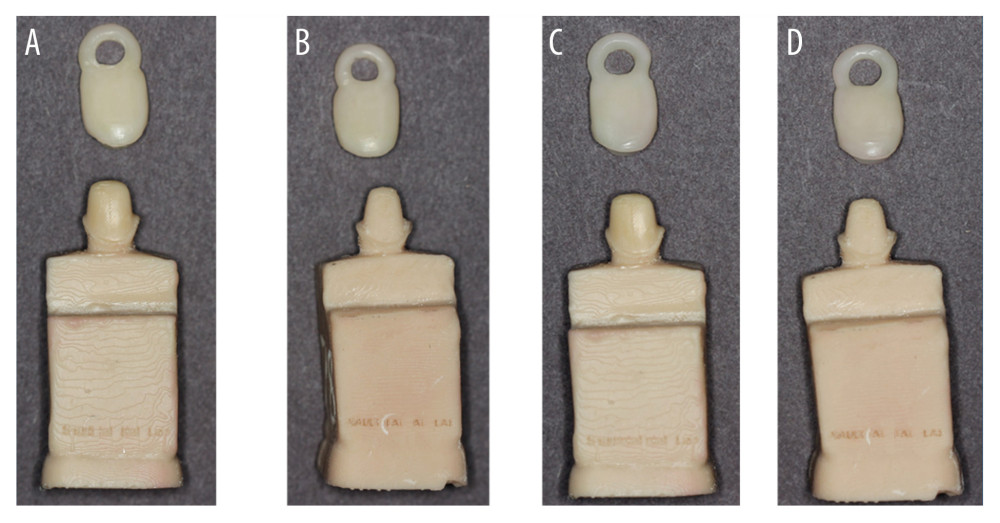 Figure 2. Working models (A) 10° taper milled crowns (B) 20° taper milled crowns (C) 10° taper 3D printed crowns, (D). 20° taper 3D printed crowns. Figure edited and labelled using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corp.).
Figure 2. Working models (A) 10° taper milled crowns (B) 20° taper milled crowns (C) 10° taper 3D printed crowns, (D). 20° taper 3D printed crowns. Figure edited and labelled using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corp.). 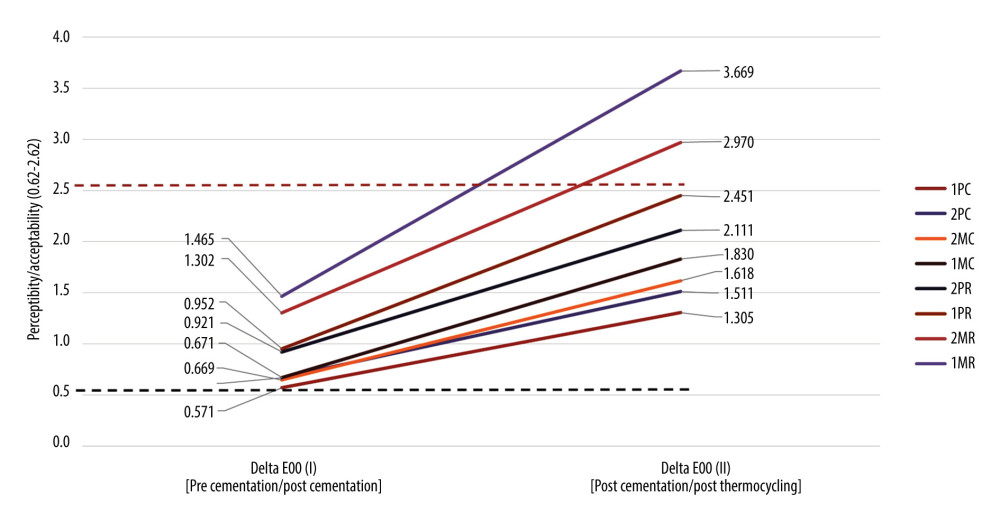 Figure 3. Graphic presentation of mean values for color differences ΔE00(I) (pre- and post-cementation) and ΔE00(II) (post-cementation and post-thermocycling) among studied groups (ascending order of noted color changes among 2 time intervals). Figure created using MS Excel sheet, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corp).
Figure 3. Graphic presentation of mean values for color differences ΔE00(I) (pre- and post-cementation) and ΔE00(II) (post-cementation and post-thermocycling) among studied groups (ascending order of noted color changes among 2 time intervals). Figure created using MS Excel sheet, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corp). Tables
Table 1. List of materials, instrumentation, and manufacturers.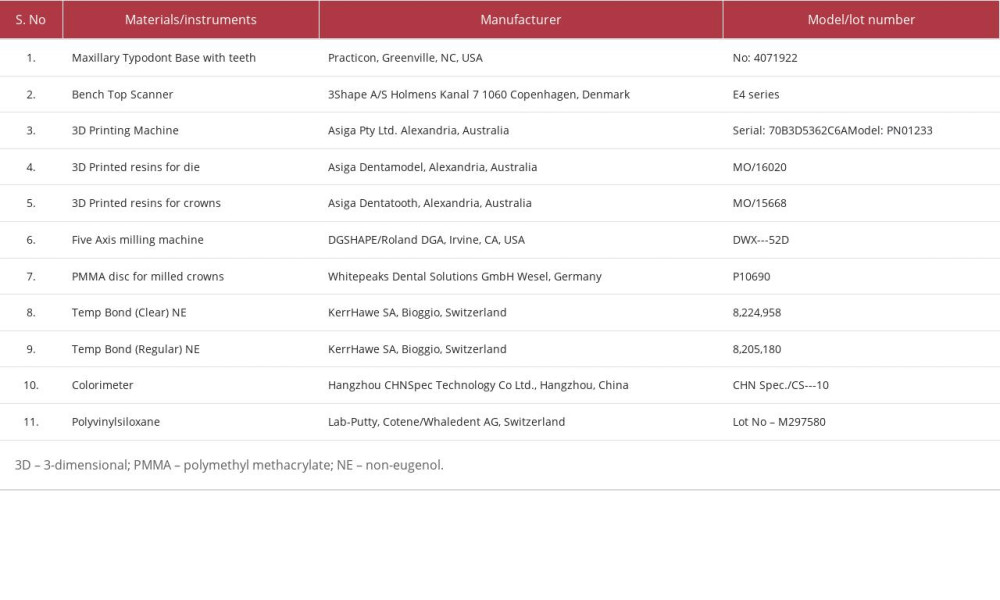 Table 2. Group distribution based on manufacturing, degree of taper, and provisional cement used.
Table 2. Group distribution based on manufacturing, degree of taper, and provisional cement used.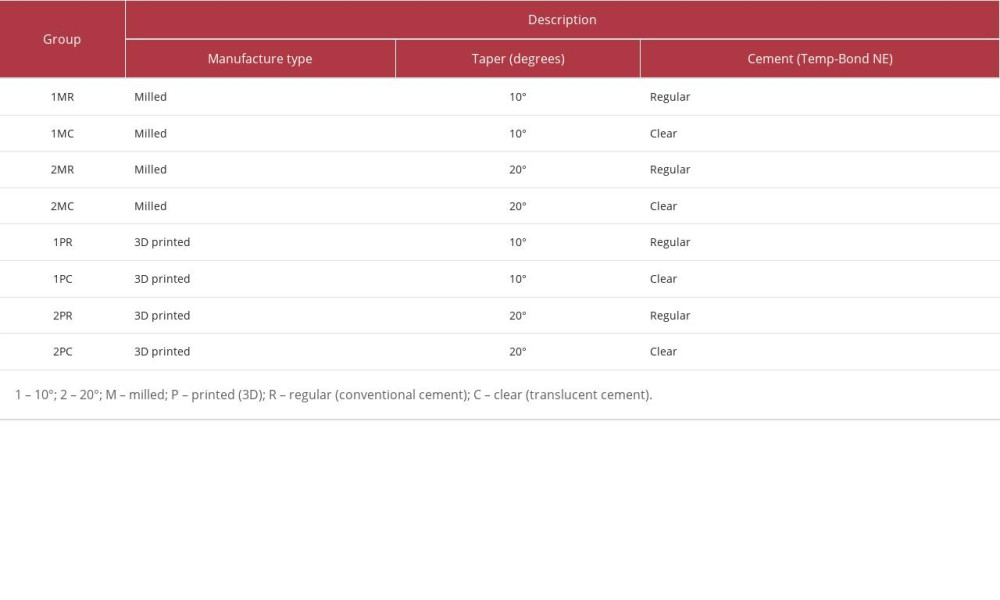 Table 3. Descriptive analysis of the color change ΔE00(I) before cementation and after cementation reported with 95% confidence intervals, mean±SD, and median (minimum, maximum).
Table 3. Descriptive analysis of the color change ΔE00(I) before cementation and after cementation reported with 95% confidence intervals, mean±SD, and median (minimum, maximum).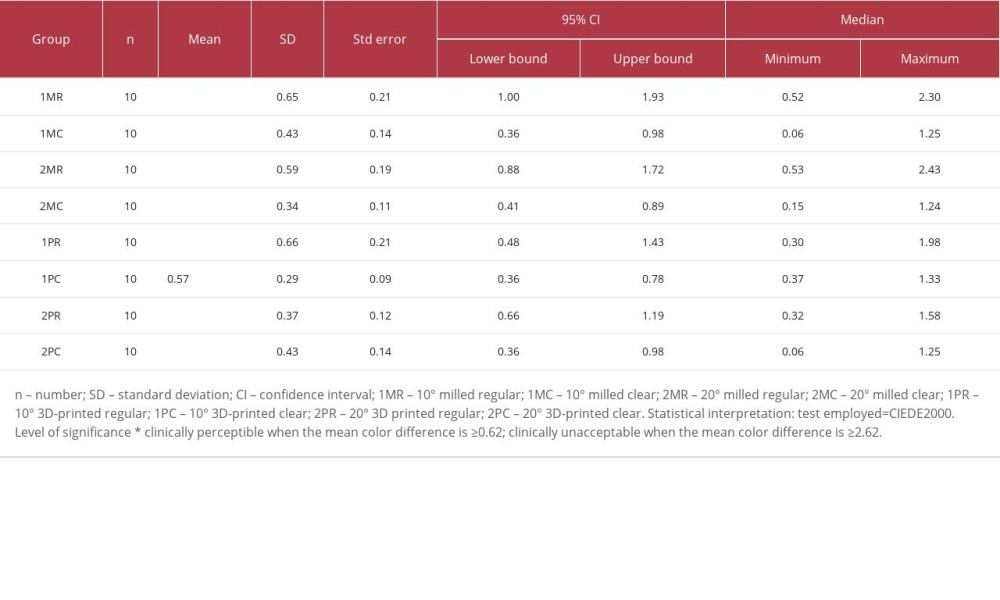 Table 4. Descriptive analysis of the color change ΔE00(II) after cementation and after thermocycling reported with 95% confidence interval, mean±SD, and median (minimum, maximum).
Table 4. Descriptive analysis of the color change ΔE00(II) after cementation and after thermocycling reported with 95% confidence interval, mean±SD, and median (minimum, maximum).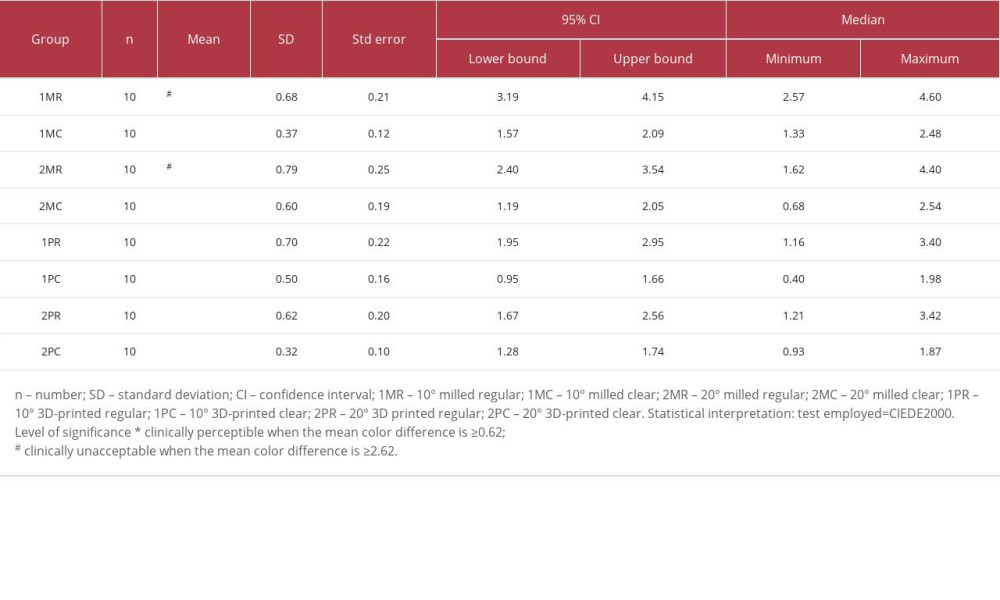 Table 5. One-way ANOVA for comparison of color differences (between and within) observed among studied groups.
Table 5. One-way ANOVA for comparison of color differences (between and within) observed among studied groups.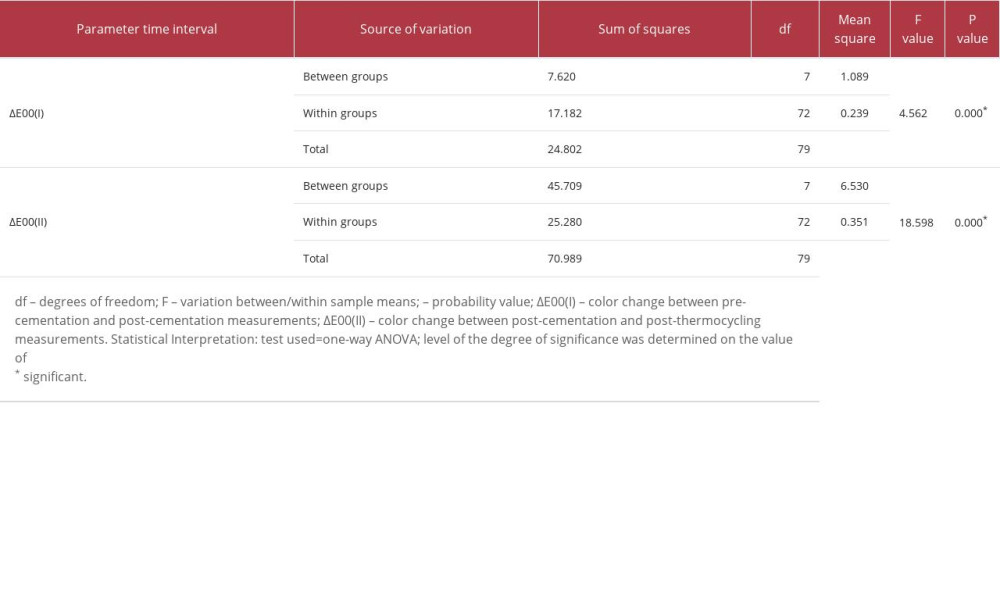 Table 6. One-way ANOVA Fisher’s least significant difference post hoc test for individual group comparison with other groups for 2 different time interval color differences ΔE00(I) and ΔE00(II).
Table 6. One-way ANOVA Fisher’s least significant difference post hoc test for individual group comparison with other groups for 2 different time interval color differences ΔE00(I) and ΔE00(II).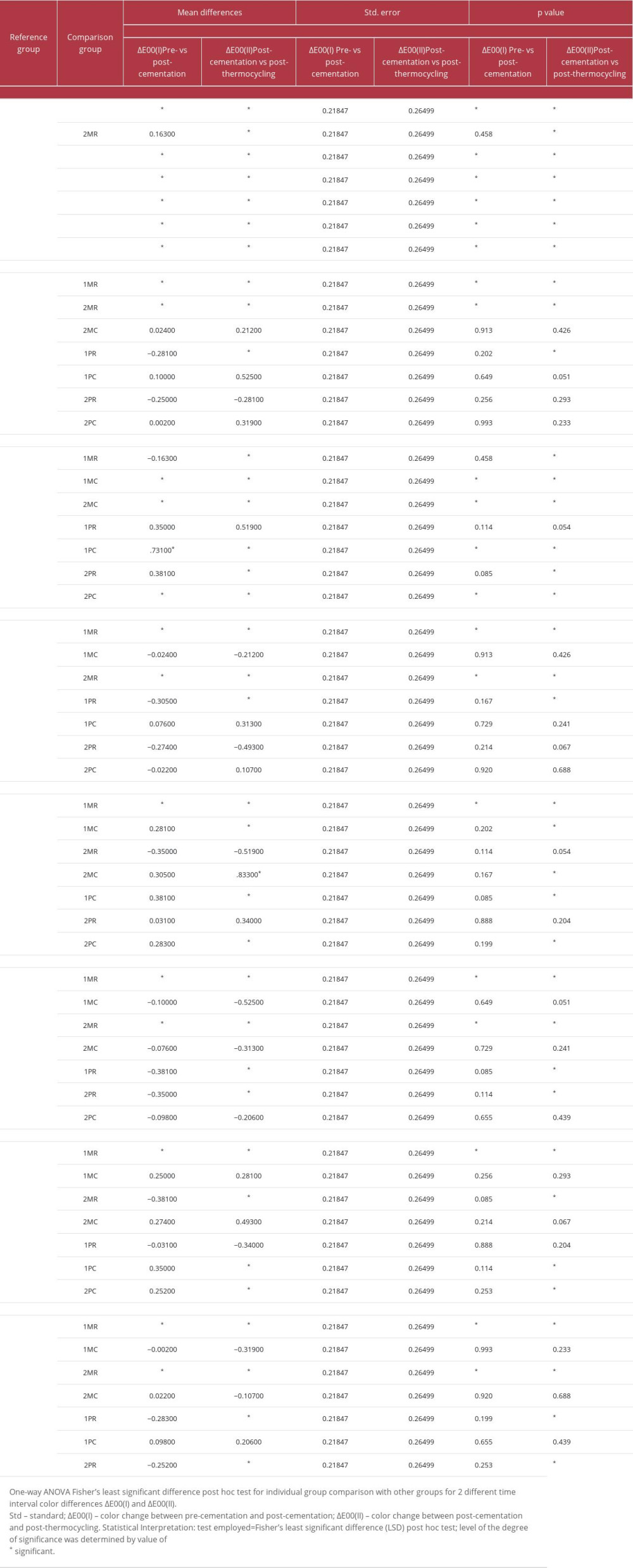
References
1. Bergam B, Nilson H, Andersson M, A longitudinal clinical study of Procera ceramic-veneered titanium copings: Int J Prosthodont, 1999; 12; 135-39
2. Galluci GO, Grütter L, Nedir R, Esthetic outcomes with porcelain-fused-to-ceramic and all-ceramic single-implant crowns: A randomized clinical trial: Clin Oral Implants Res, 2011; 22; 62-69
3. Heydecke G, Locker D, Awad MA, Oral and general health-related quality of life with conventional and implant dentures: Community Dent Oral Epidemiol, 2003; 31(3); 161-68
4. Goiato MC, Santos DM, Haddad MF, Pesqueira AA, Effect of accelerated aging on the microhardness and color stability of flexible resins for dentures: Braz Oral Res, 2010; 24; 114-19
5. Sham AS, Chu FC, Chai J, Chow TW, Color stability of provisional prosthodontic materials: J Prosthet Dent, 2004; 91; 447-52
6. Singh Y, Brar A, Mattoo KA, Clinical reliability of different facial measurements in determining vertical dimension of occlusion in dentulous and edentulous subjects: Int J Prosthodont Restor Dent, 2017; 4(3); 68-77
7. Allen EP, Surgical crown lengthening for function and esthetics: Dent Clin N Am, 1993; 37(2); 163-79
8. Regish KM, Sharma D, Prithviraj DR, Techniques of fabrication of provisional restoration: An overview: Int J Dent, 2011; 2011; 134659
9. ¸akmak G, Cuellar AR, Treviño Santos A, Color and translucency of milled polymethyl methacrylate crowns on non-tooth-colored interim abutments with different surface treatments: J Prosthet Dent, 2022 [Online ahead of print]
10. Yadav LA, Mattoo KA, Kapoor AD, Shuja SA, Factors associated with post core correction of malpositioned teeth: Int J Res Med Sci Tech, 2015; 1(2); 5-7
11. Balkenhol M, Köhler H, Orbach K, Wöstmann B, Fracture toughness of cross-linked and non-cross-linked temporary crown and fixed partial denture materials: Dent Mater, 2009; 25(7); 917-28
12. Karaman T, Eser B, Altintas E, Atala MH, Evaluation of the effects of finish line type and width on the fracture strength of provisional crowns: Odontology, 2021; 109; 76-81
13. Rezaie F, Farshbaf M, Dahri M, 3D printing of dental prostheses: Current and emerging applications: J Compos Sci, 2023; 7(2); 80
14. Srinivasan M, Kalberer N, Kamnoedboon P, CAD-CAM complete denture resins: An evaluation of biocompatibility, mechanical properties, and surface characteristics: J Dent, 2021; 114; 103785
15. Tahayeri A, Morgan M, Fugolin AP, 3D printed versus conventionally cured provisional crown and bridge dental materials: Dent Mater, 2018; 34(2); 192-200
16. Al-Dwairi ZN, Al Haj Ebrahim AA, Baba NZ, A Comparison of the surface and mechanical properties of 3D printable denture-base resin material and conventional polymethylmethacrylate (PMMA): J Prosthod, 2023; 32(1); 40-48
17. Di Fiore A, Meneghello R, Brun P, Comparison of the flexural and surface properties of milled, 3D-printed, and heat polymerized PMMA resins for denture bases: An in vitro study: J Prosthodont Res, 2022; 66(3); 502-8
18. Al-Qarni FD, Goodacre CJ, Kattadiyil MT, Stainability of acrylic resin materials used in CAD-CAM and conventional complete dentures: J Prosthet Dent, 2020; 123(6); 880-87
19. Gruber S, Kamnoedboon P, Özcan M, Srinivasan M, CAD/CAM complete denture resins: An in vitro evaluation of color stability: J Prosthod, 2021; 30(5); 430-39
20. Elagra MI, Rayyan MR, Alhomaidhi MM, Color stability and marginal integrity of interim crowns: An in vitro study: Eur J Dent, 2017; 11; 330-34
21. Song SY, Shin YH, Lee JY, Shin SW, Color stability of provisional restorative materials with different fabrication methods: J Adv Prosthodont, 2020; 12; 259-64
22. Alt V, Hannig M, Wöstmann B, Balkenhol M, Fracture strength of temporary fixed partial dentures: CAD/CAM versus directly fabricated restorations: Dent Mater, 2011; 27(4); 339-47
23. Alp G, Murat S, Yilmaz B, Comparison of flexural strength of different CAD/CAM PMMA-based polymers: J Prosthodont, 2019; 28(2); e491-e95
24. Joshi N: Physical and optical properties of provisional crown and bridge materials fabricated using CAD/CAM milling or 3D printing technology, 2019, Fort Lauderdale, FL, USA, Nova Southeastern University
25. Turgut S, Bagis B, Effect of resin cement and ceramic thickness on final color of laminate veneers: An in vitro study: J Prosthet Dent, 2013; 109(3); 179-86
26. Moecke SE, Silva AG, Borges AB, Torres CR, Optical properties of esthetic temporary cements and final restoration color: J Am Dent Assoc, 2023; 154(6); 461-70
27. Dede DÖ, Armaganci A, Ceylan G, Influence of abutment material and luting cements color on the final color of all ceramics: Acta Odontol Scand, 2013; 71; 1570-78
28. Abdullah AO, Tsitrou EA, Pollington S, Comparative in vitro evaluation of CAD/CAM vs conventional provisional crowns: J Appl Oral Sci, 2016; 24(3); 258-63
29. Güth JF, Kauling AEC, Ueda K, Transmission of light in the visible spectrum (400–700 nm) and blue spectrum (360–540 nm) through CAD/CAM polymers: Clin Oral Investig, 2016; 20; 2501-6
30. Perea-Lowery L, Gibreel M, Vallittu PK, Lassila LV, 3D-printed vs. heat-polymerizing and autopolymerizing denture base acrylic resins: Materials (Basel), 2021; 14; 5781
31. Bucciarelli A, Paolelli X, De Vitis E, VAT photopolymerization 3D printing optimization of high aspect ratio structures for additive manufacturing of chips towards biomedical applications. Addit: Manuf, 2022; 60; 103200
32. Faul F, Erdfelder E, Lang AG, Buchner A, G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences: Behav Res Methods, 2007; 39(2); 175-91
33. Dayan C, Kiseri B, Gencel B, Wear resistance and microhardness of various interim fixed prosthesis materials: J Oral Sci, 2019; 61(3); 447-53
34. Alp G, Johnston WM, Yilmaz B, Optical properties and surface roughness of prepolymerized poly (methyl methacrylate) denture base materials: J Prosthet Dent, 2019; 121; 347-52
35. Lepe X, Bales DJ, Johnson GH, Retention of provisional crowns fabricated from two materials with the use of four temporary cements: J Prosthet Dent, 1999; 81(4); 469-75
36. Reeponmaha T, Angwaravong O, Angwarawong T, Comparison of fracture strength after thermomechanical aging between provisional crowns made with CAD/CAM and conventional method: J Adv Prosthodont, 2020; 12; 218-24
37. Gupta S, Sayed ME, Gupta B, Comparison of composite resin (Duo-Shade) shade guide with vita ceramic shades before and after chemical and autoclave sterilization: Med Sci Monit, 2023; 29; e940949
38. CIE (Commission Internationale de l’Eclairage): Technical report: colorimetry, 2018; 16-20, Vienna, Austria, CIE Central Bureau CIE Pub no 15-4
39. Paravina RD, Ghinea R, Herrera LJ, Color difference thresholds in dentistry: J Esthet Restor Dent, 2015; 27; 1-9
40. Salas M, Lucena C, Herrera LJ, Translucency thresholds for dental materials: Dent Mater, 2018; 34(8); 1168-74
41. Al Moaleem MM, Alkhayrat FM, Madkhali HA, Subjective differences between dentists and patients about relative quality of metal ceramic restorations placed in the esthetic zone: J Contemp Dent Pract, 2017; 18(2); 112-16
42. Mittal N, Khosla A, Jain S, Effect of storage media on the flexural strength of heat and self cure denture base acrylic resins – an invitro study: Ann Romanian Soc Cell Biol, 2021; 11743-50
43. Capa N, Tuncel I, Tak O, Usumez A, The effect of luting cement and titanium base on the final color of zirconium oxide core material: J Prosthod, 2017; 26(2); 136-40
44. Dehno SM, Giti R, Kalantari MH, Mohammadi F, The effects of provisional resin cements on the color and retentive strength of all-ceramic restorations cemented on customized zirconia abutments: PLoS One, 2022; 17(1); e0262582
45. Nayar S, Aruna U, Bhat WM, Enhanced aesthetics with all ceramic’s restoration: J Pharm Bioallied Sci, 2015; 7(Suppl 1); S282
46. Rayyan MM, Aboushelib M, Sayed NM, Comparison of interim restorations fabricated by CAD/CAM with those fabricated manually: J Prosthet Dent, 2015; 114; 414-19
47. Arslan M, Murat SE, Alp G, Zaimoglu A, Evaluation of flexural strength and surface properties of prepolymerized CAD/CAM PMMA-based polymers used for digital 3D complete dentures: Int J Comput Dent, 2018; 21(1); 31-40
48. Alfouzan AF, Alotiabi HM, Labban N, Color stability of 3D-printed denture resins: Effect of aging, mechanical brushing and immersion in staining medium: J Adv Prosthodont, 2021; 13(3); 160
49. Astudillo-Rubio D, Delgado-Gaete A, Bellot-Arcís C, Mechanical properties of provisional dental materials: A systematic review and meta-analysis: PLoS One, 2018; 13(2); e0193162
50. Shin JW, Kim JE, Choi YJ, Evaluation of the color stability of 3D-printed crown and bridge materials against various sources of discoloration: An in vitro study: Materials, 2020; 13(23); 5359
51. Berli C, Thieringer FM, Sharma N, Comparing the mechanical properties of pressed, milled, and 3D-printed resins for occlusal devices: J Prosthet Dent, 2020; 124(6); 780-86
52. Ayman AD, The residual monomer content and mechanical properties of CAD\CAM resins used in the fabrication of complete dentures as compared to heat cured resins: Electron Physician, 2017; 9(7); 4766
53. Bartoloni JA, Murchison DF, Wofford DT, Sarkar NK, Degree of conversion in denture base materials for varied polymerization techniques: J Oral Rehabil, 2000; 27; 488-93
54. Ferracane JL, Hygroscopic and hydrolytic effects in dental polymer networks: Dent Mater, 2006; 22; 211-22
55. Yao Q, Morton D, Eckert GJ, Lin W-S, The effect of surface treatments on the color stability of CAD-CAM interim fixed dental prostheses: J Prosthet Dent, 2020; 126(2); 248-53
56. Dizon JR, Gache CC, Cascolan HM, Post-processing of 3D-printed polymers: Technol, 2021; 9(3); 61
57. Alikhasi M, Jafarian Z, Additional manufactured interim restorations: A review on the literature: J Dent, 2022; 23(4); 424-37
58. Aati S, Akram Z, Ngo H, Fawzy AS, Development of 3D printed resin reinforced with modified ZrO2 nanoparticles for long-term provisional dental restorations: Dent Mater, 2021; 37(6); e360-74
59. Gad MM, Al-Harbi FA, Akhtar S, Fouda SM, 3D-printable denture base resin containing SiO2 nanoparticles: An in vitro analysis of mechanical and surface properties: J Prosthodont, 2022; 31(9); 784-90
60. Kolb C, Gumpert K, Wolter H, Sextl G, Highly translucent dental resin composites through refractive index adaption using zirconium dioxide nanoparticles and organic functionalization: Dent Mater, 2020; 36(10); 1332-42
61. Revilla-León M, Meyers MJ, Zandinejad A, Özcan M, A review on chemical composition, mechanical properties, and manufacturing work flow of additively manufactured current polymers for interim dental restorations: J Esthet Restor Dent, 2019; 31(1); 51-57
62. Değer Y, Bakır M, Demirci F, Deveci B, Color stability of provisional restorative materials in different mouthwash solutions: Adv Mater Sci Eng, 2022; 17
63. Luo MR, Cui G, Rigg B, The development of the CIE 2000 colour-difference formula: CIEDE2000: Color Res Appl.: Endorsed by Inter-Society Color Council, The Colour Group (Great Britain), Canadian Society for Color, Color Science Association of Japan, Dutch Society for the Study of Color, The Swedish Colour Centre Foundation, Colour Society of Australia, Centre Français de la Couleur, 2001; 26(5); 340-50
64. Sharma G, Wu W, Dalal EN, The CIEDE2000 color-difference formula: Implementation notes, supplementary test data, and mathematical observations: Color Res Appl, 2005; 30; 21-30
65. Ghinea R, Pérez MM, Herrera LJ, Color difference thresholds in dental ceramics: J Dent, 2010; 38; e57-e64
66. Ren J, Lin H, Huang Q, Zheng G, Determining color difference thresholds in denture base acrylic resin: J Prosthet Dent, 2015; 114; 702-8
67. Saltzman Billmeyer: Principles of color technology, 2019; 57-63, Hoboken, NJ, Wiley
68. Vichi A, Ferrari M, Davidson CL, Influence of ceramic and cement thickness on the masking of various types of opaque posts: J Prosthet Dent, 2000; 83(4); 412-17
69. Lee YK, Translucency of human teeth and dental restorative materials and its clinical relevance: J Biomed Opt, 2015; 20; 45002
Figures
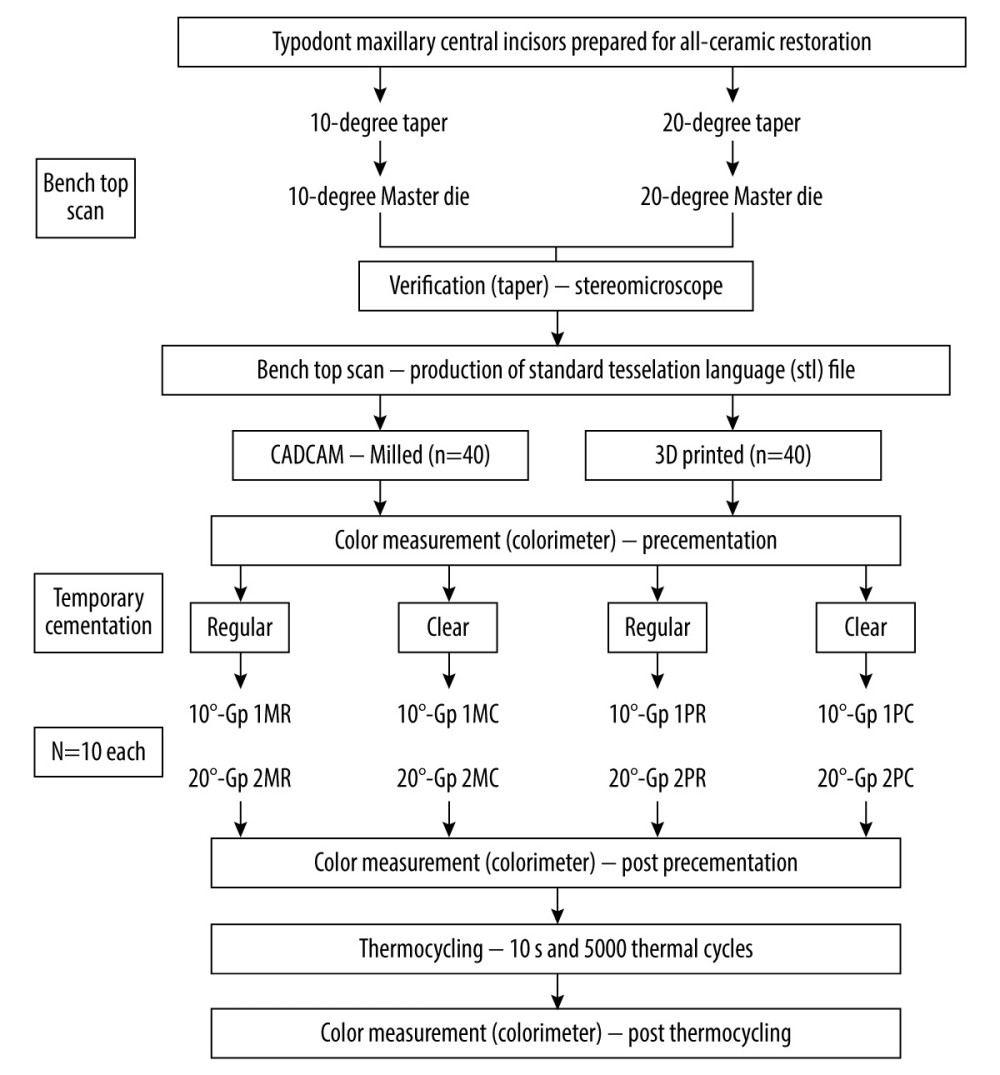 Figure 1. Flowchart showing study sampling and group distribution. Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corp.).
Figure 1. Flowchart showing study sampling and group distribution. Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corp.).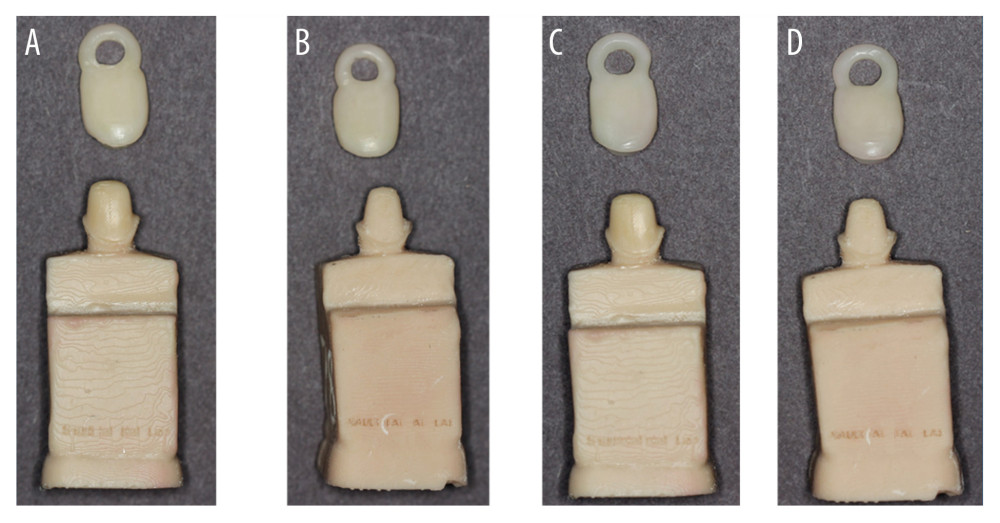 Figure 2. Working models (A) 10° taper milled crowns (B) 20° taper milled crowns (C) 10° taper 3D printed crowns, (D). 20° taper 3D printed crowns. Figure edited and labelled using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corp.).
Figure 2. Working models (A) 10° taper milled crowns (B) 20° taper milled crowns (C) 10° taper 3D printed crowns, (D). 20° taper 3D printed crowns. Figure edited and labelled using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corp.).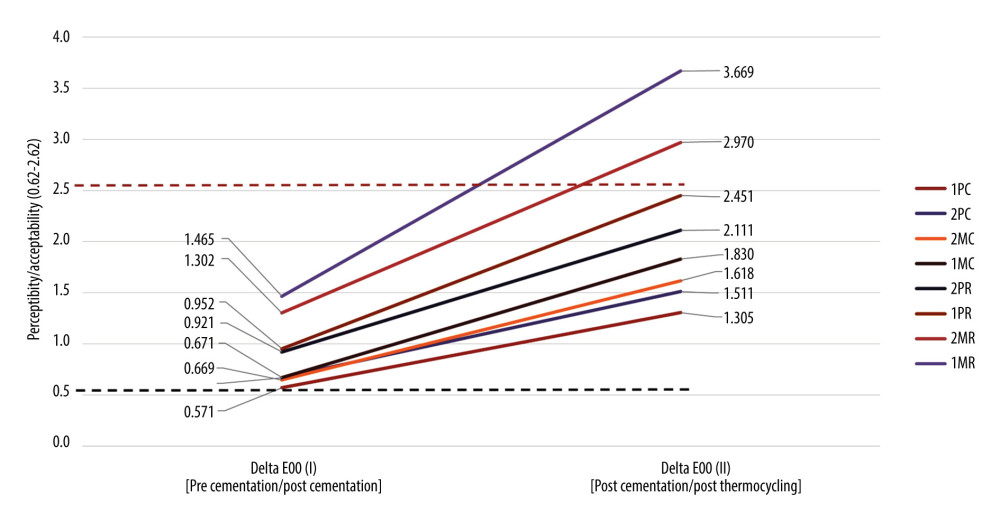 Figure 3. Graphic presentation of mean values for color differences ΔE00(I) (pre- and post-cementation) and ΔE00(II) (post-cementation and post-thermocycling) among studied groups (ascending order of noted color changes among 2 time intervals). Figure created using MS Excel sheet, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corp).
Figure 3. Graphic presentation of mean values for color differences ΔE00(I) (pre- and post-cementation) and ΔE00(II) (post-cementation and post-thermocycling) among studied groups (ascending order of noted color changes among 2 time intervals). Figure created using MS Excel sheet, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corp). Tables
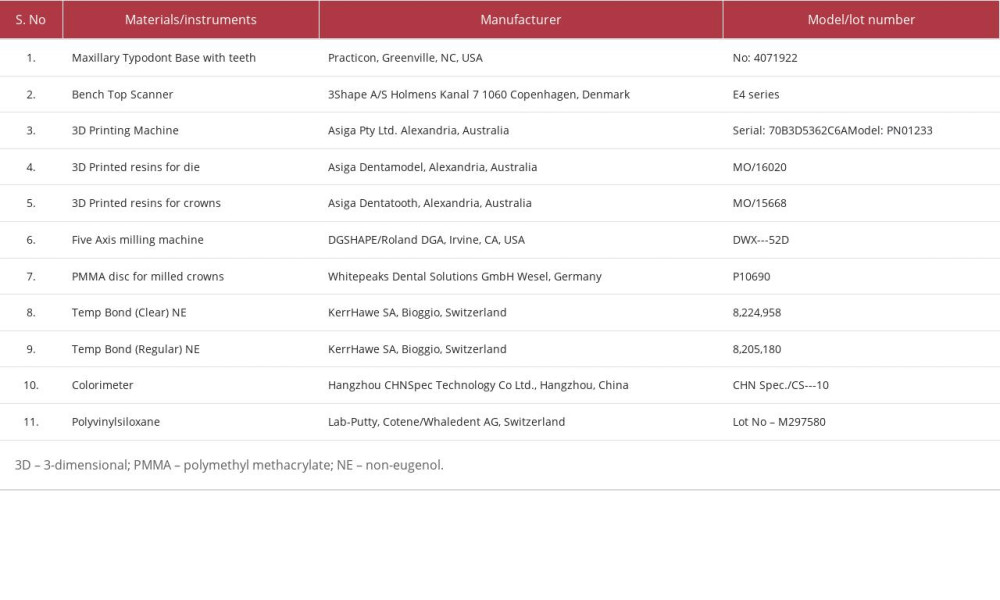 Table 1. List of materials, instrumentation, and manufacturers.
Table 1. List of materials, instrumentation, and manufacturers.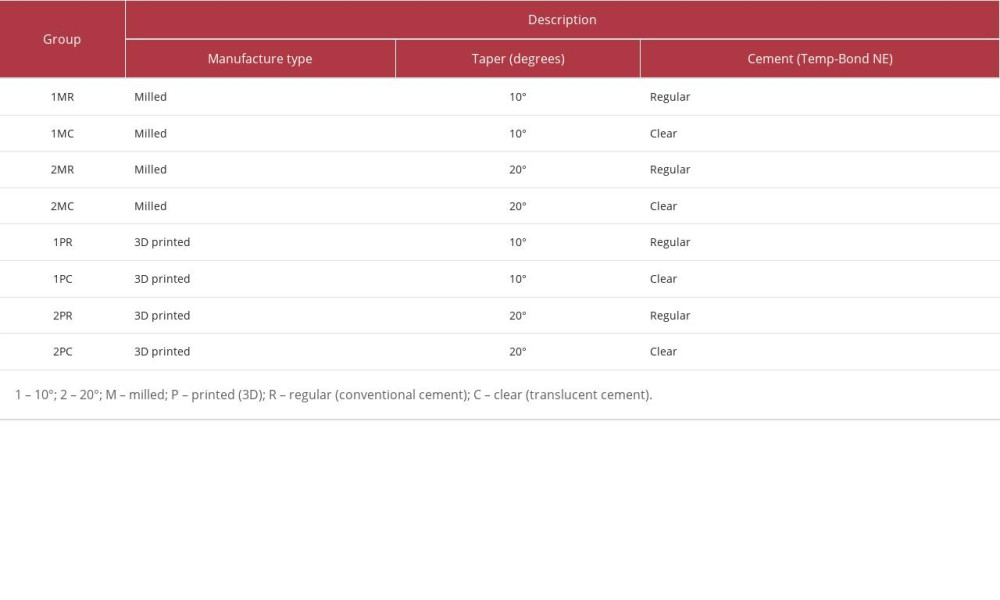 Table 2. Group distribution based on manufacturing, degree of taper, and provisional cement used.
Table 2. Group distribution based on manufacturing, degree of taper, and provisional cement used.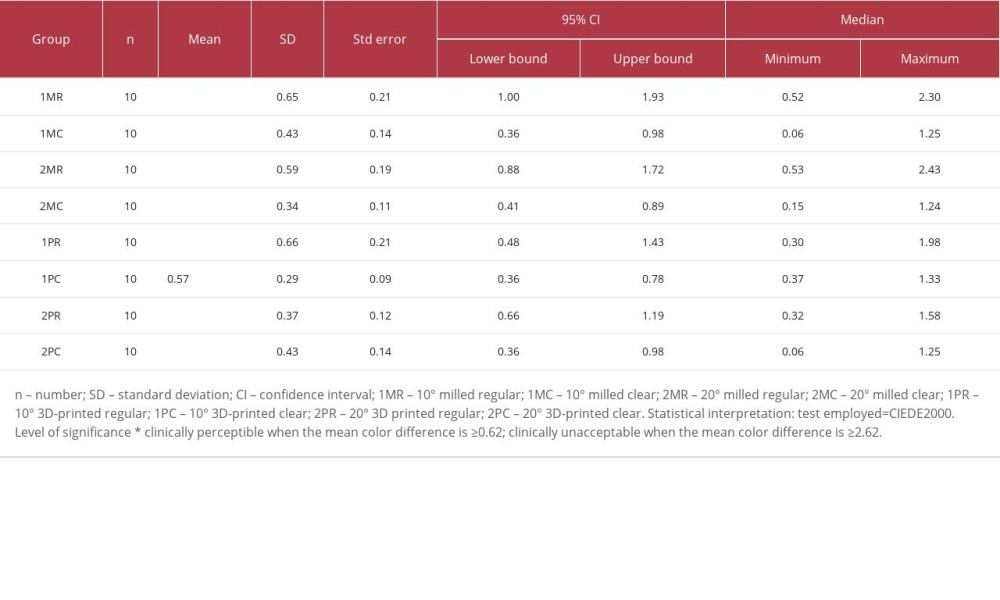 Table 3. Descriptive analysis of the color change ΔE00(I) before cementation and after cementation reported with 95% confidence intervals, mean±SD, and median (minimum, maximum).
Table 3. Descriptive analysis of the color change ΔE00(I) before cementation and after cementation reported with 95% confidence intervals, mean±SD, and median (minimum, maximum).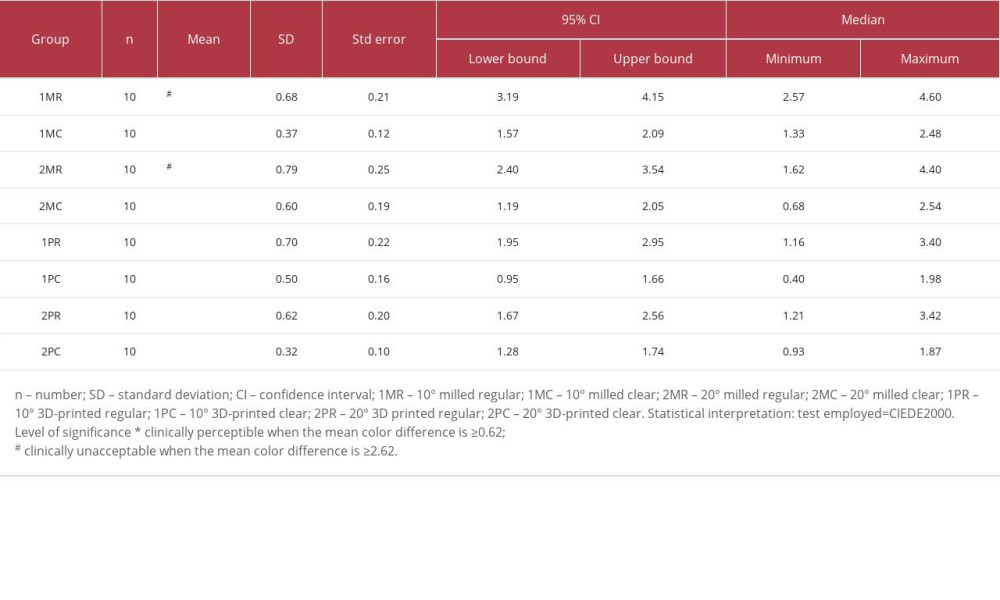 Table 4. Descriptive analysis of the color change ΔE00(II) after cementation and after thermocycling reported with 95% confidence interval, mean±SD, and median (minimum, maximum).
Table 4. Descriptive analysis of the color change ΔE00(II) after cementation and after thermocycling reported with 95% confidence interval, mean±SD, and median (minimum, maximum).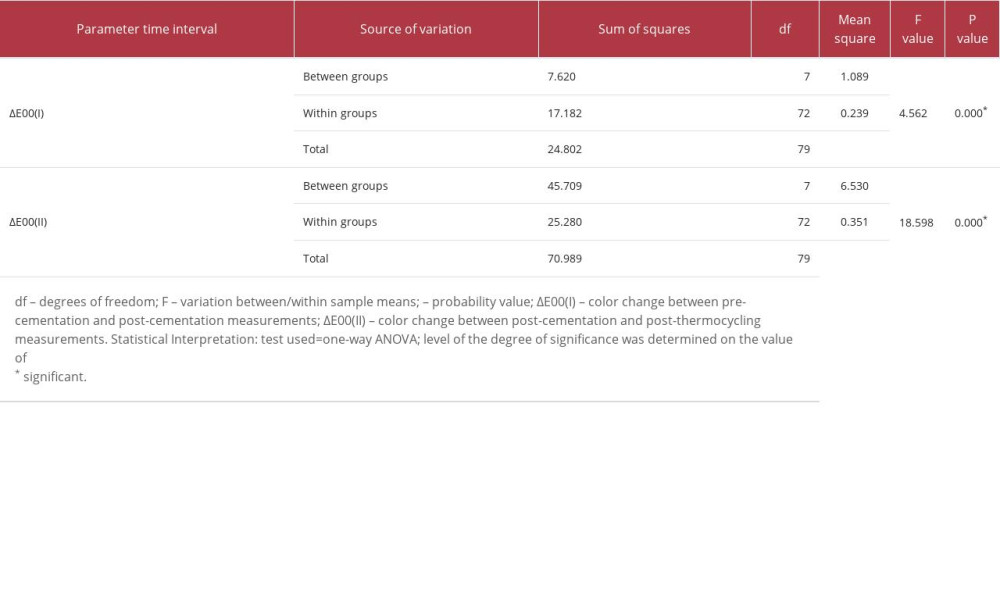 Table 5. One-way ANOVA for comparison of color differences (between and within) observed among studied groups.
Table 5. One-way ANOVA for comparison of color differences (between and within) observed among studied groups.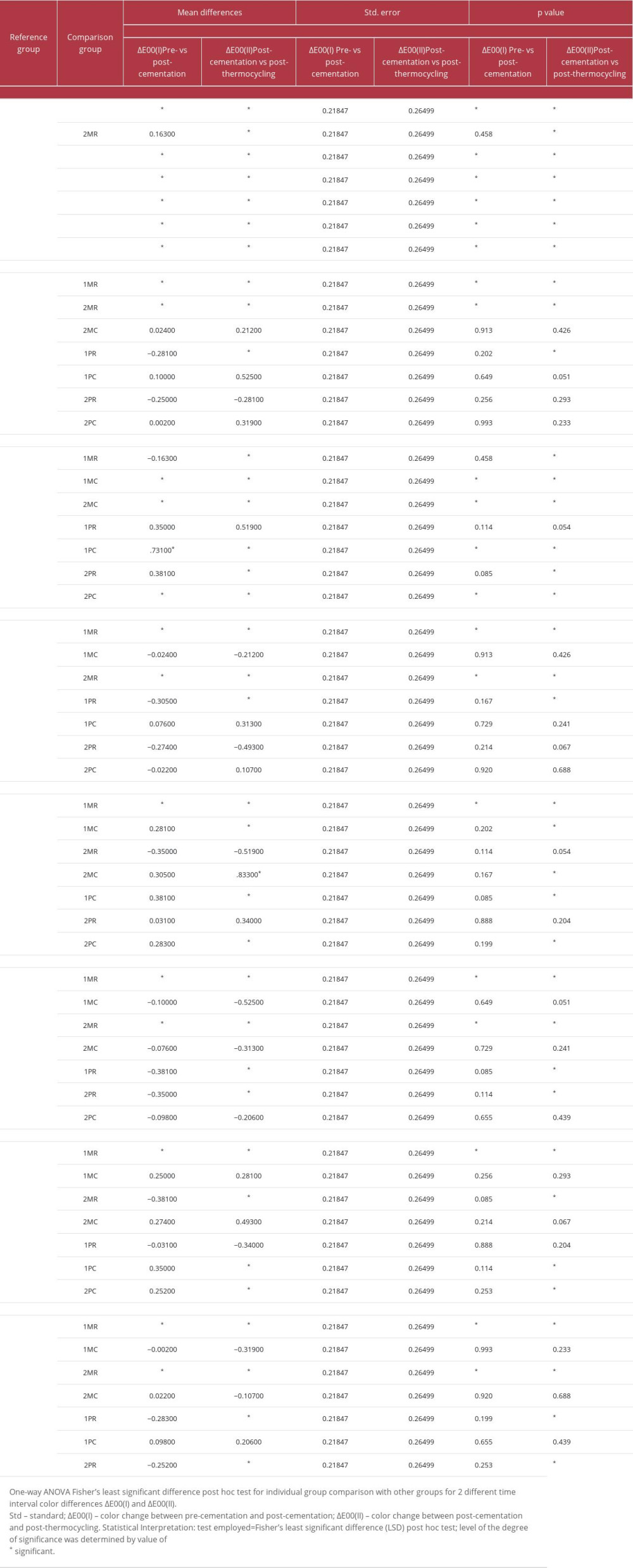 Table 6. One-way ANOVA Fisher’s least significant difference post hoc test for individual group comparison with other groups for 2 different time interval color differences ΔE00(I) and ΔE00(II).
Table 6. One-way ANOVA Fisher’s least significant difference post hoc test for individual group comparison with other groups for 2 different time interval color differences ΔE00(I) and ΔE00(II).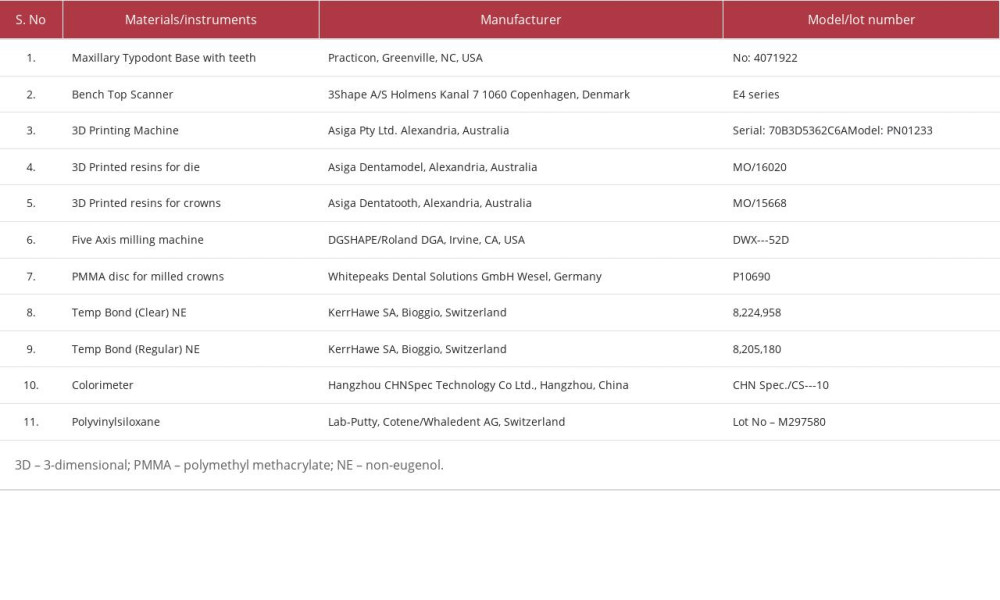 Table 1. List of materials, instrumentation, and manufacturers.
Table 1. List of materials, instrumentation, and manufacturers.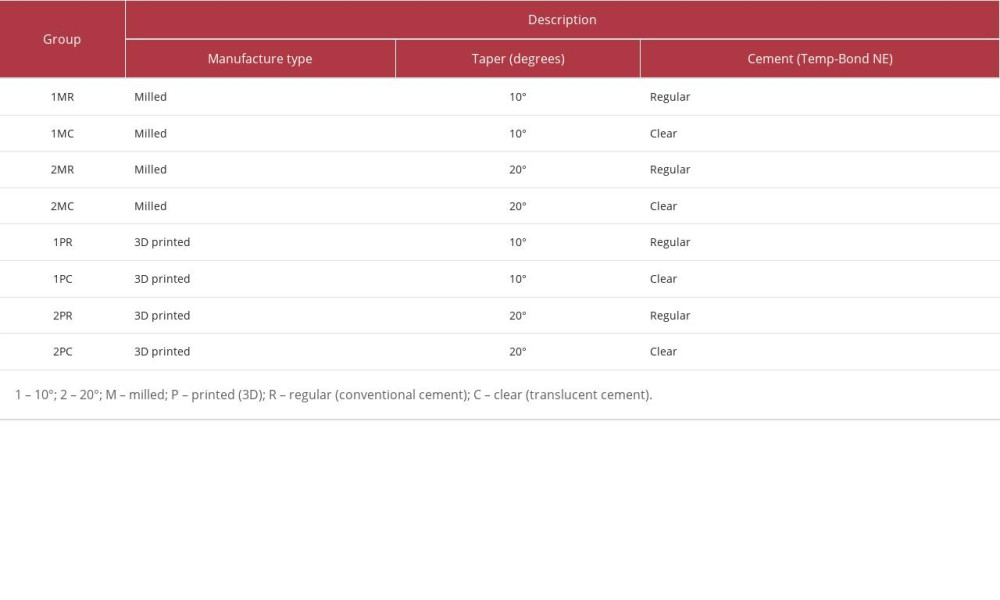 Table 2. Group distribution based on manufacturing, degree of taper, and provisional cement used.
Table 2. Group distribution based on manufacturing, degree of taper, and provisional cement used.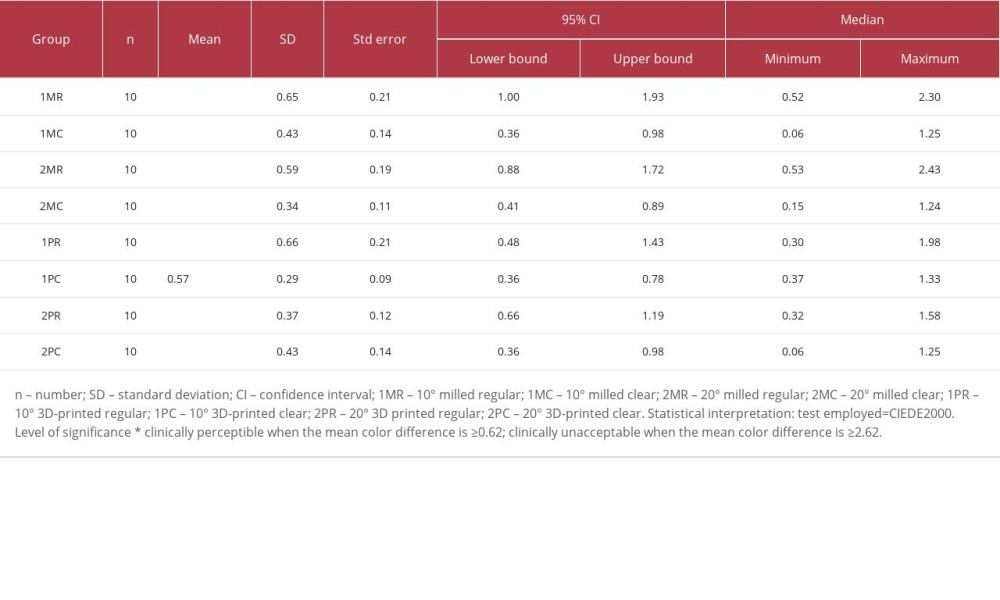 Table 3. Descriptive analysis of the color change ΔE00(I) before cementation and after cementation reported with 95% confidence intervals, mean±SD, and median (minimum, maximum).
Table 3. Descriptive analysis of the color change ΔE00(I) before cementation and after cementation reported with 95% confidence intervals, mean±SD, and median (minimum, maximum).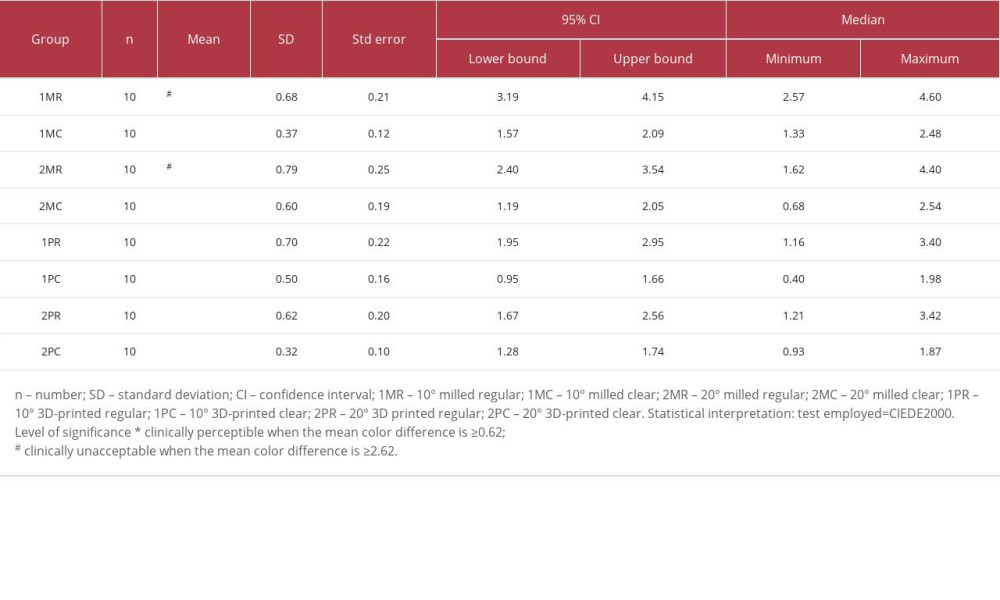 Table 4. Descriptive analysis of the color change ΔE00(II) after cementation and after thermocycling reported with 95% confidence interval, mean±SD, and median (minimum, maximum).
Table 4. Descriptive analysis of the color change ΔE00(II) after cementation and after thermocycling reported with 95% confidence interval, mean±SD, and median (minimum, maximum).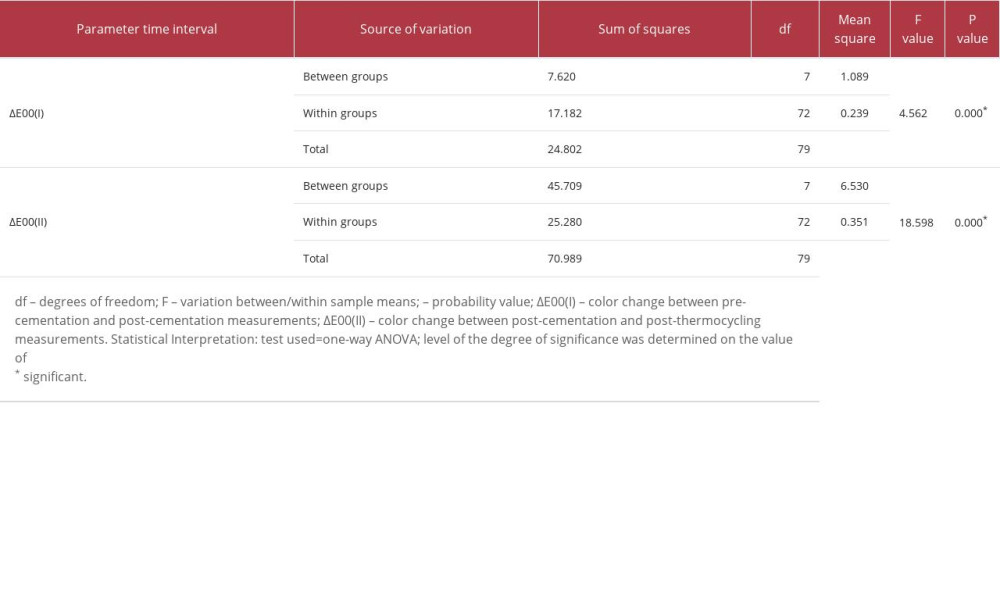 Table 5. One-way ANOVA for comparison of color differences (between and within) observed among studied groups.
Table 5. One-way ANOVA for comparison of color differences (between and within) observed among studied groups.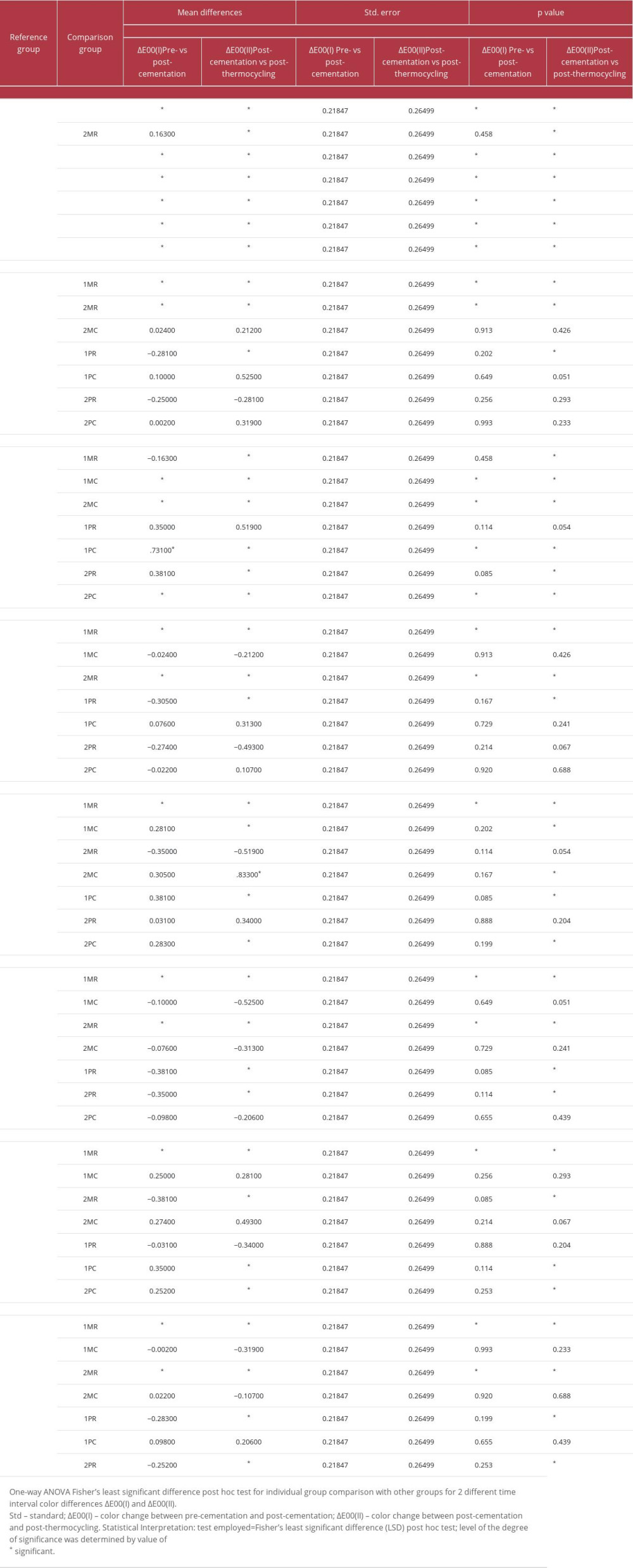 Table 6. One-way ANOVA Fisher’s least significant difference post hoc test for individual group comparison with other groups for 2 different time interval color differences ΔE00(I) and ΔE00(II).
Table 6. One-way ANOVA Fisher’s least significant difference post hoc test for individual group comparison with other groups for 2 different time interval color differences ΔE00(I) and ΔE00(II). Most Viewed Current Articles
15 Jun 2022 : Clinical Research
Evaluation of Apical Leakage After Root Canal Obturation with Glass Ionomer, Resin, and Zinc Oxide Eugenol ...DOI :10.12659/MSMBR.936675
Med Sci Monit Basic Res 2022; 28:e936675
07 Jul 2022 : Laboratory Research
Cytotoxicity, Apoptosis, Migration Inhibition, and Autophagy-Induced by Crude Ricin from Ricinus communis S...DOI :10.12659/MSMBR.936683
Med Sci Monit Basic Res 2022; 28:e936683
01 Jun 2022 : Laboratory Research
Comparison of Sealing Abilities Among Zinc Oxide Eugenol Root-Canal Filling Cement, Antibacterial Biocerami...DOI :10.12659/MSMBR.936319
Med Sci Monit Basic Res 2022; 28:e936319
08 Dec 2022 : Original article
Use of Estimated Glomerular Filtration Rate and Urine Albumin-to-Creatinine Ratio Based on KDIGO 2012 Guide...DOI :10.12659/MSMBR.938176
Med Sci Monit Basic Res 2022; 28:e938176